Hematologic Disorders
Subtopic:
Anaemia
Table of Contents

Anaemia Definition
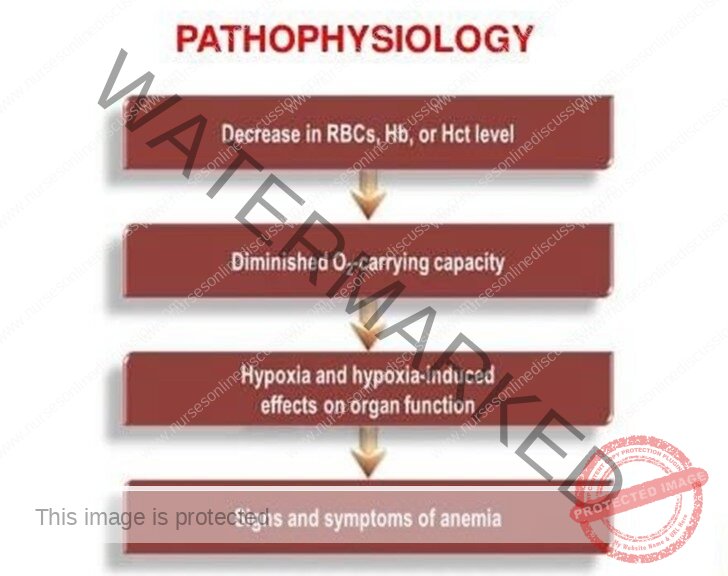
- An=Without; aemia=blood. (Anaemia=without blood)
- Therefore anaemia is a decrease in the RBC count, haemoglobin and/or hematocrit values resulting in a lower ability for red blood cells to carry oxygen to body tissues.
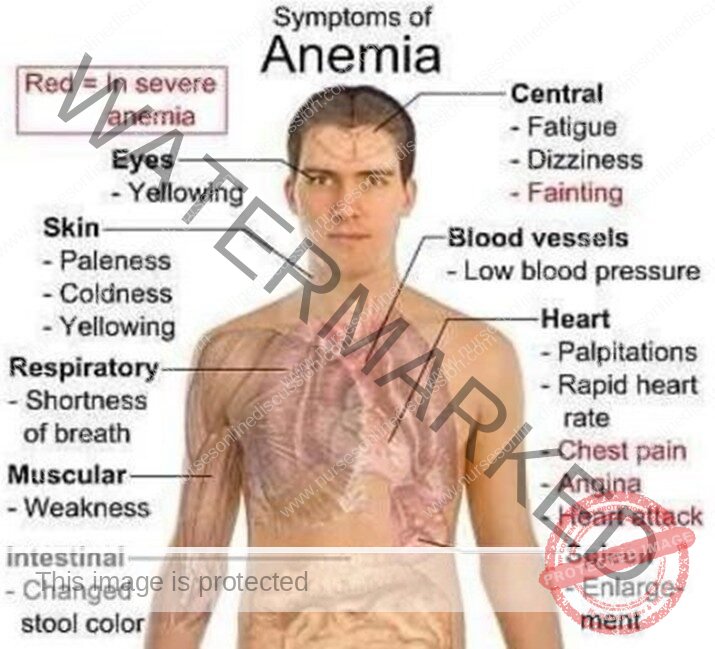
Clinical features of anemia, which include:
- Lassitude
- Fatigue
- Palpitations
- Breathlessness on exertion
- Dimness of vision
- Insomnia
- Angina
- Tingling sensation
- Pallor of the skin, mucous membranes, and conjunctiva
- Tachycardia
- Systolic murmur
- Oedema
- Amenorrhea
- Menorrhagia
- Attacks of giddiness
- Headache
- Drowsiness
- Flatulence of the abdomen after eating
Anaemia Classification
- Anaemia can be classified based on;
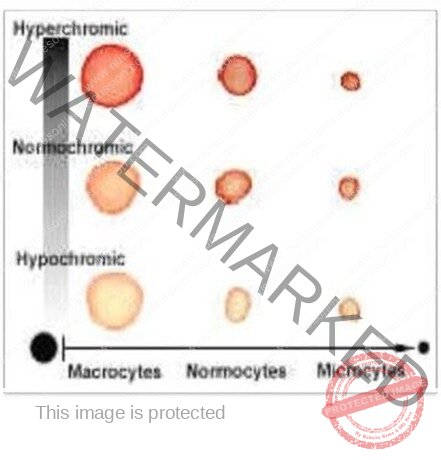
1.The morphological (shape and size) changes of the RBC in comparison with the normal shape and size of the RBCs. These can be;
- Normocytic (normal size of RBCs)
- Microcytic (smaller RBCs)
- Macrocytic (larger RBCs)
Based on the haemoglobin concentration in each RBCs anaemia can be;
- Normochromic (normal amount of haemoglobin).
