Management
Subtopic:
Key Government Policies

A policy can be understood as a detailed set of principles or rules designed to guide actions and decisions in a consistent direction.
A key government policy is a formal declaration or set of declarations from a government that defines the intended path for its operations and activities. It reflects the priorities and values of the population it serves and acts as a compass for current and future governmental actions.
Government policies are created to tackle specific problems, needs, or objectives within society. They often span multiple sectors and involve various groups and individuals who have a stake in the issue.
These policies can encompass a broad spectrum of domains, including but not limited to: public health, education, economic growth, environmental conservation, social support systems, and more. They act as a blueprint for governmental decision-making, resource distribution, and the execution of programs and initiatives.
Examples of Key Government Policies in the Realm of Health
Here are some examples of vital government policies focused on health:
National Health Strategy (Revised in 1999 & 2010): This overarching strategy establishes the broad vision, objectives, fundamental principles, and methods for the health sector nationwide. It offers direction on areas such as how health services are delivered, funded, staffed, and developed in terms of infrastructure. The core goal is to improve the overall health of the population by ensuring fair access to good quality healthcare, empowering communities to take charge of their health, and reducing health inequalities. It places emphasis on essential primary care, preventing illness, and promoting healthy living.
National Framework for Health Public-Private Partnerships (Established in 2012): This framework promotes cooperation between the government and private organizations to strengthen the healthcare system. It intends to leverage the strengths of both government and private entities to broaden healthcare access, enhance service quality, and improve efficiency. The policy outlines the structure for these partnerships, clarifying roles, responsibilities, and methods for tracking progress and evaluating impact.
National Strategy to Combat HIV and AIDS (Uganda, 2011): This strategy offers a comprehensive approach to fighting HIV and AIDS within the country. It emphasizes prevention efforts, access to treatment, provision of care, and support systems for individuals and communities affected by the epidemic.
Guidelines for Preventing Mother-to-Child HIV Transmission (Issued in 2006): These guidelines are aimed at minimizing the transmission of HIV from mothers to their infants during pregnancy, childbirth, and breastfeeding. They detail effective measures, such as antiretroviral drug therapy and counseling services.
Operational Guidelines for Private Wings in Public Health Facilities (Issued in 2010): These guidelines regulate how private patient care units are set up and run within government-owned health facilities. They are designed to uphold quality standards, ensure ethical practices, and maintain accountability in the delivery of these healthcare services.
National Policy on Safe Male Circumcision (Adopted in 2010): This policy promotes safe male circumcision as a significant strategy for HIV prevention. It details the required procedures, training for providers, and quality control measures for circumcision services.
National HIV Counseling and Testing Policy (Uganda, 2011): This policy provides guidance on how to offer voluntary and confidential HIV counseling and testing services. It underscores the importance of obtaining informed consent, protecting confidentiality, and linking individuals to necessary care and support after testing.
Local Government Workplace HIV/AIDS Policy (Established in 2009): This policy addresses the issue of HIV/AIDS within local government workplaces. It focuses on prevention initiatives, raising awareness, and providing support for employees affected by HIV/AIDS. It defines the roles of employers and employees in fostering a supportive and inclusive work environment.
Education Sector Workplace HIV and AIDS Policy (Ministry of Education): This policy seeks to lessen the impact of HIV/AIDS on the education sector. It provides direction on prevention, care, and support for students, teaching staff, and other personnel within educational institutions.
Guidelines for Decentralized HIV/AIDS Coordination (Uganda, 2013): These guidelines are designed to improve the coordination of HIV/AIDS programs and services at the local level. They clarify the roles and responsibilities of various stakeholders, including local health authorities, government bodies, and community-based organizations.
Village Health Team (VHT) Strategy and Operational Framework: These guidelines outline how to effectively engage and utilize Village Health Teams in delivering healthcare at the community level. VHTs are crucial in health education, disease monitoring, and improving access to healthcare, especially in rural areas.
National Health Policy and Health Sector Strategic Plan (HSDP)
The National Health Policy (NHP) and the Health Sector Development Plan (HSDP) are structured by the principles of Uganda’s Constitution of 1995 and the Local Government Act of 1997, which promoted decentralized governance and service provision. They also take direction from the National Health Sector Reform Programme, the National Poverty Eradication Programme, and the Alma Ata Declaration’s vision of “Health for All”.
