Anatomy & Physiology 2
Subtopic:
The Reproductive System
The Reproductive System
The reproductive role of male is to produce and deliver sperm to the female reproductive tract.But the reproductive role of females is to produce ova and carrying the developing embryo. The sex hormones play an important role both in the development and function of the reproductive organ and in sexual behavior & drives.
Male reproductive system
The male’s reproductive role is to produce sperm and deliver to the vagina. These functions require four different structures. These are the: Testes, Accessory glands, Accessory ducts and penis
Male internal reproductive organs
Male internal reproductive organs include the tastes, series of ducts and accessory glands.

TESTES
- Testes are paired male reproductive organs (gonads), which produce sperm. During fetal life, tests are formed just below the kidneys inside the abdomino-pelvic cavity. By third fetal month it stats is to descend and by the seventh month of fetal life it passes through the inguinal canal.
- The inguinal canal is a passageway leading to scrotum. Scrotum is a paunch of skin that hangs between the thighs.
- The tests complete their descent in to the scrotum shortly before or after birth. Because the tests hang in scrotum outside the body their temperature is of cooler than the body temperature by 3 Degree Fahrenheit. This lower temperature is needed for sperm production and survival.
- Under the skin of scrotum, Cremaster muscle elevates tests during cold weather. The interior of the scrotum is divided in to two by median septum. One tests in each compartment.
- Each test is oval-shaped measuring 4.5 c.m. long, 2.5 c.m wide in adults. It is enclosed in fibrous sac called Tunica Albuginea. The sac extends to divide the test in two lobules. Next to tunica albuginea is Tunica Vaginals, which is a continuation of membrane of abdomino-pelvic cavity.
- Each test contains 800 lightly coiled Semniferous Tubules which produce thousands of sperm each second.

The walls of the semniferous tubes are lined with germinal tissue. The germinal tissue contains two types of cells: spermatogenetic cell producing or developing the sperm cell and the sustentacular cell, which provide nourishment for the germinal sperm.
Between the semniferous tubules clusters of endocrine cells called interstitial endocrinocytes (Leydig cell) secret male sex hormone (Androgens) where testosterone is the most important.
Sperm
The male genetic carrying cell is the sperm. Matured spermatozoa have head, middle piece, and tail
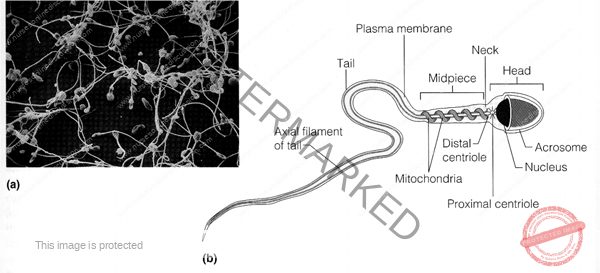
At the tip of the head is acrosome containing several enzymes that help the sperm to penetrate the egg? In the center of head is a nucleus-containing chromosome. This is a genetic constitution. The middle piece consist mainly coiled mitochondria for energy production for tail motility.
Sperm is one of the smallest cells in the body. For complete development each sperm need 2 months. Normally 300 to 500 million sperms are released during ejaculation. A male who releases 20 to 30 million normal sperms tends to be infertile.
Accessory Ducts
The sperm produced in the testes are carried to the point of ejaculation from penis by a system of ducts. These are epididymis, ductus defference, ejaculatory duct and the urethra.
Epididymis: – The semniferous tubules merge in the central posterior portion of the testes as epydidimis. Semniferous become straight opens into Tubules tubule (Tubule Recti) network of tube (Rete Testes) drain in to 15-20 tubes called Efferent ducts.
The efferent ducts extend upward in to a convoluted mass of tubes that forms a crescent shape along its side. This coiled tube is epididymis. It has three main functions.
– Store sperm until maturity
– Passage way of sperm
– Propel sperm to next duct system
Epididymis has head, body & tail. The head join with efferent duct and tail continues as vas deference (ductus deference).
