Communicable disease
Subtopic:
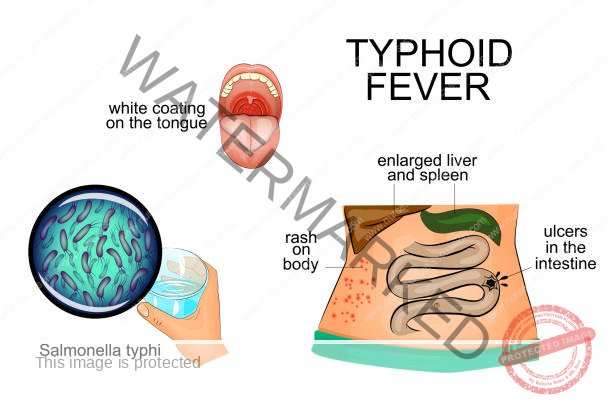
Typhoid fever
Definition:
Typhoid fever, also known as enteric fever, is an acute systemic illness caused by the bacterium Salmonella Typhi. It is characterized by a sustained high fever and is primarily transmitted through the ingestion of food or water contaminated with fecal matter from infected individuals.
Etiology (Causes):
Primary Cause: Salmonella Typhi is the primary causative agent of typhoid fever.
Related Organisms: Salmonella Paratyphi A and B can cause paratyphoid fever, a milder form of enteric fever with similar symptoms.
Relationship to Other Infections:
Enteric Fever: Typhoid fever is a specific type of enteric fever. Enteric fever refers to a febrile inflammatory reaction in the intestines caused by bacteria.
Salmonellosis: Typhoid fever is a specific type of salmonellosis. Salmonellosis is a broader term for infections caused by bacteria of the genus Salmonella.
Characteristics of Salmonella Typhi:
Classification:
Belongs to the Enterobacteriaceae family, a common group of bacteria found in the intestines of mammals.
Motile due to the presence of flagella (hair-like structures).
Morphology and Physiology:
Gram-negative bacteria (stain pink in Gram stain).
Facultatively anaerobic (can grow with or without oxygen).
Optimal growth temperature is 37°C.
Utilizes glucose and mannose for energy.
Antigenic Structure:
Possesses cell wall (O) antigens and flagellar (H) antigens, crucial for host cell invasion and serological identification.
Serological Detection:
Infection can be diagnosed through agglutination tests using patient serum to detect O and H antigens with specific antisera.
Host Specificity:
Unlike other Salmonella species that can colonize various animals, Salmonella Typhi is uniquely pathogenic to humans.
Predisposing Factors and Risk Factors:
Hygiene and Sanitation:
Inadequate Hand Hygiene: Poor handwashing after using the toilet increases the risk of transmission.
Poor Environmental Hygiene: Lack of clean water, inadequate sanitation, and improper excreta disposal (lack of latrines) facilitate bacterial spread.
Vectors: Flies can act as mechanical vectors, carrying bacteria to food and surfaces.
Socioeconomic Factors: Poor nutrition and living in poverty increase susceptibility to infection.
Compromised Gastric Acidity: Achlorhydria (lack of stomach acid) reduces the body’s ability to kill ingested bacteria.
Underlying Medical Conditions:
Schistosomiasis can compromise intestinal integrity, making it easier for bacteria to invade.
Individuals with homozygous sickle cell disease are more susceptible to infections.
Incidence and Susceptibility:
Age: While it can affect all ages, the peak incidence is typically between 10 and 25 years.
Sex: More commonly reported in women.
Infectious Dose:
A dose of 100,000 bacteria can cause illness in approximately 25% of individuals.
A high dose of 1,000,000,000 bacteria can lead to illness in about 95% of cases.
Higher doses generally correlate with shorter incubation periods.
Gastric Acidity: Lower gastric pH (higher acidity) provides protection by killing ingested bacteria.
Incubation Period:
The typical incubation period for typhoid fever is 2 to 3 weeks.
Transmission:
Fecal-Oral Route: The primary mode of transmission is the ingestion of food or water contaminated with the feces of infected individuals or carriers.
Water Contamination: Individuals with acute illness shed high concentrations of bacteria in their stool, contaminating water supplies.
Carriers:
Approximately 3-5% of infected individuals become chronic carriers, harboring the bacteria in their gallbladder, bile ducts, or liver and shedding it intermittently in their feces.
Some individuals experience mild, unrecognized illness and become long-term carriers.
Chronic carriers may be asymptomatic and serve as a source of new outbreaks for years.
Transmission Routes (Specific):
Fomites: Contact with contaminated objects (fomites) that have been in contact with feces or urine.
Flies: Flies can transmit the bacteria by contaminating food and surfaces.
Ingestion: Direct ingestion of contaminated food or water is the most common route.
Ano-oral Transmission: Direct fecal-oral contact, particularly in environments with high carrier rates (e.g., prisons).

Clinical Manifestations:
The clinical presentation of typhoid fever is variable, but a classic untreated course can be divided into four stages, each lasting approximately one week. However, with prompt antibiotic treatment, this progression is often altered.
Week 1 (Initial Stage): Characterized by a gradually increasing fever (step-ladder pattern), reaching 39-40°C (102-104°F) by the end of the week. Patients often experience malaise, fatigue, headache (frequently frontal and severe), generalized myalgia, and anorexia. Abdominal discomfort may be present. Some individuals may have a dry cough. Epistaxis (nosebleeds) can occur in about 25% of cases. Relative bradycardia (a slower pulse rate than expected for the degree of fever) is a classic sign. Laboratory findings often reveal leukopenia, eosinopenia, and relative lymphocytosis. Blood cultures are usually positive during this stage, while the Widal test is typically negative.