Mission Statement of the NHP:
“To enable all people in Uganda to achieve a good level of health, thus fostering a healthy and productive life for everyone.”
Objectives of the NHP:
Lower rates of death, illness, and childbirth, and reduce related inequalities.
Guarantee access to a basic package of essential healthcare services for all.
Key Priorities of the NHP:
Controlling Infectious Diseases: Focus on diseases like malaria, STIs/HIV/AIDS, and tuberculosis.
Integrated Child Health Management (IMCI): A comprehensive approach to managing common childhood illnesses.
Sexual and Reproductive Health Rights: Including care during pregnancy and childbirth, family planning options, adolescent reproductive health services, and addressing violence against women.
Broader Public Health Actions: Encompassing vaccinations, environmental health initiatives, health education and awareness campaigns, school health programs, preparedness for epidemics and disasters, nutrition improvements, and eradication efforts for diseases like guinea worm, river blindness, polio, neonatal tetanus, and measles.
Enhancing Mental Health Services: Strengthening the availability and quality of mental healthcare.
Essential Clinical Care: Addressing injuries, non-communicable diseases, disabilities, rehabilitation services, palliative care, and oral/dental health.
Guiding Principles of the NHP:
Primary Health Care (PHC): Using PHC as the core strategy and philosophy for national health advancement.
Equitable Service Distribution: Ensuring health services are fairly available across the entire country.
Cost-Effective, Quality Interventions: Prioritizing healthcare actions that are both affordable and effective in delivering good quality care.
Efficiency and Accountability: Promoting strong management within the health system with clear accountability.
Health Promotion and Community Focus: Emphasizing health education, disease prevention, and empowering communities to take charge of their health.
Addressing Emerging Health Needs: Paying attention to new and growing health challenges, including the healthcare needs of older populations.
Strengthened Partnerships: Building stronger collaborations between the public and private health sectors, NGOs, and traditional medicine practitioners.
Inter-Sectoral Collaboration: Working together across different sectors to improve health outcomes.
Gender-Sensitive Health System: Developing a health system that recognizes and responds to the specific health needs of all genders.
Sustainable Health Financing: Establishing reliable and long-term methods to fund healthcare.
HSDP Priorities:
The government will prioritize health services that are cost-effective and have the biggest positive impact on reducing illness and death rates.
These crucial services include actions to combat: malaria, STIs/HIV/AIDS, tuberculosis, diarrheal illnesses, acute lower respiratory infections, conditions around birth and for mothers, vaccine-preventable childhood diseases, malnutrition, injuries, and physical and mental disabilities.
These priority actions will be incorporated into the Uganda National Minimum Healthcare Package, which will be regularly reviewed and updated.
HEALTH SECTOR DEVELOPMENT PLAN (HSDP)
RATIONALE FOR HSDP:
Local Context:
Serves as a key component of the broader health sector planning structure.
Provides a focused strategic direction for the health sector over the medium term.
Supports the implementation of the National Development Plan (NDP II) and the National Health Policy (NHP II).
Takes direction from the NDP II, which outlines Uganda’s strategic path and development priorities for the medium-term.
Regional Context:
Developed acknowledging the African Union’s Common African Position (CAP).
Stresses the importance of universal and fair access to good quality healthcare, with special attention to vulnerable groups and strengthening health systems.
International Context:
Aligned with Uganda’s global commitments, such as:
Implementing the International Health Regulations.
Following the Ouagadougou Declaration on Primary Health Care and Health Systems.
Participating in International Health Partnerships (IHP+) on improving aid effectiveness.
Working towards the Post-MDG 2015 agenda (UN Sustainable Development Goals).
Upholding international human rights agreements related to health.
STRATEGIC DIRECTION:
A medium-term (5-year) plan designed to guide the health sector in achieving the objectives of NHP II.
AIM:
To realize Uganda Vision 2040’s goal of a healthy and productive population that contributes to economic progress and national development.
STRATEGY:
Implementing the Uganda National Minimum Health Care Package effectively.
Adopting a client-centered approach in healthcare delivery.
Focusing efforts on both the supply and demand aspects of healthcare services.
