Genitourinary Conditions in Children
Subtopic:
Nephrotic syndrome
Nephrotic syndrome, also known as nephrosis, is a cluster of symptoms characterized by substantial protein loss in urine (nephrotic range proteinuria), widespread swelling (edema), reduced levels of albumin in the blood (hypoalbuminemia), and may include elevated lipid levels in the blood (hyperlipidemia).
Key Features:
MASSIVE Proteinuria: Urinary protein excretion exceeding 3.5 grams per 24 hours. Alternatively, assessed by spot urine protein to creatinine ratio of greater than 300 – 350 mg/mmol.
Hypoalbuminemia: Reduced blood albumin concentration, typically below 25g/L.
Edema: Swelling due to fluid retention. Generalized edema is clinically referred to as Anasarca.
Hyperlipidemia/dyslipidemia: Frequently observed, characterized by elevated total cholesterol levels (>10 mmol/L).
Furthermore, the loss of immunoglobulins elevates susceptibility to infections, and the loss of proteins responsible for preventing blood coagulation increases the likelihood of blood clot formation in affected individuals.
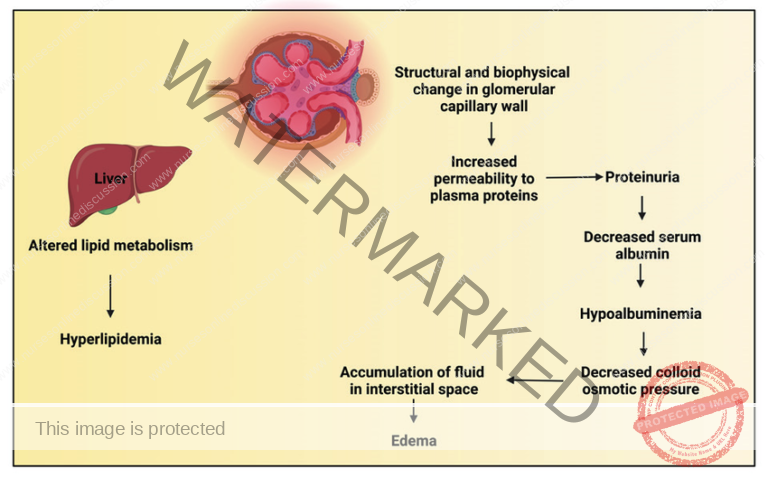
Pathophysiology of Nephrotic Syndrome
Nephrotic syndrome results from damage to the kidney’s glomeruli, the tiny blood vessels that filter waste and
excess water from the blood and send them to the bladder as urine.
Damage to the glomeruli from diabetes or even prolonged hypertension causes the membrane to become porous,
so that small proteins such as albumin pass through the kidneys into urine.
Glomerular Filtration Barrier Disruption: The renal glomerulus, responsible for filtering blood entering the kidney, consists of capillaries with small pores. In nephrotic syndrome, inflammation or hyalinization
affects the glomeruli, allowing proteins, including albumin, antithrombin, and immunoglobulins, to pass
through the normally restrictive cell membrane.
Proteinuria: Increased permeability results in the leakage of proteins into the urine. Albumin, a key protein
for maintaining oncotic pressure in the blood, is lost in significant amounts.
Hypoalbuminemia: Loss of albumin in the urine reduces the oncotic pressure in the blood. Reduced
oncotic pressure leads to the accumulation of fluid in the interstitial tissues, causing edema.
Hyperlipidemia: Hypoalbuminemia triggers compensatory mechanisms in the liver. The liver increases
the synthesis of proteins such as alpha-2 macroglobulin and lipoproteins. Elevated lipoprotein levels
contribute to hyperlipidemia associated with nephrotic syndrome.
Signs and Symptoms of Nephrotic Syndrome
Manifestation of Glomerular Disease
Characterized by nephrotic-range proteinuria alongside a trio of clinical signs linked to substantial protein loss in urine: low albumin in the blood (hypoalbuminaemia), swelling (edema), and elevated blood lipids (hyperlipidemia).