- Hyperchromic (much concentration of haemoglobin)
- Hypochromic (little concentration of haemoglobin)
- These changes can be identified when a peripheral film is done
The cause of anaemia
Classification/types of anaemia based on the cause
- Iron deficiency anaemia; due to little iron in the body.
- Iron is an important component of haemoglobin which is the major oxygen carrying component in RBCs. Therefore its deficiency results into reduced ability of the RBCs to carry oxygen.
- Most common causes of iron deficiency in the body;
- Low dietary intake of iron.
- Decrease in iron absorption; as in gastectomy, intestinal malabsorption.
- Increase body demand of iron as in pregnancy, growing age, lactating mother, menstruating females.
- Chronic blood loss; such as in excessive or prolonged menstrual blooding, chronic gastrointestinal bleeding ( as in chronic use NSAIDs, large bowel tumors).
Sources of iron;
- Non-vegetarian food, like liver, kidney, egg-yolk, meat, fish fat.
- Vegetarian food like, dark green vegetables like spinach, green leafy vegetables fruits like dates, bananas, apples.
- Iron absorption across the lumen of the GIT is increased by HCL and Vit-C and decreased by milk and antacids.
Iron deficiency
Specific symptoms;
- Sored tongue
- Atrophy of the lingual papillae Brittle, fragile finger nails.
- Erosions of the corners of the mouth
Treatment;
- Dietary iron supplement
- Oral ferrous sulphate or ferrous sulphate /folic acid
- Antihelminthics (deworming) like albendazole
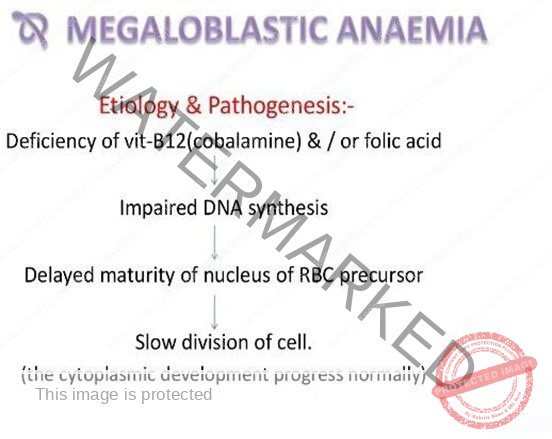
Megaloblastic anaemia/pernicious anaemia
- This type of anaemia is due to deficiency of vit-B12 and/or folic acid. Both Vit-B12 and folic acid are important for maturation and condensation of the DNA in RBCs. Their deficiency results into abnormally large RBCs and of fewer number. The deficiency in Vit-B12 usually is due to autoimmune destruction of the intrinsic factor (the intrinsic factor is a molecule that aids the absorption of Vit-B12 in the GIT). Vit-B12 and folic acid are also important for the development of nerve cells, their deficiency cause neuropsychiatric disorders.
Causes
Vitamin B-12 Deficiency due to;
1.Inadequate Dietary Intake
- More common in vegetarians and breastfed babies.
2. Malabsorption
- Due to lack of intrinsic factor.
- Gastrectomy.
- Diseases of the small intestine (e.g., Crohn’s disease).
3. Increased Demand
- Occurs in pregnancy.
- Lactation.
- Infancy.
Source
- Non-veg food like kidney, liver, heart, muscle meat, etc., are rich in B12.
- Fish, egg, cheese, and milk also rich in B12.
- Vegetables are poor in source (B12).
Daily requirement: 2-4µg
Absorption: In distal ileum.
Storage
- Mainly in liver → 2 mg
- Kidney
- Heart
- Brain
Folic Acid Deficiency
Similar to B-12 deficiency.