GOAL:
To accelerate progress towards Universal Health Coverage (UHC), ensuring everyone has access to essential, high-quality health services without facing financial hardship.
GUIDING PRINCIPLES:
Fairness and non-discrimination in service provision.
Community participation and accountability within the health system.
Respecting the right to health, including ensuring services are available, accessible, acceptable, and of good quality.
PRIORITY AREAS OF INTERVENTION:
Promoting health, ensuring environmental health, preventing diseases, and enhancing community health initiatives.
Preventing, managing, and controlling communicable diseases.
Preventing, managing, and controlling non-communicable diseases.
Improving maternal and child health outcomes.
HSDP INVESTMENT FOCUS:
Strengthening health governance and partnerships.
Improving service delivery systems.
Enhancing health information systems.
Ensuring sustainable health financing mechanisms.
Managing health products and technologies effectively.
Developing and supporting the health workforce.
Developing and maintaining health infrastructure.

THE UGANDA’S NATIONAL HEALTH SYSTEM/SECTOR
The World Health Organization (WHO) defines a healthcare system as:
“All activities with the primary goal of promoting, restoring, or maintaining health.”
Essentially, a healthcare system comprises all the people, organizations, and resources that are organized based on established policies. Their collective aim is to improve the health of the population they serve. This involves meeting people’s reasonable expectations for healthcare and safeguarding them from financial hardship when they become ill. This is achieved through a variety of actions primarily intended to enhance health outcomes.
This definition is broad, encompassing both:
Health Actions: Activities directly within the health sector.
Non-Health Actions: Activities outside the traditional health sector that contribute to positive health results.
The World Bank offers an even broader perspective, defining health systems to include interconnected factors impacting health. These extend beyond direct medical services to include elements like poverty levels, education accessibility, infrastructure quality, and the wider socio-political environment.
Effective health systems are crucial for achieving the Sustainable Development Goals (SDGs) by the target year 2030, highlighting their global importance.
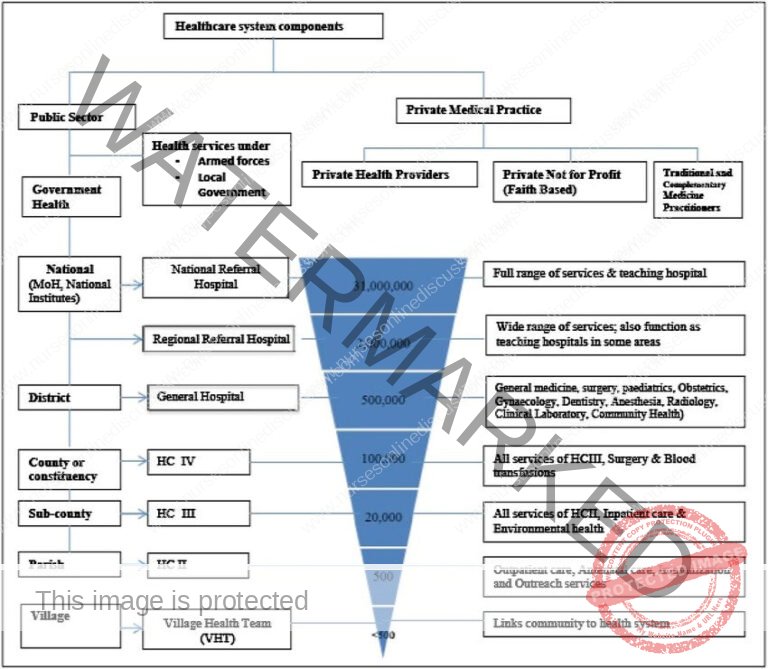
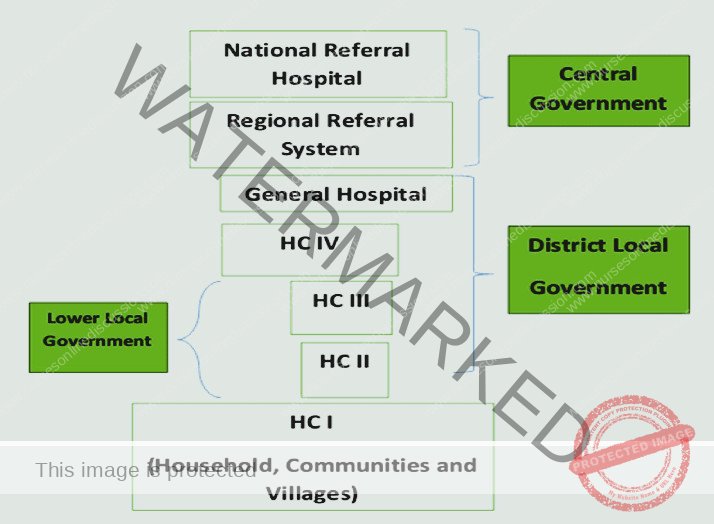
Uganda’s National Healthcare System is structured as a well-organized, decentralized system. Healthcare delivery operates on a referral system, meaning patients are ideally seen at lower levels of care first and referred upwards for more specialized services if needed. Districts and Health Sub-Districts (HSDs) are central to both delivering and managing health services at the local level. The district health structure oversees all facilities within its jurisdiction, with the exception of regional referral hospitals in areas where they exist.
