Urinary Disorders Affecting Children
Subtopic:
Nephritic Syndrome
NEPHRITIC SYNDROME.
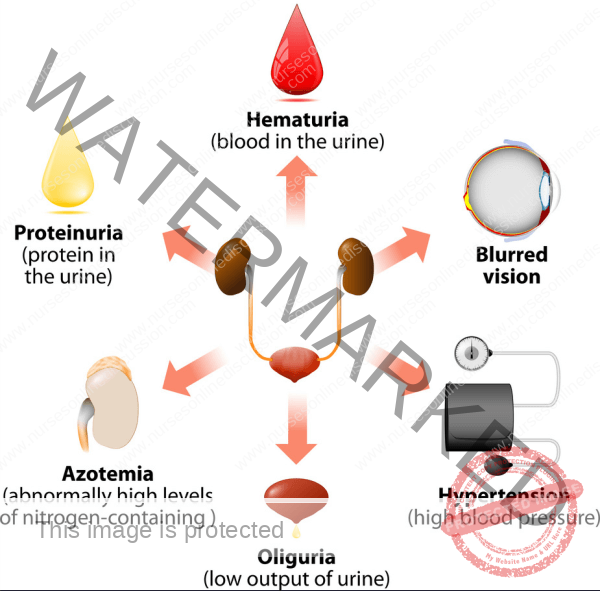
Nephritic syndrome is a medical condition defined by the rapid development of several key signs: the presence of blood in the urine (hematuria), protein in the urine (proteinuria), elevated blood pressure (hypertension), swelling (oedema), and decreased urine output (oliguria). This often emerges after a recent infection, typically occurring approximately 10 to 20 days afterwards.
Nephritic syndrome encompasses a spectrum of kidney diseases where the glomeruli – the kidney’s internal filtering units – become inflamed or swollen. This glomerular inflammation triggers the swift appearance of hematuria, proteinuria, hypertension, oedema, and oliguria.
Acute Nephritic Syndrome
Acute Nephritic Syndrome is characterized by a sudden injury or inflammation of the kidney’s glomeruli. It’s marked by symptoms including fever and the quick onset of blood in urine (haematuria), protein in urine (proteinuria), high blood pressure, and reduced urine production.
This condition is also commonly known as Acute Glomerulonephritis.
Signs and Symptoms
Historically, nephritic syndrome has been classically recognized by a triad of:
Hematuria: Presence of blood in urine. Typically, this is microscopic, only detectable under a microscope. However, in some instances, visible hematuria may occur, causing a pinkish or red urine discoloration.
Hypertension: Elevated blood pressure. This arises from the kidneys’ impaired ability to regulate bodily fluids and electrolyte balance.
Edema: Swelling in body tissues. This is due to the kidneys’ compromised function in removing excess fluid from the body.
Nephritic syndrome is further characterized by PHAROH:
P: Proteinuria (Proteins in urine): Small quantities of proteins are excreted in the urine, generally in a trivial amount (less than 3.5g/day).
H: Hematuria (Blood in urine): Slight hematuria may give the urine a smoky appearance.
A: Azotemia (Elevated blood Urea and Creatinine): This results from the body’s retention of waste products due to variable renal insufficiency.
R: Red blood cell casts: Presence of red blood cell casts in the urine.
O: Oliguria: Reduced urine output, typically less than 400ml/day.
H: Hypertension: High blood pressure, often mild in nephritic syndrome.
Other signs and symptoms of nephritic syndrome may include:
Nocturia: Frequent urination specifically during nighttime hours.
Fatigue: A sensation of tiredness or weakness, linked to the accumulation of metabolic waste products in the bloodstream.
Loss of appetite: Reduced desire to eat, also attributed to the buildup of waste products in the blood.
Nausea and vomiting: Indications of gastrointestinal disturbance. These symptoms are triggered by the accumulation of waste products in the blood.
Blurred vision: A visual disturbance associated with high blood pressure. It is caused by damage to the small blood vessels within the eyes.
Causes of Nephritic Syndrome
Nephritic syndrome arises from inflammation within the glomeruli, the kidney’s filtration units. This inflammation can harm the glomerulus, hindering its proper function and leading to an accumulation of waste substances in both the bloodstream and urine.