Causes of Folic Acid Deficiency:
- Inadequate dietary intake – More common in vegetarians and breastfed babies.
- Malabsorption – Due to lack of intrinsic factor, gastrectomy, disease of the small intestine like Crohn’s disease.
- Increased demand – Occurs in pregnancy, lactation, infancy, etc.
Megaloblastic anaemia
Specific features of Vit B12 deficiency;
- neuropsychiatric abnormalities e.g., impaired vibration and position sense, abnormal gait, weakness, decreased muscle strength, spastic motions, memory loss, disorientation, depression, and acute confusional state.
Specific treatment
- Dietary modification to ensure adequate intake of Vit B12and F/A, like advise patients to eat plenty of green leafy vegetables, and food of animal origin.
- F/A and Vit B12 supplementation; eg
- Folic acid: 5 mg daily until haemoglobin levels return to normal
- Vitamin B12: 1 mg IM daily for 5 days; then weekly for a further 3 doses – Followed with 1 mg every second month for life in patients with pernicious anaemia.
NOTE: Incase Vit B12 deficiency, F/A is not given alone as it may cause permanent neurological damage.
Aplastic Anaemia
- This type of anaemia is caused by failure of the bone marrow to produce enough or mature RBCs. The bone marrow has haematopoetic stem cells that are responsible for synthesizing all the blood cell lines (RBCs, WBCs &platelets).
- Aplastic anaemia is characterized by pancytopenia (reduction in all blood cells);
- Anaemia (low RBCs)
- Leucopenia (low WBCs)
- Thrombocytopenia (low platelets)
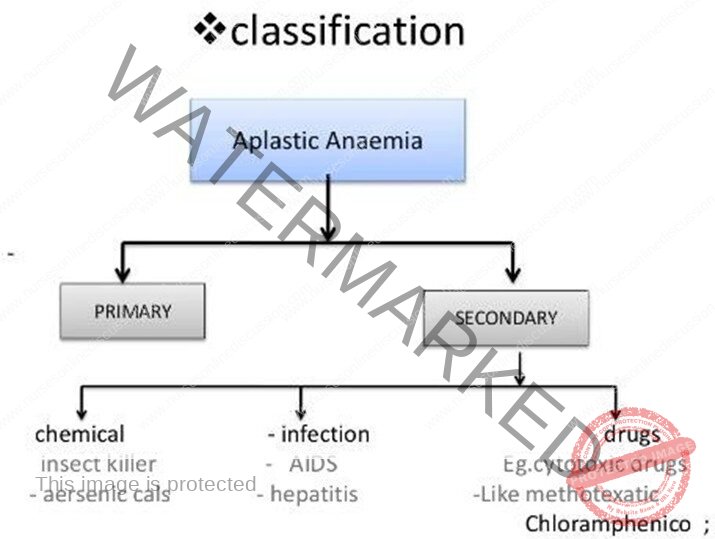
Aplastic anaemia
Causes of aplastic anaemia;
- Exposure to radiation and chemotherapy (cancer) treatment.
- Toxic chemicals; pesticides, insecticides, benzene (plane fuel).
- Use of some drugs;
- Autoimmune disorders; in which the bone marrow is attacked and destroyed by immune cells.
- Viral infections, such as Epstein Barr virus (EBV), Cytomegalovirus (CMV)
- In some cases its idiopathic (no known cause).
- Specific clinical features; purplish or red spots (petechiae and purpura), nose and gum bleeding, frequent infections, fever, fatigue and dizziness.
- Specific diagnostic investigations; Bone marrow biopsy (a small piece of bone is taken off for analysis under a microscope), a complete blood count (to check the level of all the blood cells).
- Specific treatment; blood transfusion (usually whole blood), stem cell (bone marrow) transplant, immunosuppresants, antibiotics, anti-virals.
Haemorrhagic Anaemia
- This is anaemia due to blood loss (haemorrhage). The degree/severity of anaemia depends on the severity of blood loss. It can be;
- Acute haemorrhagic anaemia, as in accidents, surgery, Ante-partum haemorrhage (APH) and post-partum haemorrhage (PPH). This is of sudden onset usually severe and life threatening.
