Medical Nursing (III)
Subtopic:
Cystitis

Cystitis is a lower lower urinary infection involving inflammation of the urinary bladder.
Acute bacterial cystitis is common in women as the short urethra predisposes them to infection of the bladder.
Causes of Cystitis
Urinary Tract Obstruction: Conditions that impede the free flow of urine, such as bladder stones and growths (tumors), can predispose to cystitis. Blockages can lead to stagnant urine, fostering bacterial growth.
Impaired Bladder Emptying: Incomplete voiding of the bladder can leave residual urine, creating an environment conducive to bacterial proliferation and subsequent infection.
Neoplasms of the Bladder: Tumors within the bladder can obstruct the urinary passage, resulting in urinary stasis and consequently elevating the risk of infection.
Prostatic Hyperplasia & Paralysis: Enlargement of the prostate gland and paraplegia, alongside extended use of urinary catheters, are recognized risk factors for developing cystitis. These conditions can disrupt normal bladder function and increase susceptibility to infection.
Underlying Systemic Infections: Certain systemic infections, including gonorrhea and tuberculosis, can also contribute to the development of cystitis as secondary complications.
Ascending Bacterial Infections: A significant proportion of lower urinary tract infections (UTIs) arise from bacteria ascending from the lower urinary tract. These are often Gram-negative enteric bacteria such as Escherichia coli, Klebsiella, Proteus, Enterobacter, Pseudomonas, and Serratia.
Compromised Immune System: A weakened immune system, whether due to illness or immunosuppressive medications, increases an individual’s vulnerability to infections, including cystitis.
Specific Infective Agents: Various pathogens can cause cystitis, including:
Klebsiella aerogenes
Proteus mirabilis
Escherichia coli and Enterococcus faecalis (predominant causes in approximately 80% of cases)
Streptococcus faecalis
Chlamydia trachomatis
Neisseria gonorrhoeae
Mycobacterium tuberculosis
Clinical Manifestations of Cystitis
Dysuria: Pain or discomfort experienced during urination.
Nocturia: The need to urinate excessively during nighttime hours.
Urethral Discharge: Possible, especially in male patients, indicating inflammation or infection.
Urinary Frequency and Urgency: An increased need to urinate more often than usual, often with a sudden, compelling urge.
Pyuria: Urine that appears cloudy or turbid due to the presence of white blood cells (pus).
Fever: Elevated body temperature, suggesting a systemic inflammatory response.
Hematuria: The presence of blood in the urine.
Suprapubic Tenderness: Pain or sensitivity in the lower abdominal region, often described as a burning sensation.
Malodorous Urine: Urine with an unpleasant or foul smell.
Nausea and Vomiting: Gastrointestinal upset may occur in some cases.
Fatigue and Anorexia: General feelings of tiredness and loss of appetite.
Bacteriuria: The presence of bacteria in the urine, confirmed through laboratory testing.
Investigating Cystitis
Urinalysis: Analysis of a midstream urine sample to detect abnormal components like proteins and pus. Microscopic examination helps identify the causative organism.
Blood Tests: Measurement of urea and creatinine levels in the blood to assess kidney function.
Cystoscopy/Intravenous Pyelography (IVP): Endoscopic examination of the bladder and X-ray imaging of the urinary tract, respectively, may be used in specific cases to visualize the urinary system.
Computed Tomography (CT) Scan: Imaging technique to identify potential complications such as pyelonephritis (kidney infection) or abscesses.
Ultrasonography: A highly effective imaging modality for detecting urinary tract obstructions, abscesses, tumors, and cysts.
Microscopic Examination of Urine Sediment: Cellular studies of urine sediment frequently reveal microscopic hematuria (red blood cells) and pyuria (white blood cells) in cystitis cases.
Leukocyte Esterase Test: A rapid screening test using a multi-test dipstick to detect the presence of leukocyte esterase, an enzyme indicative of white blood cells in urine.
Management of Cystitis
Antimicrobial Therapy: Treatment with appropriate antibiotics is crucial. Antibiotic selection is guided by urine culture and sensitivity testing, and therapy typically lasts for 7-10 days. Examples include:
Ciprofloxacin: Dosage ranging from 250mg to 500mg twice daily.
Nitrofurantoin: 100mg administered every 8 hours for a 5-day course.
Cotrimoxazole: Dosage of 960mg to 480mg every 12 hours.
Ampicillin or Gentamicin: May be used depending on bacterial susceptibility.
Analgesia: Pain relievers are used to manage discomfort associated with cystitis.
Increased Hydration: Encouraging a high fluid intake helps to flush out bacteria from the bladder and soothe irritated tissues.
Urine Monitoring: Regular follow-up urine examinations are important to ensure treatment effectiveness.
Avoidance of Bladder Irritants: Limiting or avoiding substances that can irritate the bladder, such as coffee, alcohol, citrus juices, chocolate, certain carbonated drinks, and spicy foods, can aid in recovery.
Patient Education: Counseling patients on UTI prevention strategies and the importance of adhering to the prescribed treatment regimen is essential.
Rest: Adequate rest supports the body’s healing processes.
Safe Sexual Practices: Using condoms or abstaining from sexual activity during treatment helps prevent reinfection and transmission.
Perianal Hygiene Education: Emphasis on proper hygiene practices, including wiping front to back, and discouraging the sharing of personal bathing items.
Preventive Measures and Patient Advice
Maintain Hydration: Drink ample fluids, aiming for approximately 8 glasses of water daily, to promote urinary tract health.
Avoid Delaying Urination: Urinate promptly when the urge arises to prevent urinary stasis.