Ductus deferens:
It is the dilated continuation of epididymis. It is located easily over the spermatic cord; hence male permanent (surgical) contraceptive method (vasectomy) is usually performed over it. As it passes from tail of epididymis it is covered by spermatic cord containing testicular artery, vein, autonomic nerves, lymphatic and connective tissue.
After the ducts deferens pass through the inguinal canal, it free from spermatic cord and pass behind the urinary bladder, where it travels alongside an accessory gland, the seminal vesicle and becomes ejaculatory duct. Just before reaching the seminal vesicle, it widens in to an enlarged portion, Ampulla.
Ampulla is sperm storage sites before ejaculation. It transports sperm by peristalsis during peak stimulation.
Ejaculatory duct:
The ducts deference joins to the duct of seminal vesicle at ejaculatory duct. It is about 2 c.m. long. They receive secretion from the seminal vesicles and pass through the prostate where they receive additional secretion.
Urethra
It is the final section of the reproductive system. It leads from the urinary bladder through the prostate gland and to the tip of the penis. Its reproductive function is to transport semen out of penis.
Accessory Glands:
These are seminal vesicles, prostate and bulbo-urethral glands.
Seminal vesicles
Seminal vesicles are paired; secretary sacs lie next to the ampulla of the ducts of vas deferens. It produces alkaline secretion.
It contains mostly water, fructose, prostaglandin & vit. C.
Prostate gland
Prostate gland lies inferior to the urinary bladder surrounding the first portion of urethra. It is a rounded mass about the size of chestnut. The secretion of prostate makes sperm motile and neutralizes vaginal acidity. A thin but firm capsule of fibrous connective tissue surrounds the prostate. The secretion of prostate mainly contains water, acid phosphate & cholesterol.
Bulbo-uretheral gland
Bulbo urethral glands are pair; one in each side of the urethra.
Each gland is about shape & size of pea. They lie directly below prostate. Bulbo urethral glands secrets clearly alkaline fluid to neutralize the acidity of urine during the onset of sexual excitement and it also act as a lubricant.
Male external reproductive organ
Penis
Penis is an extension from the perineal area of male. It is soft and erective tissue.
Has two main functions, it carries urine through urethra to the outside during urination and it transports semen through the urethra during ejaculation. In addition to urethra penis contains three cylindrical strands of erectable tissue.
– Two corpora cavernosa, which run parallel to the dorsum of penis.
– Corpus spongiosum which contain urethra
The corpora cavernosa is surrounded by a dense, relatively inelastic connective tissue called tunica albuginea. It also contains numerous vascular cavities called venous sinusoids.
Penis (draw the structure of the penis)
The corpus spongiosum extends distally beyond the corpora cavarnosa & becomes expanded at the tip of the penis, which is called glans penis. The loosely fitting skin of the penis is folded forward over the glans to form the prepuce or foreskin, which usually excised during circumcision. Corona of the glans is a ridge at behind margin of glans.
Semen
Secretions from epididymis, seminal vesicles, prostate and bulbourethral gland together with sperm make up semen.
Sperm make up only 1% of semen. The rest is a fluid secretion from accessory glands, which provide fructose to nourish sperm and alkaline medium to neutralize urethral (acidity because of urine) & vaginal acidity. It also contains vitamin C, and trace elements like calcium, Zinc, magnesium, Copper and sulfur.
Hormonal regulation in the male
Follicular Stimulating Hormone (FSH) and Leutinizing Hormone (LH) produced by the anterior pituitary gland are chiefly responsible for stimulating spermatogenesis and testosterone secretion. Follicular Stimulating Hormone (FSH) and Leutinizing Hormone (LH) affect only tests whereas;
Testosterone affects not only spermatogenesis but also sex organ development and appearance of secondary male sexual characteristics.
Female Reproductive System
The reproductive role of females is far more complex than that of male. They
– Produce egg
– After fertilization they also carry and protect the developing embryo.
– Production of milk by mammary glands
The female reproductive system consists of overlies, uterine tube, uterus, vagina, external genital organ (vulva) and mammary gland.
Female’s External reproductive organs:
This includes mons pubis, labia majora, labia minora, vestibular glands, clitoris and vestibule of vagina, which collectively called vulva.