The origins of nephritic syndrome can be broadly classified into three main categories:
Infectious Causes: These represent the most frequent triggers of nephritic syndrome, particularly in children. These include:
Post-streptococcal glomerulonephritis: The most prevalent infectious cause in children. It develops following a recent streptococcal infection, such as strep throat or scarlet fever. The bacteria produce antigens that resemble components of the kidney’s glomeruli. The body’s immune system produces antibodies to combat the bacteria, but these antibodies mistakenly react with the glomeruli, triggering inflammation and injury.
Infective endocarditis/Bacterial endocarditis: An infection affecting the inner lining of the heart valves. Bacteria causing infective endocarditis can release antigens into the bloodstream, which subsequently deposit in the glomeruli. This can result in inflammation and damage to the glomeruli, ultimately causing nephritic syndrome.
Viral Infections: Certain viral infections, for example, hepatitis B and C, can also induce nephritic syndrome.
Hepatitis B glomerulonephritis: A specific type of glomerulonephritis caused by the hepatitis B virus. The virus can multiply within the glomerular cells, leading to inflammation and harm, which can progress to nephritic syndrome.
Systemic Lupus Erythematosus (SLE): A chronic autoimmune disorder impacting various organs, including the kidneys. In SLE, the body’s immune system produces autoantibodies that mistakenly target its own tissues. These autoantibodies can attack the glomeruli, causing inflammation and injury that can lead to nephritic syndrome.
Vasculitis: A condition characterized by inflammation of blood vessels. Vasculitis can affect blood vessels within the kidneys, resulting in inflammation and damage to the glomeruli.
Autoimmune Causes: These are conditions where the body’s immune system mistakenly attacks its own tissues. They include:
IgA nephropathy: The most common autoimmune cause of nephritic syndrome in adults. It is characterized by the deposition of IgA antibodies within the glomeruli.
Lupus nephritis: A kidney disease type induced by the autoimmune disorder lupus.
Goodpasture syndrome: A rare autoimmune condition that targets both the lungs and kidneys. It involves the body producing antibodies that attack the glomeruli and the alveoli of the lungs. This can lead to nephritic syndrome and pulmonary hemorrhage.
Serum sickness: A reaction to foreign proteins, such as those found in certain medications or vaccines. The body’s immune system generates antibodies to target these foreign proteins, but these antibodies can also cross-react with the glomeruli, causing inflammation and damage, potentially leading to nephritic syndrome.
Other Causes: These encompass:
Hemolytic Uremic Syndrome: A condition marked by the destruction of red blood cells, low platelet counts, and kidney failure. It can be triggered by specific infections, such as E. coli, or certain medications.
Henoch-Schonlein purpura: A condition characterized by a rash, joint pain, and kidney problems. It is caused by the deposition of IgA antibodies within the blood vessels.
Rapidly Progressive Glomerulonephritis: A rare condition that can lead to kidney failure rapidly, often within weeks or months. It is frequently caused by an autoimmune disease or infection.
Pathophysiology of Nephritic Syndrome
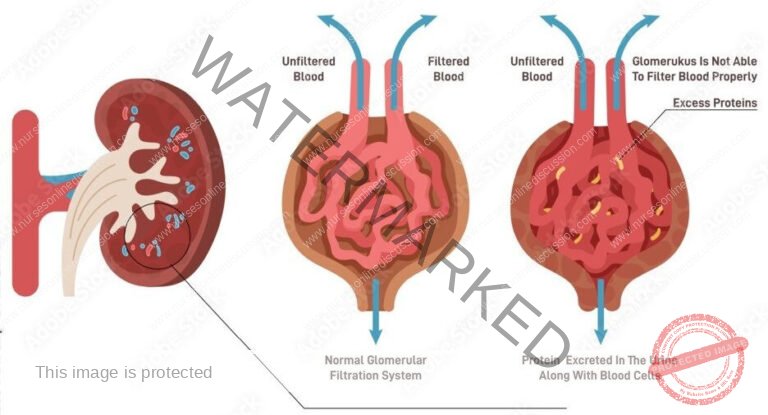
Nephritic syndrome stems from injury to the renal glomeruli. These glomeruli are delicate networks of blood vessels in the kidneys responsible for filtering waste and excess fluid from the bloodstream, ultimately forming urine that is transported to the bladder. This damage is frequently initiated by an immune system reaction, often following a streptococcal infection.
Inflammation impairs the glomeruli’s normal function. The glomeruli are crucial components of the kidney that regulate filtration and waste removal from the body.
Glomerular damage, resulting from inflammation triggered by streptococcal infection, increases the permeability of the glomerular filtration membrane. This heightened porosity allows smaller proteins and red blood cells (RBCs) to escape from the bloodstream and enter the urine.
