Gynecological Nursing
Subtopic:
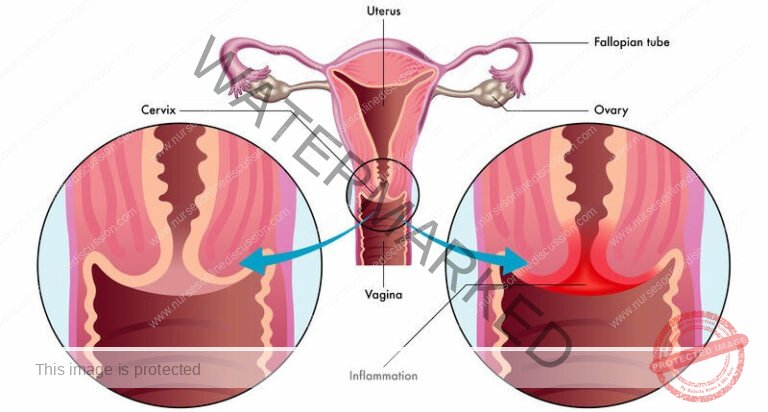
Cervical ectropion (Cervical Erosion)
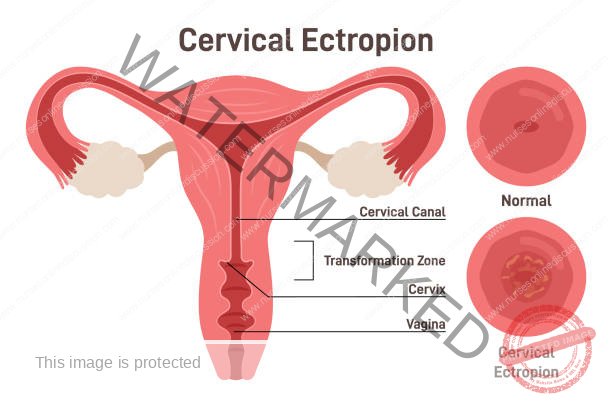
Cervical ectropion describes a condition where the inner lining cells of the cervix are present on the outer surface, creating a reddish area.
This condition, also known as cervical erosion, occurs when the glandular cells normally found inside the cervical canal extend outwards onto the cervix’s exterior.
These glandular cells are naturally red in appearance, which gives the affected area a red or inflamed look. The terms cervical erosion or cervical ectopy are also used to refer to this condition.
It is important to emphasize that cervical ectropion is a non-cancerous (benign) state and does not progress to cervical cancer.
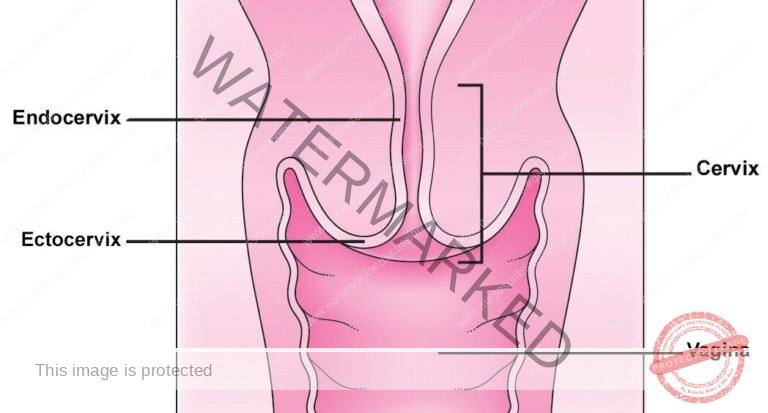
The cervix, the lower part of the uterus, is structured into two main regions: the ectocervix and the endocervical canal.
Endocervical Canal (Endocervix): This is the inner part of the cervix, located closer to the uterus. Its lining consists of simple columnar epithelium, a tissue type that produces mucus.
Ectocervix: This is the outer portion of the cervix that protrudes into the vagina. Typically, it is covered by stratified squamous non-keratinized epithelium, a different type of protective tissue.