COMPONENTS of the National Health System (NHS):
The NHS in Uganda is composed of two main sectors:
Public Sector:
Encompasses all government-owned health facilities operating under the Ministry of Health (MOH).
Includes health services administered by other government ministries such as:
Ministry of Defence (Military/Army Health Services)
Ministry of Education (School Health Services)
Ministry of Internal Affairs (Police and Prisons Health Services)
Ministry of Local Government (Potentially overseeing health aspects at local levels)
Private Sector:
Private Not-for-Profit (PNFP) Providers: These are often faith-based or NGO-run health facilities that reinvest any surplus into their services rather than distributing profits.
Private Health Practitioners (PHPs): Includes private clinics, hospitals, and individual healthcare providers operating for profit.
Traditional and Complementary Medicine Practitioners (TCMPs): Providers of traditional healing practices and complementary therapies.
PUBLIC HEALTH SECTOR STRUCTURE (Under MOH):
The public health sector, directly managed by the MOH, has a hierarchical structure extending from the national level down to the community:
MOH Headquarters: Central leadership and policy-making body for health in Uganda.
National Services:
National Referral Hospitals (NRHs): Specialized hospitals providing tertiary care and national-level expertise.
Regional Referral Hospitals (RRHPs): Hospitals offering specialized services at the regional level, acting as referral points for districts.
General Hospitals: Provide a broader range of inpatient and outpatient services, typically located at the district level.
District Health Headquarters (District Health Team): Responsible for coordinating and managing health services within the district.
Health Centre (HC) Levels: A tiered system of primary healthcare facilities:
HC IVs: Higher-level health centers offering a wider range of services, including some inpatient care and surgical procedures.
HC IIIs: Provide basic outpatient services, laboratory services, and preventative care.
HC IIs: Primarily focus on basic outpatient care, community health outreach, and some preventative services.
Community Health Services:
Community Health Centers: Smaller facilities located within communities to provide basic health services.
Community Health Workers (CHWs)/Village Health Teams (VHTs-HCIs): Volunteers or trained individuals working at the village and household level to provide health education, basic services, and referrals.
Households: The base level for health promotion and disease prevention efforts, with families and individuals playing a key role in their own health.
MOH HEADQUARTERS AND NATIONAL LEVEL INSTITUTIONS
The main roles of the Ministry of Health (MOH) headquarters include:
Policy Leadership: Analyzing, creating, and discussing health policies.
Strategic Planning: Developing long-term plans for the health sector.
Quality Control: Setting standards and ensuring the quality of health services.
Resource Management: Finding and managing funds for health initiatives.
Inter-Ministerial Advice: Providing health expertise to other government bodies.
Capacity Building: Improving skills and providing technical support to health personnel.
National Service Coordination: Managing nationwide health services, including emergency and epidemic responses.
Research Coordination: Overseeing and promoting health research.
Performance Monitoring: Evaluating the overall effectiveness of the health sector.
National, Regional, and General Hospitals:
General Hospitals: Offer a range of services:
Preventive and health promotion programs.
Treatment for illnesses.
Maternity care.
Inpatient services.
Surgery.
Blood transfusions.
Laboratory and imaging diagnostics.
Clinical support services.
Training and consultations.
Research to support community health programs.
Regional Referral Hospitals: Provide all services of General Hospitals, plus:
Specialized clinical care, including:
Psychiatry.
