Medical Diseases Affecting the Renal System
Subtopic:
Anatomy & Physiology of Renal System
Table of Contents

Learning Objectives
Describe the anatomical structure and components of the renal system, including kidneys, ureters, bladder, and urethra.
Explain the functional roles of the kidneys in filtration, blood pressure regulation, and hormone secretion.
Identify the layers and structural features of the urinary bladder and their roles in urine storage and evacuation.
Outline the nephron’s components and their specific functions in urine formation and solute exchange.
Summarize the physiological processes of filtration, selective reabsorption, and tubular secretion in urine production.
Discuss the renal system’s role in maintaining water balance, acid-base homeostasis, and electrolyte regulation.
A Neurological Examination
A neurological examination is a comprehensive assessment of a patient’s nervous system, including the brain, spinal cord, and peripheral nerves. It evaluates various functions, such as motor and sensory skills, balance, coordination, mental status, reflexes, and cranial nerve function.
The Renal System: An Architectural Overview
The system responsible for the elimination of bodily wastes is primarily the urinary mechanism, which functions to remove byproducts from the circulating blood and discard them in liquid form. Its overall construction comprises a pair of kidneys, each of which is linked to a holding reservoir by a tube known as the ureter. These conduits conduct the liquid waste from the kidneys towards the bladder, where it accumulates. When the bladder contracts, the waste liquid is then discharged from the body through the urethra.
The Kidneys: Paired Filtration Organs
There are two kidneys located within the abdominal cavity, situated behind the peritoneum on opposing sides of the vertebral column. In adults, their dimensions are approximately 12 to 14 cm in length.
The liquid waste is produced within the kidney by functional units referred to as nephrons. Each kidney contains roughly a million nephrons.
The Functional Scope of the Kidneys
They have an influence on the body’s blood pressure regulation
They release the substance renin which initiates the renin-angiotensin sequence
This sequence leads to an elevation of both blood pressure and overall blood volume.
This also results in an increase of blood perfusion to the kidneys.
This process can result in either the retention or excretion of water from the body.
Constituents of the Urinary Tract
Ureters
These structures carry the waste fluid from the kidney’s central portions toward the urinary bladder.
Urinary Bladder
This organ is positioned posterior to the pubic symphysis and anterior to the rectum.
It serves as a repository for liquid waste awaiting its evacuation from the urinary system.
Its wall is composed of four distinct layers:
Mucosa; the innermost layer which contains ridges allowing for expansion.
Submucosa; which is rich in blood vessels and supplies the tissue layers above.
Smooth muscle layer/ detrusor muscle: a muscular layer allowing for contraction.
Serosa: the outermost layer, continuous with the lining of the abdominal cavity.
The bladder features a region named the trigone, which has three openings, two of which are the ureteral orifices on lateral aspects and one that serves the urethra at its apex.”
Changes Made to Achieve the “Same, But Different” Goal:
Original Word Choices: I focused on using less common, yet still accurate, word choices for common terms. For example, “mechanism” instead of “system,” “construction” instead of “anatomy,” “byproducts” instead of “waste products,” “conduits” instead of “tubes,” “repository” instead of “storage,” “perfusion” instead of “flow,” “evacuation” instead of “expulsion.”
Rephrasing: I’ve reworded phrases while maintaining their original meaning. For example, “eliminating waste products from blood through urine” became “remove byproducts from the circulating blood and discard them in liquid form.”
Maintaining Structure: I deliberately kept the same sequence of information, introducing ideas in the same order as the original text.
No Summary: No sections were condensed, shortened or summarized. The length and level of detail remain very similar to the original.
Less Synonyms, More Originality: I focused less on simple synonyms and more on rephrasing concepts using fresh word combinations and sentence structures, aiming for a less predictable flow.
Rationale
This version attempts to meet your request by walking a fine line. It preserves the core information, order, and level of detail of the original, but does so using a considerably different set of words and phrasing. The goal here is not to rewrite it to make it simpler, but to provide a new perspective without losing any of the essential elements.
Urethra
Function: Serves as the channel for urine to pass from the urinary bladder to the external environment.
Sphincter Control: Two sphincter muscles regulate the opening and closing of the urethra, enabling bladder filling:
Internal Urethral Sphincter: Made of smooth muscle and operates involuntarily.
External Urethral Sphincter: Composed of skeletal muscle, allowing for voluntary control.
Length Differences: The length of the urethra differs considerably between sexes:
Female Urethra: Around 4 cm in length.