Cervical ectropion is characterized by the presence of the endocervical columnar epithelium extending outwards onto the ectocervix. This displacement is thought to be influenced by elevated estrogen levels. It’s crucial to understand that this condition is not metaplasia, meaning it’s not a change in the cell type, but rather a change in the location of the cells.

Etiology
The primary cause of Cervical Ectropion is hormonal fluctuations. Frequently, women using oral contraceptives are observed to have this condition. It is believed that this occurrence is a reaction to elevated estrogen levels within the body. The cells that naturally line the inner cervical canal can migrate and become situated on the external surface of the cervix. This cellular displacement can be visually identified during a speculum examination.
It is generally accepted that cervical ectropion is promoted by high estrogen levels. Consequently, factors that elevate estrogen levels are also considered to increase the likelihood of developing ectropion. These risk factors notably include:
Utilization of combined oral contraceptive pills.
Gestation (Pregnancy).
Adolescent years.
Being within menstruating age (it is less commonly observed in women who have gone through menopause).
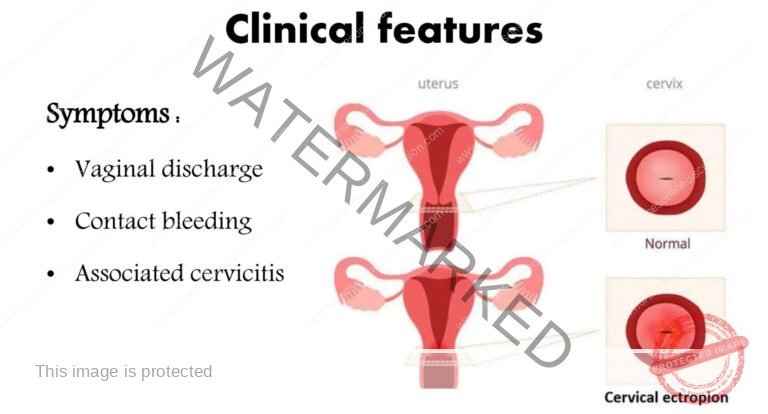
Clinical Features of Cervical Erosion
Cervical ectropion often presents without noticeable symptoms. However, when symptoms do occur, they may include:
Unusual Vaginal Bleeding: Cervical ectropion can manifest as unexpected bleeding from the vagina. This bleeding might occur spontaneously or be triggered by activities such as sexual intercourse. The exposed area of the cervix in ectropion is more delicate and prone to irritation, making it susceptible to bleeding.
Spotting or Blood-Tinged Discharge: Individuals with cervical ectropion may experience spotting between periods or notice a vaginal discharge that is streaked with blood. This occurs because the glandular cells on the outer cervix have fragile blood vessels that can easily break and bleed, even with minor friction.
Bleeding Related to Sexual Activity: Bleeding is commonly reported during or after sexual intercourse. The physical contact and pressure during intercourse can irritate the exposed and sensitive area of the cervix, leading to episodes of bleeding. This bleeding may not be consistent but can be a recurring concern for some individuals.
Exacerbation by Vaginal Infections: The presence of vaginal infections, such as yeast infections (thrush) or bacterial vaginosis, can worsen the symptoms associated with cervical ectropion. These infections can cause further irritation to the already sensitive cervical area, increasing the likelihood of bleeding and discharge.
Asymptomatic Presentation: It is important to note that many individuals with cervical ectropion experience no symptoms at all. In these cases, the condition may only be detected during routine gynaecological examinations, such as during a Pap smear.

Investigations of Cervical Erosion
Diagnosis of cervical erosion/ectropion is primarily clinical, relying on a physical examination. The purpose of further investigations is mainly to exclude other conditions that might present similarly. These investigations may include:
Pregnancy Test: This is performed to eliminate pregnancy as a possible reason for changes observed on the cervix. Ruling out pregnancy is a standard first step in evaluating many gynecological conditions.