Edema, or swelling, arises due to protein loss from the blood. Proteins are essential for maintaining fluid balance within blood vessels. When proteins are lost, fluid shifts out of the bloodstream and accumulates in body tissues, leading to swelling. Furthermore, the structural damage to kidney vessels also results in blood leaking into the urine.
Diagnosis of Nephritic Syndrome
Assessment: The diagnostic process for nephritic syndrome initiates with a comprehensive medical history review and physical examination. The physician will inquire about the patient’s symptoms, specifically noting the start and length of symptoms, along with any recent infections or illnesses. A physical examination will be conducted to identify signs such as edema (swelling), hypertension (high blood pressure), or other physical irregularities.
Laboratory Tests:
Urinalysis: This is a fundamental test involving the examination of urine to detect abnormalities. It is used to check for the presence of blood, protein, or casts, all of which are indicators of kidney dysfunction.
Blood Tests: Various blood tests are crucial for measuring the levels of electrolytes, urea nitrogen, and creatinine in the blood. These measurements are essential to evaluate kidney function and to differentiate from other conditions that might be causing the patient’s symptoms.
Creatinine Clearance Test: This specialized blood test is performed to assess the efficiency of the kidneys in filtering waste products from the blood. Creatinine, a waste byproduct of muscle metabolism, is normally removed by the kidneys, and this test measures how effectively this process is occurring.
Kidney Biopsy: In some cases, a kidney biopsy might be necessary. This involves obtaining a small tissue sample from the kidney for microscopic examination. This allows for direct visualization of the glomeruli to identify signs of inflammation or structural damage.
Streptococcal Serology: This test is specifically employed to detect antibodies against Streptococcal bacteria in the blood. It helps determine if the patient has had a recent Streptococcal infection, which is a frequent underlying cause of nephritic syndrome.
Imaging Tests:
Imaging Tests: Techniques like ultrasound or magnetic resonance imaging (MRI) may be utilized to visualize the kidneys. These imaging studies help to assess the kidneys’ structure and identify any abnormalities in their form or function.y
Management of Nephritic Syndrome
The majority of individuals with acute nephritic syndrome achieve complete recovery, though a small proportion may develop chronic conditions. Children generally fare better than adults, typically recovering fully, with chronic glomerulonephritis being a rare progression.
Aims of Management:
Preserve Renal Function: The primary goal is to protect and maintain the kidney’s ability to filter waste.
Reduce Inflammation and Edema: Strategies are implemented to minimize kidney inflammation and alleviate fluid retention (edema).
Prevent Complications: Measures are taken to avoid potential complications associated with nephritic syndrome.
1. Rest: Patient care involves complete bed rest in a comfortably warm and well-ventilated room. Bed rest is typically maintained until all prominent symptoms subside and urine is clear of red blood cells and, ideally, albumin. However, it’s noted that in some individuals, albuminuria might persist even as the condition transitions into a chronic phase; therefore, prolonged bed rest until complete normalization of urine may not always be practical or necessary.
2. Diet: Due to the crucial need to minimize stress on the affected kidneys, dietary management is paramount in treating acute nephritic syndrome. A diet that minimizes the kidney’s workload is recommended. This typically involves limiting protein intake to reduce the production of protein waste products. Adequate calorie intake, particularly from carbohydrates, is important to prevent body protein breakdown. In cases of edema, fluid and sodium intake are carefully restricted.
3. Intake and Output Chart: Meticulous monitoring of fluid balance is essential. An intake and output chart must be maintained for all patients. Regular urine examinations are conducted daily to monitor for albumin, red blood cells, and casts. Bowel regularity is maintained, often with the aid of a mild laxative if needed.
4. Prevention of Complications: Managing potential complications is a crucial aspect of care. Convulsions, observed in severe instances, are addressed with sedatives. In cases of significantly elevated blood pressure, rapid blood pressure reduction via rapid fluid withdrawal (e.g., approximately 500ml of blood) can be beneficial in reducing strain on the heart.
Medications:
Immune-system-suppressing medications: These medications, such as corticosteroids, are used to dampen the immune response and reduce kidney inflammation, particularly in cases associated with certain kidney disorders like membranous nephropathy and other autoimmune-related causes.
Adrenocorticosteroids: These are utilized specifically to reduce proteinuria (protein in the urine), a key characteristic of nephritic syndrome.
Diuretics: These medications are employed to manage edema by promoting fluid excretion from the body, thereby reducing swelling.