Mound of fatty tissue covers symphysis pubis. It is covered with hair at puberty.
Labia majora:
Labia majora are two longitudinal folds of skin that forms the outer border of vulva. It contains fat, smooth muscle, areolar tissue, sebaceous glands & sensory receptors. At puberty covered with hair.
Labia minora:
Labia minora is a smaller fold of skin that lies between the labia majora. Labia minora and labia majora surround vaginal & urethral orifices. The labia merge at the top to form the foreskin or prepuce called the clitoris.
The clitoris:
Clitoris is a small erectile organ at the upper end of vulva below the mons pubis, where the two folds of labia minora meet. Like the penis it contains many nerve endings, hence it is very sensitive part.
The vestibule:
Vestibule is a space between the labia minora. Its floor contains the greater vestibular glands and the opening for the urethra & vagina. During sexual arousal the greater and lesser vestibular gland secrete alkaline mucous for lubrication to aid penetration.
Perineum
Perineum is a diamond shaped region bounded anteriorly by symphysis pubis, posteriorly by coccyx and laterally by ischeal tuberosity.
Female’s internal reproductive organs
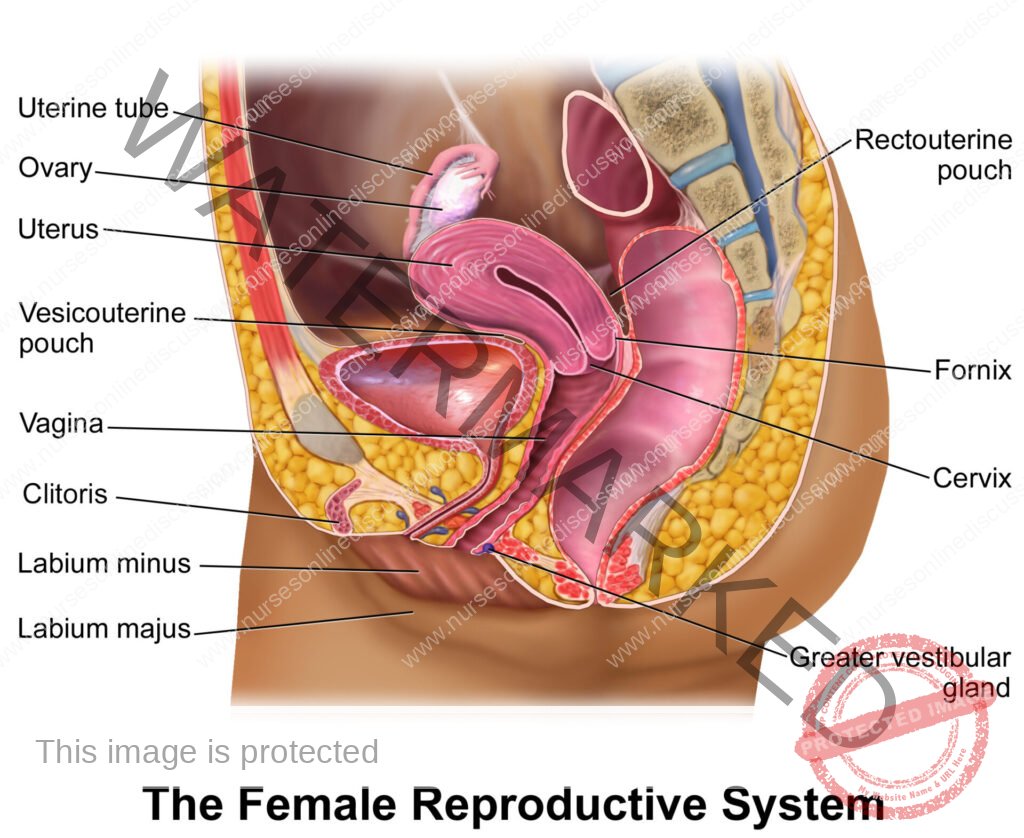
Females’ internal reproductive organs include the ovary, the uterine tube, the uterus, and the vagina.