Triple Swabs: If there are indications of infection, such as a pus-like discharge, taking endocervical and high vaginal swabs is recommended. (Triple swabs are taken to test for various infections, ensuring comprehensive screening if infection is suspected.)
Cervical Smear (Pap Smear): This test is conducted to exclude cervical intraepithelial neoplasia (CIN), which is a precancerous condition of the cervix. If a suspicious lesion is visually identified during examination, a biopsy might be necessary. (Biopsies are not routinely taken for cervical ectropion, but are crucial if there is concern about more serious conditions like CIN.)

Management of Cervical Erosion
Cervical ectropion is typically harmless and often resolves on its own, meaning treatment is usually unnecessary unless symptoms are bothersome.
Initial Step: Review Medications: The primary approach is to discontinue any estrogen-containing medications, most commonly the combined oral contraceptive pill. This simple change can effectively resolve the condition in many instances by allowing the hormonal influence to lessen.
Treatment for Persistent Symptoms: If symptoms continue to be problematic, ablation of the columnar epithelium may be considered. This can be achieved through methods like cryotherapy (freezing) or electrocautery (heat). It’s important to note that these procedures will typically result in a noticeable vaginal discharge as the cervix heals post-treatment.
Vaginal pH Adjustment: Using medications to increase vaginal acidity has been suggested as a management strategy. Examples include boric acid pessaries. The rationale is to create a less favorable environment for the columnar cells on the outer cervix.
Observation for Asymptomatic Cases: In many women, cervical erosion is identified incidentally, without any accompanying symptoms. In these asymptomatic cases, specific treatment is generally not recommended, and observation is sufficient.
Cauterization Therapy Options (for Symptomatic Cases):
There are different methods to cauterize, or remove, the affected cells:
Diathermy (Heat Cautery): This method uses heat to carefully destroy the glandular cells on the outer cervix.
Cryotherapy (Freezing): This technique applies intense cold, typically using carbon dioxide, to freeze and destroy the problematic area. A study in 2016 indicated cryotherapy as an effective treatment option for women experiencing excessive discharge related to cervical ectropion.
Silver Nitrate Cautery: This involves applying silver nitrate, a chemical substance, to cauterize the glandular cells.
Post-Treatment Care:
Following cauterization treatment, healthcare providers usually advise women to avoid sexual intercourse and tampon use for approximately four weeks to allow complete healing of the cervix.
When to Seek Medical Review After Treatment:
It’s important for women to be aware of potential complications. Medical attention should be sought if any of the following occur post-treatment:
Foul-smelling vaginal discharge
Heavy vaginal bleeding, significantly more than a typical menstrual period
Persistent vaginal bleeding

CERVICAL POLYPS
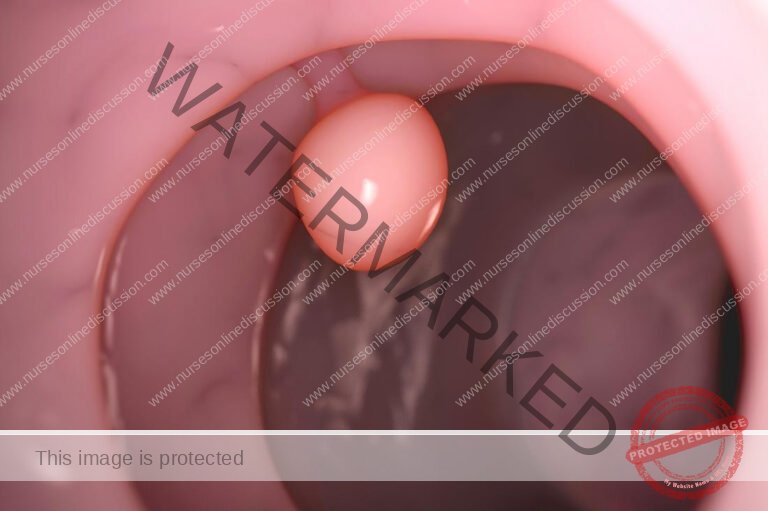
Cervical polyps are benign growths protruding from the inner surface of the cervix.