Ear, Nose, and Throat (ENT) services.
Ophthalmology (eye care).
Advanced surgical and medical treatments.
Comprehensive clinical support services (laboratory, imaging, pathology).
Teaching and research activities.
National Referral Hospitals: Offer the most advanced level of care:
Comprehensive and highly specialized services.
Extensive involvement in health research and medical education.
Provide all services offered by General and Regional Referral Hospitals.
The Ministry of Health and National Level Institutions
The Ministry of Health (MOH) is the central government body responsible for health oversight in Uganda. Its key functions are:
Policy Leadership: Developing, analyzing, and communicating health policies and strategies.
Strategic Planning: Establishing long-term goals and strategic directions for the entire health sector.
Standards and Quality Assurance: Defining and monitoring quality benchmarks for health services to ensure safety and effectiveness.
Resource Mobilization: Securing and allocating financial and other resources necessary for health programs.
Inter-Agency Consultation: Advising other government ministries, departments, and agencies on health-related issues and policies.
Capacity Development & Supervision: Providing training, support, and oversight to enhance the skills and knowledge of health workers.
Nationally Coordinated Services: Managing and coordinating national health initiatives, including emergency preparedness, outbreak response, and disease control at a national scale.
Research Coordination: Facilitating, supporting, and guiding health research efforts across the country.
Health Sector Performance Monitoring & Evaluation: Tracking progress, assessing impact, and evaluating the overall performance of the health sector to inform improvements.
National Autonomous Institutions
To improve efficiency and focus, the MOH has delegated specific functions to independent institutions. These include:
Specialized Clinical Services:
Uganda Cancer Institute: Center for specialized cancer treatment and research.
Uganda Heart Institute: Specialized care and research for heart-related conditions.
Specialized Clinical Support Services:
Uganda Blood Transfusion Services (UBTS): Manages the national system for blood collection, testing, and distribution, ensuring a safe blood supply.
Uganda Virus Research Institute: Conducts research focusing on viruses and viral infectious diseases.
National Medical Stores: Responsible for procuring, storing, and distributing essential medicines and medical supplies to public health facilities.
National Public Health Laboratories: Provides essential laboratory services for public health surveillance, disease diagnosis, and monitoring.
Regulatory Bodies / Authorities: These bodies ensure quality and standards within their respective areas:
National Drug Authority: Regulates drugs, ensuring quality, safety, and efficacy of pharmaceuticals on the market.
Medical and Dental Practitioners Council: Regulates medical and dental professionals, ensuring ethical and competent practice.
Allied Health Professional’s Council: Regulates allied health professionals (e.g., physiotherapists, medical lab technicians), maintaining standards in these fields.
Pharmacy Council: Regulates pharmacists and pharmaceutical services, ensuring qualified pharmacy practice.
Nurses and Midwives Council: Regulates nurses and midwives, ensuring professional standards in nursing and midwifery care.
Other National Level Institutions:
Uganda National Research Organisation (UNHRO): Coordinates and promotes national health research activities across various institutions.
Health Service Commission: Responsible for human resource management within the public health sector, including recruitment and management of health personnel.
Uganda AIDS Commission (UAC): Leads and coordinates the national multi-sectoral response to the HIV/AIDS epidemic.
District Health Systems:
Uganda’s constitution (1995) and the Local Government Act (1997) empower Local Governments (LGs) with significant health responsibilities, including:
Local Health Governance: Planning, budgeting, and implementing health policies and sector plans at the district level.
Human Resource Management: Recruiting, deploying, developing, and managing health personnel within district health services.
Local Health Regulations: Creating and enforcing health-related local laws (by-laws) and monitoring overall health sector performance within the district.
Facility Management & Supervision: Managing public general hospitals and Health Centres (HCs), and overseeing all health activities (public and private) within their areas. Public-private partnerships at the district level are still developing.
Health sub-District system (HSDs):
Decentralized Management: HSDs are responsible for planning, organizing, budgeting, and managing health services within their designated sub-district and lower-level health centers.
Oversight Function: HSDs supervise all health activities within their area, including curative, preventive, promotive, and rehabilitative services, regardless of provider type (public, private non-profit, private for-profit).