Weight Gain
Patients typically notice an increase in body weight because of fluid retention. This fluid build-up, primarily caused by significant protein in the urine and reduced oncotic pressure, leads to a gain in weight.
Facial Edema (Puffiness Around the Eyes)
Swelling, particularly prominent around the eyes, following a specific pattern. Widespread edema is termed Anasarca.
Morning Onset: Puffiness is most visible upon waking and tends to lessen as the day progresses.
Location: Primarily seen around the eye area.
Abdominal Swelling
Enlargement of the abdominal area. This can be associated with:
Pleural Effusion: Fluid accumulation in the pleural space surrounding the lungs.
Labial or Scrotal Swelling: Swelling in the genital regions.
Edema of Intestinal Mucosa: Swelling of the intestinal lining, potentially causing various digestive symptoms.
Diarrhea: Resulting from swelling affecting the intestinal lining.
Anorexia: Loss of appetite due to abdominal discomfort and swelling.
Poor Intestinal Absorption: Reduced nutrient uptake, potentially leading to malnutrition.
Ankle/Leg Swelling
Edema affecting the lower legs and ankles. Fluid builds up in these areas due to imbalances in fluid regulation within the body.
Behavioral Changes
Alterations in mood and behavior can occur, presenting as:
Irritability: Increased agitation or frustration levels.
Easily Fatigued: Experiencing tiredness more readily than usual.
Lethargy: Persistent state of tiredness and reduced energy levels, indicating general weakness.
Susceptibility to Infection
Increased risk of developing infections. Loss of protective antibodies (immunoglobulins) in the urine, combined with possible immune suppression from treatments like corticosteroids, elevates the chance of infections.
Urine Alterations
Changes in urine characteristics, including:
Decreased Volume: Reduced amount of urine produced.
Frothy Urine: Urine appears foamy or bubbly, indicating substantial protein presence.
Lipiduria: Presence of fats in the urine; while it can occur, it’s not essential for diagnosing nephrotic syndrome.
Hyponatremia: Low sodium levels in the blood, often accompanied by low sodium excretion in urine.
Hyperlipidaemia
Low blood protein levels (hypoproteinemia) trigger increased protein production in the liver, leading to an overproduction of lipoproteins and consequently high lipid levels in the blood.
Anaemia
Iron-resistant microcytic hypochromic anaemia might be present, potentially due to the loss of transferrin (an iron-transport protein) in the urine.
Dyspnea
Shortness of breath may occur because of pleural effusion or due to pressure on the diaphragm from abdominal fluid accumulation (ascites).
Other features
Patients might exhibit signs related to the underlying cause of nephrotic syndrome, such as the rash associated with systemic lupus erythematosus, or nerve damage (neuropathy) linked to diabetes.
Causes of Nephrotic Syndrome
Nephrotic syndrome arises from numerous underlying factors and can be categorized based on whether the primary disease originates within the kidney or is a manifestation of a systemic condition.
Primary Causes
Minimal change disease (MCD): This is the most common cause of nephrotic syndrome in children. Its name reflects the normal appearance of nephrons under an optical microscope, with lesions only visible using an electron microscope. A pronounced proteinuria is a key symptom.
Focal segmental glomerulosclerosis (FSGS): This represents the most common cause of nephrotic syndrome in adults. It is characterized by the presence of tissue scarring within the glomeruli. The term “focal” indicates that some glomeruli are scarred while others are intact, and “segmental” means that only a portion of the affected glomerulus is damaged.
Membranous glomerulonephritis (MGN): This condition involves inflammation of the glomerular membrane, leading to increased leakage within the kidney. The exact reason for its development is often unclear, although an autoimmune mechanism is suspected.
Membranoproliferative glomerulonephritis (MPGN): This involves inflammation of the glomeruli along with the deposition of antibodies in their membranes, hindering the filtration process.
Rapidly progressive glomerulonephritis (RPGN): (Typically presents as a nephritic syndrome) In this condition, the glomeruli exhibit a characteristic crescent moon shape. Clinically, it is marked by a rapid decline in the glomerular filtration rate (GFR) by at least 50% over a short period, typically ranging from a few days to 3 months.