They are benign tumours arising from the endocervical epithelium and may be seen as smooth reddish protrusion in the cervix.
They are usually asymptomatic, but a very small minority can undergo malignant change. They are estimated to be present in 2-5% of women.
Types of Cervical Polyps
Cervical polyps are categorized based on their origin within the cervix:
Ectocervical Polyps:
Location: These polyps develop on the outer surface of the cervix (ectocervix) and protrude into the vaginal space.
Characteristics: They originate from the stratified squamous non-keratinized epithelium that typically covers the ectocervix. Their external location means they are easily visible during routine pelvic exams.
Appearance: Ectocervical polyps often look like finger-like or grape-like growths extending from the cervix. They vary in size and are typically attached by a stalk or peduncle.
Symptoms: Frequently, they cause no symptoms. However, when symptoms are present, they can include abnormal vaginal bleeding, spotting, or bleeding after intercourse. Their location makes them readily diagnosed during speculum exams.
Endocervical Polyps:
Location: These polyps grow within the endocervical canal, which is the more internal part of the cervix, closer to the uterus.
Characteristics: They arise from the mucus-secreting simple columnar epithelium that lines the endocervical canal. Being located inside the canal, they are less easily seen during standard pelvic exams compared to ectocervical polyps.
Appearance: Endocervical polyps are less visible externally but may be detected through imaging methods like ultrasound or hysteroscopy. In some cases, they can block the cervical canal.
Symptoms: Similar to ectocervical polyps, they may cause abnormal bleeding or spotting. However, their internal location can sometimes have a greater impact on fertility or potentially interfere with the accuracy of cervical smear tests.
Clinical Features of Cervical Polyps
Often without symptoms, and discovered during routine cervical screening.
Abnormal Vaginal Bleeding:
Menorrhagia: Heavy menstrual periods.
Intermenstrual bleeding: Bleeding between regular menstrual cycles.
Post-coital bleeding: Bleeding after sexual intercourse.
Post-menopausal bleeding: Bleeding after menopause.
Increased Vaginal Discharge.
Infertility is rare, but large polyps can potentially block the cervical canal, making conception more difficult.
Visible on Speculum Examination: During a speculum exam, cervical polyps are typically seen as growths protruding from the cervical opening (external os).
Aetiology
The precise cause of cervical polyps is not fully understood. However, some factors are considered to increase the risk:
Premenopausal status: More common in women before menopause.
Multigravidity: Women who have had multiple pregnancies.
Sexually Transmitted Infections (STIs): May play a role in polyp development.
History of Cervical Polyps: Having had cervical polyps in the past increases the risk of recurrence.
Chronic Cervicitis: Long-term inflammation of the cervix.
Chronic Inflammation: General inflammation may be a contributing factor.
Abnormal Response to Oestrogen: Linked to conditions related to excessive oestrogen influence, such as endometrial hyperplasia.
Localized Congestion of Cervical Blood Vessels: Increased blood flow and congestion in cervical vessels may be involved.
Investigations
A definitive diagnosis of a cervical polyp is made through histological examination of the polyp after it’s removed. Other investigations mainly aim to rule out other causes of symptoms:
Triple Swabs: Taken if infection is suspected (e.g., purulent discharge). These swabs typically include endocervical and high vaginal samples.
Cervical Smear (Pap Smear): Performed to exclude cervical intraepithelial neoplasia (CIN), a precancerous condition. If a polyp obstructs taking a smear, the smear should be repeated after polyp removal.
Management
Removal is generally recommended for all cervical polyps, even if they are asymptomatic, due to a very low (less than 0.5%) but present risk of malignant transformation.
Simple Removal in Office: Polyps are usually easily removed during an office visit, without needing anaesthesia.
Removal Technique: They are typically removed by grasping and gently twisting them off, or using polypectomy forceps or ring forceps.