HSD Headquarters: Typically based at a Health Centre IV or a designated general hospital within the sub-district.
Health centres III, II and village Health Teams (HCI):
Health Centre IIIs (HCIIIs): Offer a broader range of primary care services:
Basic preventive, health promotion, and curative services.
Supervisory support for community health activities and HCIIs.
Basic laboratory services for diagnosis.
Maternity care services.
First-level referral point within the sub-county.
Health Centre IIs (HCIIs): Serve as the initial point of contact with the formal health system for communities, providing:
Outpatient care services.
Community outreach programs.
Links to Village Health Teams (VHTs).
Community Health Services & Village Health Teams (VHTs):
Community Health Extension Workers (CHEWs): Planned role (as per HSDP 2015/016) to train and deploy 15,000 CHEWs across 7,500 parishes, based at community health centers. CHEWs would supervise VHTs.
Village Health Teams (VHTs): Community-based volunteer health workers responsible for the health of designated households/families. Aimed to cover the entire population, with VHTs reporting to trained CHEWs (currently being piloted).
Roles of Village Health Teams (VHTs):
Needs Assessment: Identifying health needs within their communities.
Resource Mobilization: Mobilizing community resources and monitoring their use for health improvements.
Community Mobilization for Health: Encouraging community participation in health programs like immunization, malaria control, sanitation, and promoting health-seeking behaviors.
Household Health Registers: Maintaining records of household members and their health status.
Vital Statistics Recording: Registering births and deaths in their communities.
Community-Health System Link: Serving as the primary connection between communities and formal health providers.
Community-Based Case Management: Managing common childhood illnesses like malaria, diarrhea, and pneumonia at the community level.
Commodity Distribution: Distributing health commodities (e.g., medications, supplies) as needed.
Challenges with VHTs:
Limited Coverage: While VHTs are important, their coverage is not universal.
Training Gaps: As of 2010, while VHTs existed in 75% of districts, only 31% had fully trained VHTs in all villages.
High Attrition: Volunteer nature and lack of consistent compensation led to high dropout rates among VHTs.
The District Health Officer and District Health Management Team
District Health Officer (DHO): A senior medical doctor with management training who leads district health services. Responsible for overall management of district health.
Members of the District Health Management Team (DHMT):
The DHMT typically includes:
District Biostatistician
District Health Educator
District Nursing Officer
District Stores Manager (Medical)
District Cold Chain Manager
District Environmental Health Officer
District Laboratory Focal Person
District Tuberculosis and Leprosy Supervisor
District Vector Control Officer
Heads/In-Charges of Health Sub-Districts (HSDs)
Other members as needed by the DHO
Functions of the District Health Management Team:
District Health Planning: Coordinating all health planning within the district.
Supervision of Health Activities: Regularly visiting and supervising government and private non-profit health facilities, providing guidance and ensuring proper record-keeping. Supervising special health programs (e.g., Immunization, TB/Leprosy control, Family Planning).
Health Personnel Training: Coordinating basic health training programs in the district and managing continuing education for health staff, including community health workers.
Clinical Work: DHO may engage in clinical duties, especially when there are staff shortages.
Health Care Setting Management Positions:
Examples of management roles within health facilities:
Ward In-Charge
Special Clinic In-Charge
Outreach Program Coordinator
Director of Medical Records
Senior/Principal Nursing Officer
Summary: Structure of Health Services in Uganda
The Ugandan health system is structured into an eight-tiered hierarchy, designed to deliver healthcare services effectively across all population levels:
1. Ministry of Health (MOH): The apex body, functioning as the central leadership for health matters in Uganda. Its core duties are:
Policy & Guideline Development: Creating national health policies and operational guidelines.
National Standards Setting: Establishing benchmarks for quality and standards of healthcare delivery throughout the nation.
Financial Resource Management: Securing and allocating funds to support the health sector’s operations and initiatives.
Workforce Capacity Building: Enhancing the skills and capabilities of health professionals through training and development programs.
Technical Oversight & Guidance: Providing expert technical support and supervision to all levels of the health system.
Performance Monitoring & Evaluation: Assessing and tracking the overall effectiveness and impact of the health sector.
Regulatory Compliance: Ensuring adherence to health regulations and standards across all healthcare services.