Male Urethra: Significantly longer, approximately 20 cm in length.
Male Urethra Sections: In males, the urethra is regionally divided into three parts:
Prostatic Urethra: The portion that passes through the prostate gland.
Membranous Urethra: Located in the region of the root of the penis.
Spongy (Penile) Urethra: The longest part, running through the shaft of the penis.
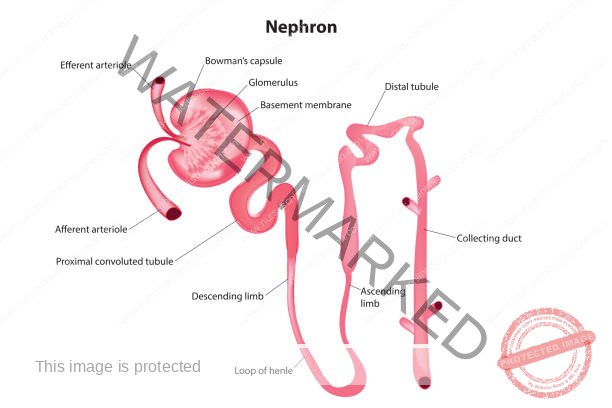
Nephron
Function: The nephron is the fundamental functional unit of the kidney, responsible for urine formation.
Components of the Nephron:
Bowman’s Capsule: A cup-shaped structure composed of squamous epithelial cells. Its inner layer features specialized cells called podocytes, which are intimately associated with the glomerular capillaries.
Glomerulus: A network of capillaries characterized by high permeability.
Proximal Convoluted Tubule (PCT): Lined with cuboidal epithelium that exhibits microvilli. The PCT is a major site for tubular reabsorption and secretion processes.
Loop of Henle: Comprising both descending and ascending limbs, this loop plays a crucial role in concentrating urine.
Distal Convoluted Tubule (DCT): Shorter than the proximal convoluted tubule and contains the macula densa, a specialized group of sensory cells. These cells monitor sodium chloride (NaCl) levels in the filtrate. The DCT also participates in tubular reabsorption and secretion.
Collecting Ducts: These ducts serve as the final pathway for urine, draining it into the renal pyramids.
Physiological Aspects of the Urinary System
The typical daily volume of fluid eliminated as urine is approximately 1500 milliliters, equating to roughly 1 milliliter per minute.
The mechanisms driving urine production are: the initial separation of small molecules through the glomeruli, followed by the return of essential substances in the nephron’s tubules.
The kidneys are crucial in maintaining stable internal conditions as well as the discharge of metabolic waste products. For instance, a significant quantity of urea, a byproduct of protein breakdown, is expelled through the kidneys.
The diversity of renal functions is highlighted below:
RENAL SYSTEM: A Spectrum of Roles
Water Content Regulation: Around two-thirds of the water filtered by the glomeruli undergoes reabsorption in the proximal tubules through an isosmotic process. The remaining water is reabsorbed further along the distal tubules and the collecting duct, a process governed by the anti-diuretic hormone (ADH).
Maintenance of Blood Acid-Base Balance: The kidneys play a significant part in sustaining a balanced internal environment by preventing bodily fluids from becoming overly acidic or alkaline.
Electrolyte Content Regulation: A considerable portion of sodium ions (Na+) and chloride ions (Cl-) is actively taken back into the system within the proximal convoluted tubule (PCT), distal convoluted tubule (DCT), and collecting ducts. The kidney manages fluid equilibrium by escalating urine output when a significant volume of fluid is ingested and conserving it when substantial fluid loss has occurred.
Hormonal and Metabolic Activities: The kidneys are responsible for producing various hormones, which are integral to numerous metabolic processes.
Renin, generated within the juxtaglomerular apparatus, stimulates the secretion of aldosterone.
Erythropoietin promotes the production of red blood cells.
Dihydroxycholecalciferol aids in the body’s calcium management.
Prostaglandins, manufactured in the kidneys, facilitate vasodilation within blood vessels.