Secondary Causes
Diabetic nephropathy: This complication can occur in individuals with diabetes. Excess blood sugar accumulates in the kidneys, causing inflammation and impairing their normal function, which leads to protein leakage into the urine.
Systemic lupus erythematosus: This autoimmune disease can affect various organs, including the kidneys, due to the deposition of immune complexes characteristic of the disease. This can result in lupus nephritis.
Infections:
Syphilis: Kidney damage can occur during the secondary stage of this infection, approximately 2 to 8 weeks after onset.
Hepatitis B: Certain antigens present during Hepatitis B can accumulate in the kidneys and cause damage.
HIV: The virus’s antigens can cause an obstruction in the glomerular capillary lumen, disrupting normal kidney function.
Vasculitis: Inflammation of the blood vessels at the glomerular level can impede normal blood flow and damage the kidney.
Cancer: In conditions like myeloma, the invasion of the glomeruli by cancerous cells can disrupt their normal functioning.
Genetic disorders: Congenital nephrotic syndrome is a rare genetic disorder involving an alteration in the protein nephrin, a component of the glomerular filtration barrier.
Drugs (e.g., gold salts, penicillin, captopril): Gold salts can lead to varying degrees of protein loss in the urine due to metal accumulation. Penicillin can be nephrotoxic in patients with kidney failure, and captopril can exacerbate proteinuria.
Diagnosis, Investigations, and Treatment of Nephrotic Syndrome
Diagnosis and Investigations
Initial Assessment:
Obtain a thorough medical history, including any acute or chronic conditions, family history of kidney disease, and a review of systems to identify symptoms such as edema, fatigue, and foamy urine.
Perform a physical examination focusing on signs of fluid overload, such as edema and ascites, as well as other systemic findings.
Laboratory Investigations:
Conduct urinalysis to detect the features of nephrotic syndrome: high levels of proteinuria.
Microscopic hematuria that may occasionally be present.
Biochemical tests to evaluate kidney function, including serum creatinine, blood urea nitrogen (BUN), electrolytes, albumin levels, and a lipid profile, as hyperlipidemia is often associated with nephrotic syndrome.
Perform a urine protein-to-creatinine ratio to quantify the degree of proteinuria.
Imaging Studies
Ultrasound: Renal ultrasounds might reveal kidneys appearing brighter than normal (hyperechoic) with less clear distinction between the outer and inner layers (corticomedullary differentiation loss).
Abdominal Ultrasound: If necessary, an ultrasound of the entire abdomen can be performed to check for complications like blood clots in veins (venous thrombosis) or to exclude other reasons for protein in the urine.
Immunological and Serological Testing
Assess autoimmune markers, which includes:
Antinuclear Antibodies (ANA): To check for autoimmune diseases.
Anti-streptolysin O Titers (ASOT): To evaluate for past streptococcal infections.
Complement Components (e.g., C3): To assess the immune system’s complement pathway.
Cryoglobulins: To detect abnormal proteins that precipitate in cold temperatures.
Serum Electrophoresis: To look for monoclonal gammopathy, which can indicate certain blood disorders.
Kidney Biopsy
A kidney biopsy is performed if initial tests are not conclusive or to pinpoint the precise cause of nephrotic syndrome.
Microscopic examination of the kidney tissue (histological examination) can determine the specific type of glomerulonephritis or other kidney abnormalities causing the condition.
Additional Investigations
Genetic Testing: Consider if hereditary causes of nephrotic syndrome are suspected, especially in children or when there’s a family history of kidney problems.
Secondary Causes Assessment: Investigate potential underlying causes of nephrotic syndrome, including:
Tests for infections like hepatitis B and C, and HIV.
Diabetes management assessment (HbA1c test).
Evaluation for cancers if clinically indicated.
Treatment of Nephrotic Syndrome
Management Goals:
Reduce swelling (edema).
Correct low albumin levels in the blood (hypoalbuminemia).
Lower elevated blood pressure.
Decrease protein in the urine (proteinuria).
Prevent complications like infections, blood clots (thrombosis), and malnutrition.
Medical Management:
Diuretics: Loop diuretics, such as furosemide, are primary medications for managing edema. Thiazide diuretics, like hydrochlorothiazide, can be added for enhanced effect if needed.