2. National Referral Hospitals: These hospitals serve a vast population, approximately 30 million citizens, and represent the highest tier of specialized medical care. Their primary roles include:
Highly Specialized Clinical Services: Delivering advanced and intricate medical and surgical treatments for complex conditions.
Specialist Training & Education: Acting as key centers for the education and advanced training of medical specialists.
Advanced Health Research: Conducting cutting-edge research to innovate medical practices and expand health knowledge.
3. Regional Referral Hospitals: Designed to cater to a population of around 2 million per region (typically serving areas of about 3 million people). Their functions encompass:
Specialist Medical & Surgical Care: Providing specialized treatments, although less super-specialized than national hospitals.
Healthcare Professional Training: Participating in the education and training of various healthcare professionals.
Regionally Relevant Research: Conducting health research focused on addressing the specific health challenges and needs of their respective regions.
Referral Hub for Districts: Serving as the main referral point for district hospitals and lower-level facilities within the region.
4. District Hospitals: Typically, each district has a designated hospital serving a population of approximately 500,000. They offer a broad spectrum of general hospital services:
Preventive Health Programs: Initiatives focused on promoting wellness and preventing diseases within the community.
Health Promotion Activities: Efforts to educate and empower communities to adopt healthy behaviors and lifestyles.
Outpatient Clinical Services: Providing general medical consultations and treatments for patients who do not require hospitalization.
Maternity Care Services: Comprehensive services for antenatal care, safe delivery, and postnatal support for mothers and newborns.
Inpatient Hospitalization: Providing care for patients requiring admission and overnight stays for medical treatment.
Emergency Surgical Interventions: Offering immediate surgical care for urgent and life-threatening medical conditions.
Blood Transfusion Services: Ensuring the availability of safe and screened blood for transfusions.
Essential Diagnostic Services: Providing necessary laboratory and medical imaging services for diagnosis and treatment.
General Medical Services: A range of other medical services to address the diverse health needs of the district’s population.
5. Health Sub-Districts (HSDs) & Health Centre IVs (HCIVs): HSDs, each serving roughly 100,000 individuals, are crucial management units. HCIVs function as the main referral centers within these sub-districts. Their responsibilities include:
Local Health Service Management: Planning, organizing, and overseeing the delivery of health services within the designated Health Sub-District.
Technical & Logistical Support: Providing expert guidance, logistical resources, and capacity enhancement for lower-level health facilities and community-based health programs operating within the HSD.
Primary Referral Point: Serving as the main point of referral for Health Centre IIIs, IIs, and community-level services within the HSD network.
HCIV Service Delivery (Government or PNFP): HCIVs themselves offer a range of essential healthcare services:
Fundamental Disease Prevention: Basic preventive measures aimed at reducing the incidence of common diseases.
Curative Treatments: Medical care for treating common illnesses and health conditions.
Rehabilitative Services: Support for patient recovery and functional restoration after illness or injury.
These services are accessible to the immediate local population and to referred patients from lower-tier facilities across the HSD.
6. Health Center 3 (HCIII): Designed to serve a population catchment of approximately 20,000 people, HCIIIs are vital for primary healthcare accessibility. They are tasked with:
Consistent Basic Preventive Care: Providing regular and ongoing basic preventive healthcare services to the community.
Health Promotion Initiatives: Implementing activities to promote healthy behaviors and lifestyles within their service area.
Curative Care for Common Ailments: Offering treatment for prevalent illnesses and health issues at the community level.
Supervisory Support Role: Providing guidance, mentorship, and supervision to community health workers and Health Center II facilities operating within their jurisdiction.
7. Health Center 2 (HCII): Serving smaller communities, around 5,000 individuals, HCIIs are the most readily accessible point of contact with the formal health system for many. Their key function is:
Initial Community-Health Sector Interface: Acting as the primary point of interaction and entry into the structured health system for local populations.
8. Village Health Team (VHT) – (Community Level/Health Centre I equivalent): Serving populations of roughly 1,000, VHTs are deeply rooted in their communities and play a crucial role in:
Community Mobilization & Empowerment: Facilitating community engagement and empowering individuals to take proactive steps to improve their health.
Village-Based Structure: Each village is supported by a VHT, consisting of approximately 9-10 volunteers chosen by village leadership, ensuring community representation and trust in local health initiatives.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