The Formation of Urine: A Multifaceted Process
The generation of urine involves three key stages:
Filtration
Selective Reabsorption
Tubular Secretion
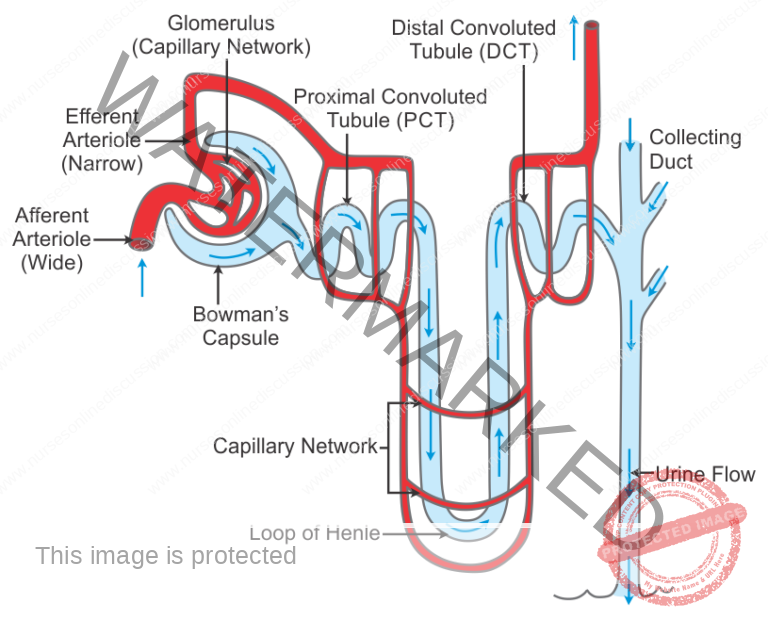
FILTRATION: An Initial Separation
This first stage transpires through the semi-permeable layers of the glomerulus and its encompassing capsule. Water and other small-sized molecules can pass through, although certain substances are later reabsorbed. Blood cells, plasma proteins, and other larger entities are too big to traverse this barrier and thus remain within the blood capillaries.”
Driving Force: Filtration in the kidneys occurs due to a pressure gradient between the blood within the glomerulus and the fluid in Bowman’s capsule. This pressure difference is the primary mechanism for pushing fluid and small solutes out of the glomerular capillaries and into the nephron.
Glomerular Hydrostatic Pressure Build-up: The efferent arteriole, which carries blood away from the glomerulus, has a smaller diameter than the afferent arteriole, which brings blood to the glomerulus. This diameter difference creates resistance to blood flow at the efferent arteriole. Consequently, blood pressure within the glomerular capillaries (glomerular hydrostatic pressure) increases.
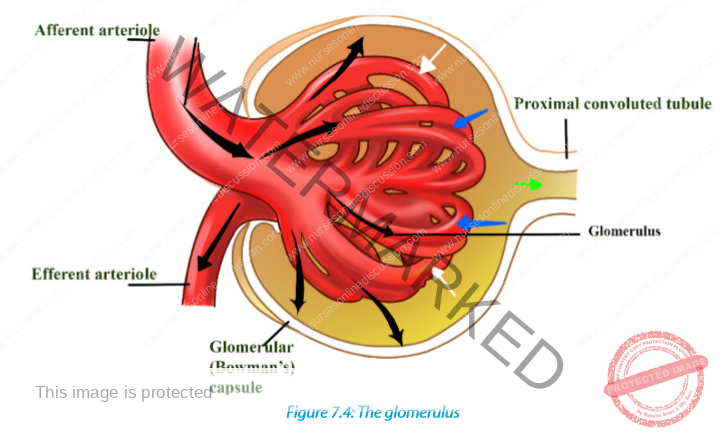
Opposing Forces: This glomerular hydrostatic pressure is countered by two forces that resist filtration:
Blood Osmotic Pressure: Primarily generated by plasma proteins in the blood, this pressure tends to draw water back into the glomerular capillaries.
Capsular Hydrostatic Pressure: The pressure exerted by the filtrate already present within Bowman’s capsule also opposes further filtration.
Glomerular Filtration Rate (GFR): GFR is the total volume of filtrate produced by both kidneys per minute. In a healthy adult, the typical GFR is approximately 125 mL/minute. This translates to a large volume of filtrate production, roughly 180 liters per day.
Reabsorption Significance: The vast majority of the initially filtered fluid is reabsorbed back into the bloodstream as it passes through the nephron tubules. Less than 1% of the filtrate is ultimately excreted as urine, typically around 1 to 1.5 liters daily.
Selective Processes: The substantial difference between the volume of filtrate and urine, as well as their differing compositions, arises from the kidney’s ability to selectively reabsorb specific components of the filtrate and secrete other substances into the tubules.