Albumin Infusions: Albumin infusions might be considered to raise blood albumin levels and reduce edema, but are often avoided due to high cost.
ACE Inhibitors or ARBs: Medications like lisinopril (ACE inhibitors) or losartan (ARBs) are used to manage blood pressure and reduce protein loss in urine.
Corticosteroids: Prednisone is a common corticosteroid used, typically starting at 1-2 mg/kg daily and gradually decreased. Lack of improvement after 4 weeks of prednisolone treatment may indicate the need for a kidney biopsy.
Immunosuppressants: Drugs like cyclophosphamide are used for patients who don’t respond adequately to corticosteroids.
Statins: Statins, for example atorvastatin, are prescribed to reduce high cholesterol levels.
Antiplatelet Agents: Antiplatelet medications, such as aspirin, may be used to prevent blood clot formation.
Nutritional Support: A diet high in protein is crucial to prevent malnutrition.
Vitamin D and Calcium: Supplements might be necessary to prevent low calcium levels (hypocalcemia).
Antibiotics: Used to treat any infections that arise.
Vaccinations: Vaccination against pneumococcal pneumonia and influenza is recommended for nephrotic syndrome patients.
Nursing Interventions for Nephrotic Syndrome:
Fluid Volume Excess:
Elevate legs and feet to help fluid drain back towards the body’s core.
Monitor for signs of fluid overload, such as edema, fluid in the abdomen (ascites), and fluid around the lungs (pleural effusions).
Restrict fluid intake as directed by the doctor.
Administer prescribed diuretics like furosemide (Lasix) to increase fluid excretion.
Strictly track fluid intake and output and maintain accurate fluid balance records.
Daily weight monitoring to assess fluid status changes.
Ineffective Breathing Pattern:
Regularly assess respiratory status, including oxygen saturation, breathing rate, and breathing effort.
Position the child in a semi-upright (semi-Fowler’s) position or supported over a table with pillows to aid lung expansion.
Provide supplemental oxygen if prescribed to maintain adequate oxygen levels.
Encourage slow, deep breaths and relaxation techniques to ease anxiety and improve breathing patterns.
Administer bronchodilators if prescribed to open airways and reduce wheezing.
Risk for Infection:
Monitor for infection signs, such as fever, chills, and elevated white blood cell count.
Administer prescribed antibiotics to treat or prevent infections.
Practice rigorous hand hygiene and maintain aseptic technique when caring for the child and performing procedures.
Keep skin clean and dry to prevent skin infections.
Monitor nutritional status and ensure a diet rich in protein and vitamins to support the immune system.
Altered Nutrition: Less Than Body Requirements:
Provide small, frequent meals that are rich in protein and calories to meet increased nutritional needs.
Offer a variety of foods to encourage eating and prevent food aversion.
Consult a dietitian to create a tailored nutrition plan that meets individual needs and preferences.
Supplement diet with nutritional supplements as prescribed to ensure sufficient intake of essential nutrients.
Dietary Management of Nephrotic Syndrome:
Provide a balanced diet with sufficient protein (1.5-2 g/kg) and calories.
Limit fat intake to less than 30% of total calories, especially avoiding saturated fats.
Encourage a “no added salt” diet to minimize fluid retention.
Discourage sugary drinks and snacks to prevent weight gain and fluid overload.
Regularly monitor weight and adjust diet as needed to maintain a healthy weight.
Complications:
Monitor for complications like ascites, pleural effusion, generalized edema, blood clotting issues, thrombosis, recurrent infections, kidney failure, growth delays, and calcium and vitamin D deficiency.
Provide appropriate treatments and interventions for any complications that develop.
Educate the child and family about potential complications and the importance of regular follow-up care.