Antibiotics: If a bacterial infection is identified as the underlying cause or a secondary complication, antibiotics are administered to treat the infection.
Anticonvulsants: In cases where seizures (convulsions) occur, anticonvulsant medications are used to manage and prevent these neurological events.
Anticoagulants and antiplatelet drugs: Medications such as dipyridamole, indomethacin, urokinase, and cyproheptadine may be considered to help prevent the formation of blood clots, particularly in specific situations where there is a risk of hypercoagulability.
Other Treatments:
Restricting protein and sodium in the diet: Dietary adjustments to limit protein and sodium intake can lessen the kidney’s workload and aid in managing symptoms.
Fluid restriction: Carefully controlled fluid intake may be necessary to manage and prevent edema, especially when kidney function is compromised.
Dialysis: In severe cases where the kidneys are unable to adequately filter waste and maintain fluid balance, dialysis might be required to perform these essential functions artificially.
Nursing Management of Nephritic Syndrome:
Monitor vital signs: Regularly check and record the patient’s vital signs, including blood pressure, heart rate, and respiratory rate, to detect any changes and ensure stability.
Monitor intake and output: Accurately track the patient’s fluid intake and urine output to assess fluid balance and kidney function.
Daily weight monitoring: Weigh the patient daily. This is a critical indicator for assessing fluid retention and the effectiveness of treatment.
Assess skin for edema: Regularly examine the patient’s skin for signs of edema (swelling), noting the location and severity.
Monitor urine: Regularly assess the patient’s urine for the presence of protein, blood, and casts, which are indicators of kidney status and disease progression.
Administer prescribed medications: Give medications as ordered by the physician, ensuring correct dosage, route, and timing.
Patient education on diet and fluid restrictions: Educate the patient and family about the importance of adhering to prescribed dietary and fluid restrictions to manage symptoms and support kidney function.
Encourage rest: Promote rest and advise the patient to avoid strenuous activity to minimize kidney workload and facilitate recovery.
Provide emotional support: Offer emotional support to the patient and family, as dealing with a kidney condition can be stressful.
Monitor for complications: Closely observe the patient for signs and symptoms of complications such as convulsions, heart failure, and infection, and report any concerns promptly.
Skin care for pressure ulcer prevention: Provide meticulous skin care to prevent pressure ulcers, especially for patients on prolonged bed rest.
Frequent turning: Turn the patient frequently to prevent pneumonia and promote lung aeration, particularly for bedridden patients.
Assist with daily living activities: Assist the patient with activities of daily living as needed, considering their fatigue and limitations.
Patient education on follow-up care: Educate the patient about the importance of follow-up care and long-term management to monitor kidney health and prevent recurrence or progression.

Complications of Nephritic Syndrome
Nutritional Deficiencies: Protein loss in urine can result in malnutrition. This can manifest as unintentional weight loss, although this might be masked by fluid retention (swelling).
Elevated Blood Pressure: Damage to the glomeruli and the subsequent accumulation of waste products in the bloodstream (azotemia) can cause hypertension.
Sudden Kidney Failure: If the kidneys lose their ability to filter blood effectively due to glomerular damage, waste products can rapidly accumulate in the blood. In severe cases, emergency dialysis may be necessary.
Long-Term Kidney Failure: Nephritic syndrome can lead to chronic kidney disease, where the kidneys progressively lose their function over an extended period, potentially necessitating dialysis or a kidney transplant.
Increased Susceptibility to Infections: Children with nephritic syndrome are at a higher risk of developing infections, particularly skin infections and pneumonia.
Seizures: Severely elevated blood pressure as a result of nephritic syndrome can trigger seizures.
Brain Dysfunction (Encephalopathy): The accumulation of toxins in the blood due to kidney failure can lead to encephalopathy, a condition that affects brain function.
Stroke: Severe hypertension associated with nephritic syndrome can also elevate the risk of stroke.
Other Complications:
Fluid Overload: Excess fluid retention can lead to swelling in areas such as the hands, feet, and ankles.
Heart Failure: The strain on the cardiovascular system due to fluid overload and hypertension can contribute to heart failure.
Inflammation of the Pericardium (Pericarditis): Inflammation of the sac surrounding the heart can occur as a complication.
Anemia: Reduced red blood cell production or increased destruction can lead to anemia.
Growth Impairment in Children: In children, nephritic syndrome can negatively impact growth and development, causing growth retardation.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