Ovaries
Ovaries are females’ gonads that produce ova and female hormones. It is about the size of unshelled almond. The ovaries are located in the pelvic cavity one in each side of the uterus. Each ovary is attached by a mesentery called mesovarium to the backside of each broad ligament.
A thickening border of the mesovarium called ovarian ligament extends from the ovary to the uterus. The ovary is suspended from the pelvic wall by the suspensory ligament.
A layer of specialized epithelial cells called germinal layer covers the ovaries. Beneath it is the storma mass of connective tissue, which contains ova in various stage of maturity.
A cross section of ovary reveals a cortex and a vesicular medulla. The cortex contains round epithelial vesicle or follicles; follicles are actual center of ovum production or oogenesis. Follicles are usually located directly beneath the cortex of the ovary, they secret estrogen. But once they begin to mature they migrate towards the inner medulla.
The medulla consists of layers of soft stormal tissue. The stormal tissue contains rich supply of blood vessels, nerves and lymph useless.
After ovulation the lining of the follicles grow in ward, forming corpus luteum (yellow body), which temporary function as endocrine tissue. It secret estrogen & progesterone which stops additional ovulation, thickening of uterine wall & stops additional mammary glands in anticipating prognoses.
If pregnancy does not occur within 14 days corpus luteum degenerates and ministration follows. If pregnancy occurs, it continues to work for 2 to 3 months & eventually degenerate when placenta takes the duty.
The Ovary:
Ovulation
Ovulation is the process by which the mature ova rapture from the follicle and eventuality travel to the fallopian tube. In response to high concentration of FSH & LH from anterior pituitary, the mature follicle raptures this process. About 20 ovarian follicles mature each month beginning at puberty. However, only one raptures to release ova (oocyte).
Uterine tubes:
Uterine tubes are a pair of tubes one in each side of the uterus. The uterine tube (fallopian tube conveys the oocyte to the uterus. One of the paired tubes receives the oocyte from the ovary to take to the uterus. The tubes are not directly connected to ovary. But it open in abdominal cavity very close to ovary.
It has 3 distinct portions;
– Infundibulum: – funnel shaped, near the ovary
– Ampulla: – thin-walled middle portion
– Isthmus: – opens in to the uterus
The tube is made of three layers, the outer serous membrane, the middle muscular (smooth muscle) and the inner mucous membrane.
The Infundibulum is fringed with feathery fimbrea, which may over lapse the ovary. Unlike sperm the oocyte is unable to move by its own instead it is carried along the uterine tube towards uterus by peristaltic contraction of the fallopian tube.
Uterus:
The uterine tubes terminate in the uterus. A hallow muscular organ located in front of the rectum and behind the urinary bladder. It is like an inverted pear when viewed anterior and is pear size as well, during pregnancy it increases 3-6 times.
Round ligament help the uterus tilted forward over the bladder. It is attached to the lateral wall of the pelvis by two broad ligaments. Two utero-sacral ligaments extend from the upper part of the cervix to the sacrum. The posterior & anterior ligaments attach uterus to rectum and urinary bladder respectively.
Uterus has three parts:
– Fundus: – the upper, doom shaped part
– Body: – the tapering middle portion
– Cervix: – the body terminates to narrow portion
The constricted region between the body and cervix is the
Isthmus: – The interior of the cervix is the cervical canal, which opens in to vagina.
Uterus:
The uterus is made up of three layers of tissue. The outer serosa layer, the middle muscular layer called myometrium which make the bulky uterine wall composed of 3 layers of smooth muscle and the innermost, composed of specialized mucous membrane, endometrium. The endometrium contains abundant blood supply. It is composed of two layers. These are stratum functionalis that shed during every menstruation and if pregnancy occurs it continues to be site of attachment and nourishment for morrula (fertilized zygote) and the second layer of endometrium is stratum basale that attaches to myometrium.
Vagina:
A muscle lined tube 8 to 10 c.m long. It is the site where semen deposits during sexual intercourse; it is a canal for menstrual flow and a birth canal during childbirth.