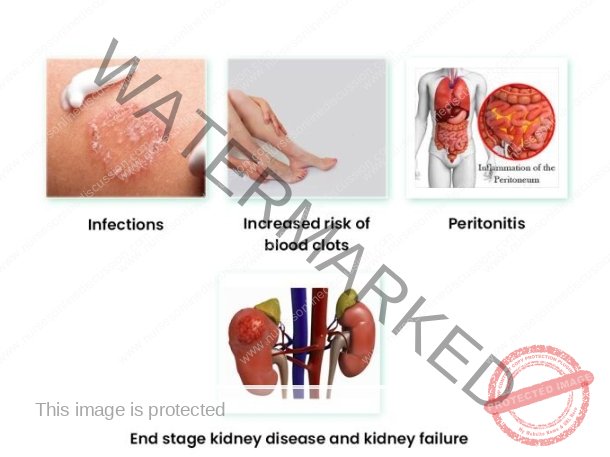
Complications of Nephrotic Syndrome:
Thromboembolic Disorders:
Cause: Decreased levels of antithrombin III (a protein that inhibits blood clotting). Antithrombin III is lost in the urine due to increased permeability of the glomerular basement membrane.
Result: Formation of blood clots in the veins (deep vein thrombosis) or arteries (pulmonary embolism).
Infections: Increased susceptibility due to:
Loss of immunoglobulins and other protective proteins in the urine.
Decreased production of white blood cells.
Impaired immune cell function.
Common Infections: Pneumonia, cellulitis, and peritonitis.
Acute Kidney Failure:
Cause: Decrease in blood volume (hypovolemia) due to fluid loss into the tissues (edema).
Result: Hypovolemia leads to decreased blood flow to the kidneys, potentially damaging them and causing acute kidney failure.
Pulmonary Edema:
Cause: Loss of proteins from the blood plasma, leading to a decrease in oncotic pressure.
Result: Decreased oncotic pressure allows fluid to leak out of the blood vessels into the lungs.
Hypothyroidism:
Cause: Loss of thyroxine-binding globulin (TBG), a protein that transports thyroid hormone in the blood.
Result: Decreased TBG levels lead to decreased levels of free thyroid hormone.
Vitamin D Deficiency:
Cause: Loss of vitamin D-binding protein, which transports vitamin D in the blood.
Result: Decreased vitamin D-binding protein levels lead to decreased levels of free vitamin D.
Hypocalcemia:
Cause: Loss of 25-hydroxycholecalciferol, the storage form of vitamin D.
Result: Decreased vitamin D levels lead to decreased calcium absorption from the intestines.
Microcytic Hypochromic Anemia:
Cause: Loss of ferritin, a protein that stores iron in the body.
Result: Decreased ferritin levels lead to decreased iron stores.
Protein Malnutrition:
Cause: Loss of protein in the urine exceeds the amount ingested.
Result: Can lead to weakness, fatigue, and impaired immune function.
Growth Retardation: (Primarily in Children)
Contributing Factors:
Protein malnutrition.
Anorexia (reduced appetite).
Steroid therapy (can suppress growth).
Cushing’s Syndrome:
Cause: Treatment with high doses of corticosteroids.
Mechanism: Overproduction of the hormone cortisol.
Potential Problems: Weight gain, high blood pressure, and diabetes.
Related Question of Nephrotic Syndrome
An adult male patient has been brought to medical ward with features of nephrotic syndrome
(a) List five cardinal signs and symptoms of nephrotic syndrome
(b) Describe his management from admission up to discharge.
(c) Mention five likely complications of this condition.
SOLUTIONS
(a) NEPHROTIC SYNDROME:
Is a syndrome caused by many diseases that affect the kidney characterized by severe and prolonged loss of protein in urine especially albumen, retention of excessive salts and water, increased levels of fats.
FIVE CARDINAL SIGNS AND SYMPTOMS:
Massive proteinuria.
Generalized edema.
Hyperlipidemia.
Hypoalbuminemia.
Hypertension.
(b) MANAGEMENT:
Aims of Management:
To prevent protein loss in urine.
To prevent and control edema.
To prevent complications.
ACTUAL MANAGEMENT:
Admit the patient in the medical ward male side in a warm clean bed in a well ventilated room and take the patient’s particulars such as name, age, sex, religion, status.
General physical examination is done to rule out the degree of oedema and other medical conditions that may need immediate attention.
Vital observations are taken such as pulse, temperature, blood pressure recorded and any abnormality detected and reported for action to be taken.