OR
- Chronic haemorrhagic anaemia, as in bleeding peptic ulcers, pile (haemorrhoids), worm infestations in the gut, intestinal malignancies, epistaxis. This anaemia tends of occur episodically, usually less severe.
Haemolytic Anaemia
This anaemia occurs due to increased destruction/ breakdown of RBCs (hemolysis), at a rate faster than the body can replace them. It can be;
- Intracorpurscular haemolytic anaemia; in which the problem is within the RBCs either their membrane or haemoglobin, hence resulting into a reduced life span. Examples of this type anaemia are;
- Sickle –cell anaemia; the RBCs adopt a sickle shape other than their normal biconcave shape, hence break easily.
- Thalassemia; genetic disorder in which there are few haemoglobin chain, hence the oxygen carrying capacity becomes reduced. There are two type beta-thalassemia and alpha thalassemia depending on which type of haemoglobin chain is affected.
- Enzymatic deficiency in RBCs; such as G-6-PD (glucose-6-phosphate dehydrogenase) deficiency and PK (phosphokinase)deficiency. Without these enzymes, the RBC membrane becomes fragile and breaks.
- Hereditary spherocytosis,; in this type the RBC membrane is abnormal and becomes spherical in shape, hence breaking easily.
Haemolytic anaemia
OR
- Intracorpurscular; in which the problem is not with RBCs, but rather external and causing the RBCs to be destroyed at a faster rate. The causes of this include;
- Infections; bacterial, protozoan eg malaria etc.
- Haemolytic disease of the new bone; in which maternal antibodies enter foetal blood and cause RBC destruction.
- Blood transfusion reactions; as a result of transfusing incompatible blood type of the patient.
- Some drugs.
Diagnosis of anaemia
- Usually anaemia can be diagnosed by clinical features;
- Based on history of; trauma resulting into blood loss, infections such as severe malaria etc.
- Based on physical examination; such as pallor of the mucous membrane
- Diagnostic investigations such as;
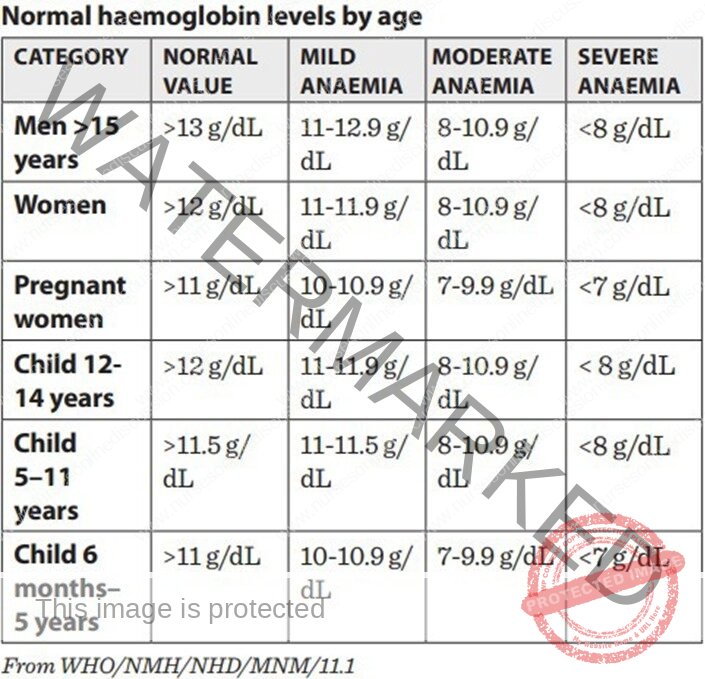
- CBC (complete blood count); to check of RBC number, Hb level and hematocrit
- Peripheral blood film to comment on the red blood cell indices, in order to determine the type of anaemia.
General management of anaemia
- The management depends on the cause and severity of anaemia, however generally;
- Haematinics,
- eg ferrous sulphate, iron sucrose, iron sulphate, folic acid etc. can be given especially in mild to moderate or resolving anaemia.
- Blood transfusion; with blood products.
- Blood products, are blood components that are that are prepared and made safe for therapeutic purposes, these are whole blood (WB), packed red blood cells (PCs), fresh frozen plasma (FFP), platelets these can be given differently as per the type of anaemia.
Related Topics
List of Topics
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