Cauterization of Bleeding: Any bleeding after removal can be stopped using silver nitrate cautery.
Histopathological Examination: Removed polyps are sent to a laboratory for pathological examination to confirm they are benign and exclude any signs of malignancy.

- If the polyps is infected antibiotics may be prescribed.
- Larger polyps, or those that are more difficult to access can be removed by diathermy loop excision in the colposcopy clinic, or under general
anaesthesia if the base of the polyp is broad. - Any excised polyps should be sent for histological examination to exclude malignancy. They have a recurrence rate of 6-12%
CERVICAL TRAUMA
Cervical trauma refers to physical injury to the cervix, the lower part of the uterus.
Etiology
Cervical injuries can arise from various factors, including:
Delivery Complications: Physical stress to the cervix during childbirth, particularly in cases of prolonged labour or difficult deliveries.
Aggressive Sexual Activity: Cervical tissue damage resulting from forceful or rough sexual practices.
Surgical Interventions: Injury to the cervix as a consequence of gynecological surgeries or procedures involving the vagina.
Elevated Vaginal Acidity: Irritation and potential harm to cervical tissues due to excessively acidic vaginal fluids.
Improper Tampon Use: Cervical damage caused by incorrect or forceful insertion or removal of tampons.
Unsafe Abortion Practices: Cervical injuries resulting from illegal or improperly performed abortions, especially when using unsuitable tools.
Gynecological Procedures: Risk of trauma during certain medical interventions, for instance, dilation and curettage (D&C).
Clinical Features
Cervical trauma can manifest through several symptoms:
Painful Intercourse (Dyspareunia): Discomfort or pain experienced during sexual activity is a common indicator.
Postcoital Bleeding: Bleeding that occurs after sexual intercourse is a significant clinical sign.
Unexplained Vaginal Bleeding: Vaginal bleeding without a clear cause or persistent unusual bleeding can be a symptom.
Lower Abdominal Discomfort: Pain or general discomfort felt in the lower abdominal region may be associated with cervical injury.
Investigations
To assess cervical trauma, the following investigations may be employed:
Speculum Examination: A visual inspection of the cervix using a speculum to identify any visible signs of injury.
High Vaginal Swab: Taking a swab to check for infections or abnormal vaginal discharge that might be related to the trauma.
Cryotherapy (as diagnostic tool): In some cases, cryotherapy might be used to further evaluate the extent of cervical trauma.
Medical History Review: Gathering detailed information about the patient’s medical history and the context surrounding their symptoms to understand potential causes.
Management
Management strategies for cervical trauma typically include:
Antibiotic Therapy: Prescribing broad-spectrum antibiotics to prevent or treat any infections that may arise from the cervical injury.
Pain Relief (Analgesics): Providing pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), to alleviate discomfort.
Sexual Abstinence: Recommending avoidance of sexual intercourse until the cervix has adequately healed to prevent further injury and promote recovery.
Rest and Recuperation: Advising sufficient rest and sleep to aid the body’s natural healing processes and avoid strain on the pelvic area.
Follow-up Appointments: Scheduling regular check-up examinations to monitor the healing progress of the cervix and adjust the treatment plan as necessary.
Pelvic Floor Exercises: Suggesting gentle pelvic floor exercises to help strengthen muscles and support tissue healing in the pelvic region.
Hygiene Maintenance: Emphasizing good hygiene practices to minimize the risk of infection as the cervix heals.
Avoidance of Irritants: Instructing the patient to avoid using vaginal douches, tampons, or harsh soaps that could irritate the healing cervix.
Psychological Support: Offering emotional support and acknowledging the potential psychological impact of the trauma, encouraging open discussion of concerns.
Patient Education: Educating the patient on the causes of cervical trauma, preventative measures, and warning signs that require immediate medical attention.
Complication Monitoring: Closely watching for any signs of complications, such as persistent bleeding, worsening pain, or indications of infection.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