Practice Proper Hygiene: Wipe from front to back after urination and bowel movements to minimize bacterial contamination of the urethra.
Post-Coital Voiding: Empty the bladder shortly after sexual intercourse to help flush out bacteria that may have entered the urethra.
Avoid Vaginal Irritants: Refrain from using potentially irritating feminine hygiene products such as deodorant sprays and douches.
Medication Adherence: Strictly follow the prescribed medication regimen to ensure complete eradication of bacteria and prevent the development of antibiotic resistance.
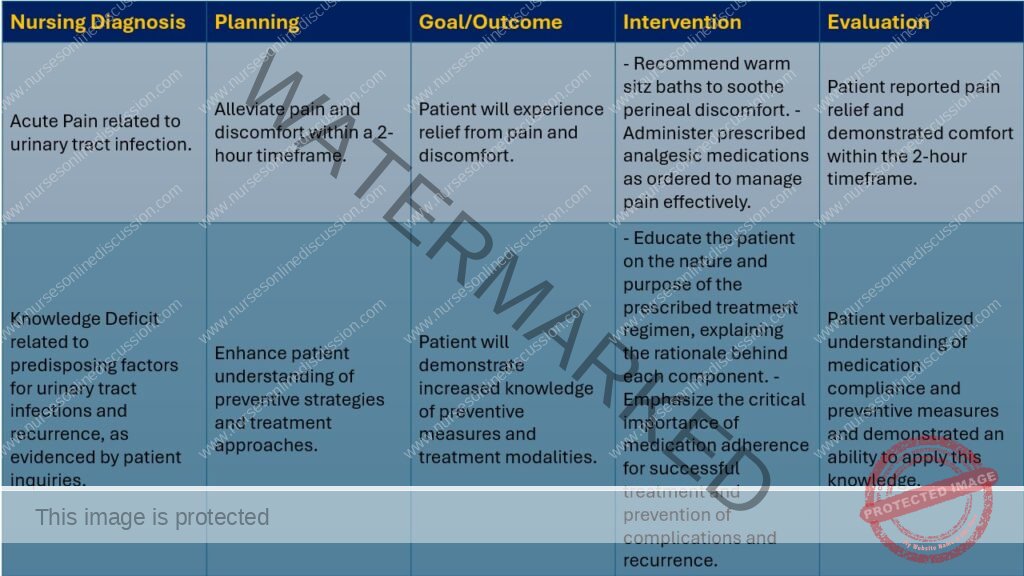
Nursing Care Plan
A lumbar puncture (also known as a spinal tap) is a medical procedure that involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF). This is done by inserting a special needle into the subarachnoid space – the space between the spinal cord and its protective covering (the meninges) – typically between the third and fourth or fourth and fifth lumbar vertebrae. This location is chosen because the spinal cord ends higher up, minimizing the risk of damaging it with the needle.
CSF is the fluid that surrounds the brain and spinal cord.
Indications for Lumbar Puncture
A lumbar puncture may be performed for several reasons, including:
URETHRITIS
Definition: Urethritis is characterized by inflammation of the urethra, the tube that carries urine from the bladder to the outside of the body.
Co-occurrence with Cystitis: Urethritis frequently occurs alongside cystitis (bladder inflammation), which can complicate diagnosis and make it challenging to differentiate between the two conditions based on symptoms alone.
Etiology of Urethritis
Infectious Agents in Women:
Trichomonas vaginalis infections
Monilial infections (yeast infections, typically Candida)
Infectious Agents in Men:
Chlamydia trachomatis (common cause)
Neisseria gonorrhoeae (common cause)
Other Bacterial Causes: Similar bacterial species that cause cystitis can also lead to urethritis.
Viral Pathogens: Viruses, such as Herpes simplex virus (HSV), can be responsible for urethritis.
Non-infectious Urethritis: Irritation from chemical agents can induce urethritis. These irritants may include:
Deodorant sprays
Certain drugs
Signs and Symptoms of Urethritis
(a) Urethral Discharge: The presence of discharge from the urethra is a key diagnostic indicator of urethritis.
(b) Dysuria and Urethral Pruritus: Pain or burning sensation during urination (dysuria) and itching within the urethra (urethral pruritus) are common symptoms.
(c) Overlapping Symptoms with Cystitis: Patients may exhibit other signs and symptoms that are also characteristic of cystitis, further complicating differential diagnosis based on symptoms alone.
Diagnostic Investigations
Urine Culture: Laboratory analysis of a urine sample to identify and isolate the specific microorganisms causing the infection.
Investigations Similar to Cystitis: Diagnostic approaches used for cystitis may also be employed in cases of urethritis to rule out other conditions or co-existing infections.
Management of Urethritis
Chlamydia Treatment: Doxycycline, administered at a dosage of 100mg every 12 hours, is a common antibiotic used to treat Chlamydia infections.
Trichomoniasis Treatment: Metronidazole is the drug of choice for Trichomonas infections, typically prescribed at a dosage of 200–400mg every 8 hours for a 7-day duration.
Monilial Infection Treatment: Antifungal medications like nystatin or fluconazole are used to treat monilial (yeast) infections.
Pain Management: Analgesics (pain relievers) are prescribed to alleviate pain and discomfort.
Antibiotic Options: Similar antibiotics used for cystitis can be effective for bacterial urethritis, including:
Ciprofloxacin: 250mg to 500mg dosages.
Nitrofurantoin: 100mg every 8 hours for 5 days.
Cotrimoxazole: 960 to 480mg every 12 hours.
Sitz Baths: Warm sitz baths can provide symptomatic relief, particularly for women experiencing discomfort.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