It lies behind urinary bladder and rectum & anterior to rectum and anus. Its wall is mainly composed of smooth muscle & fibroelastic connective tissue. It is lined with mucous membrane containing many rugae. Stratified squamous non-Keratinized epithelium covers the mucosal layer of the vagina.
The mucous that lubricates the vagina comes from glands in the cervix and the acidic environment is because of the fermentation action of bacteria. A fold of vaginal mucosa called hymen that partially blocks the vaginal entrance in virgin.
Mammary Glands:
Within the paired breasts of women are modified sweat glands that produce and secrete milk. Each breast extends from the lateral surface of sternum to middle of axilla. It is held in place by suspensory ligaments of breast.
The amount of adipose tissue matters the size of the breast not the mammary cells. Each breast is composed of 15-20 lobes of areolar gland that radiate from the nipple.
This cluster of glands with lactiferous ducts that carry milk from the gland look like bunches of grapes. Lactiferous sinuses are dilated portion of lactiferous ducts. Areola is the pigmented area around the nipple. It enlarges & darkness during pregnancy.
Breast and mammary glands:
Hormonal regulation
Females are fertile a few days each month by the action of Gonadotrophin Realizing Hormone (GnRH) and FSH & LM.
In pregnant women additional hormone called Human Chorionic Gonadotrophin (HCG), which affects uterine and other body metabolism is released by placenta.
Gametogenesis:
Gametogenesis is the process of formation of sex cells. It is said spermatogenesis in male & oogenesis in females. Both involve meiosis, a form of nuclear division.
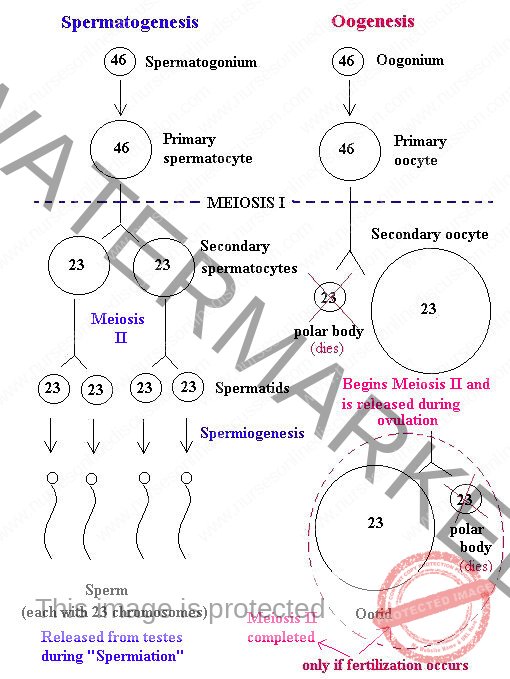
Gamete production in males begins at puberty and continues throughout life, but the situation is quite different in females. Female’s total supply of eggs is already determined by the time she is born, and the time span during which she releases them extends from puberty to menopause (about the age of 50)
Meiosis, specialized nuclear division that occurs in the testes to produce sperm, also occurs in the ovaries. In this case female sex cells are produced, and the process is called oogenesis (the beginning of an egg). The process of oogenesis takes years to complete.
First, in the fetal period the oogonia, the diploid stem cells of the ovaries multiply rapidly by mitosis and, then enter into a growth phase and lay in nutrient reserves. Gradually primordial follicles begin to appear as the oogonia are transformed into primary oocytes and become surrounded by a single layer of flattened follicle cells.
The primary oocyte begins the first meiotic division, but become “stalled” late in prophase I and do not complete it. By birth, a female has her life time supply of primary oocytes; of the original 7 million oocytes approximately 2 million of them escape programmed death and are already in place in the cortical region of the immature ovary.
At puberty, perhaps 400,000 oocytes remain and beginning at this time a small number of primary oocytes are activated each month. However only one is “selected” each time to continue meiosis I, ultimately producing two haploid cells (each with 23 replicated chromosomes) that are quite dissimilar in size. The smaller cell is called the first polar body. The larger cell, which contains nearly all the cytoplasm of the primary oocyte, is the secondary oocyte.