Inform the ward doctor about the patient’s conditions and in the meantime, the following should be done.
Position the patient in half sitting to ease and maintain breathing as the patient may present with dyspnoea due to presence of fluids in the pleural cavity.
Weigh the patient to obtain the baseline weight and daily weighing of the patient should be done to ascertain whether edema is increasing or reducing which is evidenced by weight gain or loss.
Monitor the fluid intake and output using a fluid balance chart to ascertain the state of the kidney.
Encourage the patient to do deep breathing exercises to prevent lung complications such as atelectasis.
Provide skin care particularly over edematous areas to prevent skin breakdown.
On doctor’s arrival, he may order for the following investigations.
Urine for culture and sensitivity to identify the causative agent.
Urinalysis for proteinuria and specific gravity, blood for;
Renal function test, it will show us the state of the kidney function.
Cholesterol levels; this will show us the level of cholesterol in blood.
Serum albumen; this will show us the level of protein or albumin in blood.
The doctor may prescribe the following drugs to be administered;
Diuretics, such as spironolactone 100-200mg o.d to reduce edema by increasing the fluid output by the kidney.
Antihypertensives such as captopril to control the blood pressure.
Infusion albumin 1g/kg in case of massive edema ascites and this will help to shift fluid from interstitial spaces back to the vascular system.
Plasma blood transfusion to treat hypoalbuminemia.
Cholesterol reducing medication to have the cholesterol levels in blood such as lovastatin.
Anticoagulants to reduce the blood ability to clot and reduce the risk of blood clot formation e.g. Heparin.
Immune suppressing medications are given to control the immune system such as prednisolone if the cause is autoimmune.
Antibiotics such as ceftriaxone to treat secondary bacterial infections.
The doctor may order for renal transplant if the chemotherapy fails.
Routine Nursing Care:
Continuous urine testing is done to see whether proteinuria is reducing or increasing.
Encourage the patient to take a deity rich in carbohydrates and vitamins but low in protein and salts.
Ensure enough rest for the patient as this will reduce body demand for oxygen and hence prevent fatigue.
Promote physical comfort by ensuring daily bed bath, change of position, oral care and change of bed linen.
Reassure the patient to alleviate anxiety and hence promote healing.
Ensure bladder and bowel care for the patient.
ADVICE ON DISCHARGE:
The patient is advised on the following:
To take a deity low in salt and protein.
Drug compliance.
Personal hygiene.
Stop using drugs like heroin, NSAIDs.
Screening and treating of diseases predisposing or causing the disease.
To come back for review on the appointment given.
(c) COMPLICATIONS:
Acute kidney failure.
Kidney necrosis.
Ascites.
Pyelonephritis.
Cardiac failure
Pulmonary embolism.
Atherosclerosis.
Deep venous thrombosis.
NEPHRITIC SYNDROME
Differentiation Between Acute Nephritic Syndrome and Nephrotic Syndrome
| Feature | Acute Nephritic Syndrome | Nephrotic Syndrome |
| 1. Proteinuria | Mild (less than 3 grams per 24 hours) | Heavy (more than 3 grams per 24 hours) |
| 2. Hypoalbuminaemia | Uncommon | Present |
| 3. Oedema | Mild, in loose tissue | Marked, generalized peripheral |
| 4. Mechanism of Oedema | Sodium and water retention | Reduced plasma osmotic pressure, Sodium and water retention |
| 5. Haematuria | Present, microscopic | Absent |
| 6. Hypertension | Present | Present in advanced disease |
| 7. Hyperlipidaemia | Absent | Present |
| 8. Lipiduria | Absent | Present |
| 9. Oliguria | Present | Present in advanced disease |
| 10. Hypercoagulability | Absent | Present |
Differentiation Between Nephrotic and Nephritic Syndrome: Typical Features
| Typical Features | Nephrotic Syndrome | Nephritic Syndrome |
| Onset | Insidious | Abrupt |
| Edema | ++++ | ++ |
| Blood pressure | Normal | Raised |
| Jugular venous pressure | Normal/low | Raised |
| Proteinuria |
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