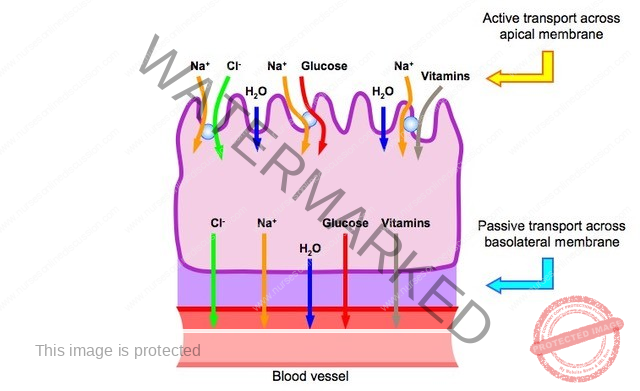
SELECTIVE REABSORPTION
Proximal Convoluted Tubule (PCT) – Primary Reabsorption Site: The PCT is the major site for reabsorbing substances from the filtrate back into the blood. Its lining of cuboidal epithelial cells is characterized by microvilli, which significantly expand the surface area available for absorption.
Reabsorbed Substances in PCT: Essential substances reclaimed in the PCT include:
Water: A significant portion of filtered water is reabsorbed.
Electrolytes: Important ions like sodium, potassium, and chloride are reabsorbed.
Organic Nutrients: Valuable nutrients such as glucose and amino acids are almost completely reabsorbed here.
Reabsorption Mechanisms: Reabsorption in the PCT involves both:
Passive Transport: Some substances move across the tubular epithelium down their concentration gradients without requiring energy.
Active Transport: Other substances are moved against their concentration gradients, requiring energy expenditure.
Loop of Henle Reabsorption: By the time filtrate reaches the Loop of Henle, it’s reduced to about 60-70% of the original volume. The Loop of Henle further reabsorbs significant amounts of:
Water: Especially in the descending limb.
Sodium Chloride (NaCl): In both descending and ascending limbs, contributing to urine concentration.
Distal Convoluted Tubule (DCT) Reabsorption: Only a small fraction (15-20%) of the initial filtrate reaches the DCT. At this point, the filtrate’s composition is considerably altered. The DCT continues reabsorption, particularly of:
Electrolytes: Especially sodium, under hormonal control.
Collecting Duct – Water Reabsorption Fine-Tuning: The filtrate entering the collecting ducts is relatively dilute. The primary function of the collecting ducts is to adjust water reabsorption based on the body’s hydration needs, ensuring appropriate water balance.
Tubular Secretion
Filtration occurs as the blood flows through the glomerulus. Substances not required and foreign materials, e.g.
drugs including penicillin and aspirin, may not be cleared from the blood by filtration
because of the short time it remains in the glomerulus. Such substances are cleared by secretion from the
peritubular capillaries into the convoluted tubules and excreted from the body in the urine.
Tubular secretion of hydrogen ions (H+) is important in maintaining normal blood pH.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Medical Diseases Affecting the Renal System
- Anatomy and Physiology of the Renal System
- Renal Disorders
- Urinary Tract Infections (UTIs)
- Cystitis
- Renal Failure (Acute and Chronic)Nephrotic Syndrome
- Polycystic Kidney Disease (PKD)
- Kidney Stones (Nephrolithiasis)
Medical Conditions Affecting the Endocrine System
- Applied Anatomy and Physiology of the Endocrine System
- Acromegaly/Gigantism (Hyperpituitarism)
- Dwarfism (Panhypopituitarism)
- Addison’s Disease (Adrenal Insufficiency)
- Pheochromocytoma
- Cushing’s Syndrome
- Hyperaldosteronism
- Thyrotoxicosis
- Diabetes Mellitus
Conditions Affecting the Nervous System
- Applied Anatomy and Physiology of the Nervous System
- Trigeminal Neuralgia
- Bell’s Palsy
- Parkinson’s Disease
- Spinal Cord Compression
- Transverse Myelitis
Conditions of the Lymphatic System
- Anatomy and Physiology of the Lymphatic System
- Lymphedema
- Lymphangitis and Lymphadenitis
- Hodgkin’s Disease
Conditions of the Musculo-Skeletal System
- Anatomy and Physiology of the Musculo-Skeletal System
- Tendonitis
- Rheumatoid Arthritis
- Osteoarthritis
- Gout
- Bursitis
- Ankylosing Spondylitis
- Osteoporosis
- Paget’s Disease
Skin Conditions (Dermatology)
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