Oogenesis begins before birth and is not completed until after fertilization. Oogenesis begins when oogonia (singular, oogonium), which are the immature eggs that form in the ovaries before birth and have the diploid number of chromosomes, undergo mitosis to form primary oocytes, also with the diploid number.
Oogenesis proceeds as a primary oocyte undergoes the first cell division of meiosis to form secondary oocytes with the haploid number of chromosomes. A secondary oocyte only undergoes the second meiotic cell division to form a haploid ovum if it is fertilized by a sperm. The one egg cell that results from meiosis contains most of the cytoplasm, nutrients, and organelles.
This unequal distribution of materials produces one large cell and one cell with little more than DNA. This other cell, known as a polar body, eventually breaks down. The larger cell undergoes meiosis II, once again producing a large cell and a polar body. The large cell develops into the mature gamete, called an ovum. The unequal distribution of the cytoplasm during oogenesis is necessary as the zygote that results from fertilization receives all of its cytoplasm from the egg. So, the egg needs to have as much cytoplasm as possible.
Conception
Conception is the process of fertilization and subsequent establishment of pregnancy. Pregnancy begins with fertilization of an ovum and ends with delivery of the fetus after birth. When sperm is deposited in the vagina, the many spermatozoa wriggle about in all direction. Some travel in to the uterus and oviduct to meet the ova. If ova and sperm join this is called fertilization. From the day of fertilization on wards pregnancy starts.
Contraception
Contraception means protection. It has one aim, preventing pregnancy. This aim can be achieved by preventing sperm or ova not to function. It can be achieved by:
– Preventing production
– Preventing meeting of sperm & ova
– Preventing implantation
Several methods are available, but can be grouped in to permanent & temporally methods.
Permanent methods: in this type of contraception, once the method is used fertility is not possible. The usual method is surgery. The type of surgery in females is called Tubal-ligation whereby both fallopian tubes are ligated and transmission of the released ova from the ovary to the uterus is prevented.
And in males the surgical intervention for the purpose of contraception is called vasectomy.
In this case both vas deferens are cut or ligated and after production the transmission of sperm from the testes to the tip of the penis is prevented.
Temporary methods: condoms, tablets, Intra Uterine Devices
(IUD’s), calendar methods and others. These types of contraception are reversible types. This means fertility is possible if the person no longer uses the method.
Summary of major reproduction hormones
Hormone Function Source
FEMALE
Estrogen Stimulates thickening of uterine wall, stimulates maturation of oocyte, stimulates development of female sex characteristics, inhibits FSH secretion, increases LH secretion.
Ovarian follicle, corpus luteum (controlled by FSH)
FSH (follicle-stimulating hormone)
Causes immature oocyte and follicle to develop increases estrogen secretion, stimulates new gamete formation and development of uterine wall after menstruation.
Pituitary gland (controlled by hypothalamus)
GnRH (Gonadotrophin Releasing Hormone) Controls pituitary secretion. Hypothalamus
HCG (Human Chorionic Gonadotropin)
Prevents corpus luteum from disintegrating, stimulates estrogen and progesterone secretion from corpus luteum.
Embryonic membranes placenta LH (luteinizing hormone) Stimulates further development of oocyte and follicle, stimulates ovulation, increases progesterone secretion, aids development of corpus luteum.
Pituitary gland (controlled by hypothalamus)
Progesterone Stimulates thickening of uterine wall stimulates formation of mammary ducts.
Corpus luteum (controlled by LH)
Prolactine Promotes milk production by mammary glands after child birth
Pituitary gland (controlled by hypothalamus)
MALE
FSH
Increases testosterone production, aids sperm maturation
Pituitary gland (controlled by hypothalamus)
GnRH Controls pituitary secretion. Hypothalamus Inhibits FSH secretion Sustentacular (sertoli) cell of Testes
LH Stimulates testosterone secretion Pituitary gland (controlled by Hypothalamus)
Testosterone Increases sperm production, stimulates development of male primary and secondary sex characteristics, and inhibits LH secretion.Interstitial endocrinocytes (Leydig cells) in testes (controlled by
LH)
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