Week 2 (Progressive Stage): The patient becomes more severely ill with a sustained high fever. Delirium, characterized by confusion, disorientation, or agitation, may develop. Rose spots, which are transient, blanching, pink macules (1-3 mm in diameter), may appear on the trunk (abdomen and lower chest) in approximately one-third of patients. The abdomen may become distended and tender, particularly in the right lower quadrant. Diarrhea, with characteristic pea-soup colored stools, may occur, although constipation can also be frequent. Hepatosplenomegaly (enlargement of the liver and spleen) may be detectable and tender. The tongue may be coated with a brownish fur. Signs of dehydration may become apparent. The Widal test typically shows increasing titers of anti-O and anti-H antibodies. Blood cultures may remain positive.
Week 3 (Complication Stage): The patient is often critically ill and toxic. The fever remains high and may be intermittent. The pulse may become feeble. Patients may lapse into a “typhoid state,” characterized by obtundation, muttering delirium, and picking at bedclothes (carphology). Intestinal complications are most likely during this week as the inflamed Peyer’s patches can ulcerate deeply. This can lead to intestinal hemorrhage (manifesting as melena or hematochezia) or intestinal perforation, resulting in peritonitis (severe abdominal pain, rigidity, and tenderness). Other complications, such as myocarditis, encephalitis, or cholecystitis, may also arise.
Week 4 (Defervescence and Convalescence): In uncomplicated cases, the fever begins to subside, and other symptoms gradually improve as the patient’s temperature returns to normal (lysis). Recovery is often slow, and relapses of symptoms can occur. If left untreated, severe complications can lead to death.
Diagnosis:
The diagnosis of typhoid fever involves a combination of clinical suspicion and laboratory confirmation.
Blood Culture: Considered the gold standard for diagnosing typhoid fever, particularly in the first week of illness when bacteremia is present. Multiple blood cultures may increase sensitivity.
Stool Culture: Becomes more useful in the later stages of the illness and for identifying chronic carriers.
Urine Culture: Can also be positive, especially after the first week.
Bone Marrow Culture: The most sensitive method for detecting S. Typhi, but it is invasive and not routinely performed.
Widal Test: A serological test that detects antibodies against the O and H antigens of S. Typhi. A significant rise in antibody titers between acute and convalescent serum samples is suggestive of recent infection. However, the Widal test has limitations due to low sensitivity and specificity, potential for false-positive results (due to past exposure or cross-reacting antibodies), and false-negative results (especially early in the illness). It is less reliable in areas where typhoid fever is endemic due to high background levels of antibodies.
Typhidot (Tubex Test): A rapid serological test that detects IgM and IgG antibodies against a specific S. Typhi antigen. It offers faster results compared to the Widal test but also has limitations in sensitivity and specificity.
Polymerase Chain Reaction (PCR): Can detect S. Typhi DNA in blood or stool samples, offering rapid and specific diagnosis. PCR is particularly useful in the early stages of the illness before antibody responses are detectable.
Complete Blood Count (CBC): May show leukopenia (low white blood cell count), anemia, and thrombocytopenia (low platelet count).
Liver Function Tests (LFTs): May reveal mild elevations in liver enzymes (transaminases).
Differential Diagnosis:
Typhoid fever shares symptoms with several other infectious diseases, necessitating careful differentiation:
Malaria: Characterized by cyclical fever, chills, and sweating. Requires blood smear examination for diagnosis.
Dengue Fever: Marked by high fever, severe headache, retro-orbital pain, muscle and joint pain (“breakbone fever”), and rash.
Infectious Mononucleosis: Presents with fever, pharyngitis, lymphadenopathy, and fatigue.
Tuberculosis (Disseminated): Can cause prolonged fever, weight loss, and organ involvement.
Bacterial Endocarditis: Characterized by fever, heart murmur, and systemic embolization.
Brucellosis: Presents with fever, sweats, joint pain, and fatigue.
Leptospirosis: Caused by Leptospira bacteria, often associated with exposure to contaminated water.
Amoebic Liver Abscess: Can cause fever, right upper quadrant pain, and hepatomegaly.
Complications:
If left untreated or inadequately treated, typhoid fever can lead to serious and life-threatening complications:
Gastrointestinal Hemorrhage: Bleeding from eroded blood vessels in intestinal ulcers, ranging from mild to severe.
Intestinal Perforation: A serious complication where the ulcerated intestinal wall ruptures, leading to peritonitis, a surgical emergency.
Peritonitis: Inflammation of the peritoneum due to intestinal perforation, causing severe abdominal pain, rigidity, and sepsis.
Myocarditis: Inflammation of the heart muscle, potentially leading to heart failure.
Encephalitis: Inflammation of the brain, resulting in neurological symptoms such as confusion, seizures, and coma.
Meningitis: Inflammation of the meninges (membranes surrounding the brain and spinal cord).
Cholecystitis: Inflammation of the gallbladder, which can occur due to S. Typhi colonization.
Pneumonia: Lung infection that can develop as a secondary complication.
Osteomyelitis: Bone infection, a rare complication.
Septic Arthritis: Joint infection, also a rare complication.
Renal Complications: Including glomerulonephritis or acute kidney injury.
Psychiatric Disturbances: Delirium, psychosis, and other mental health issues can occur during the acute phase.
Relapse: Recurrence of symptoms after initial improvement, occurring in about 10-20% of untreated cases.
Treatment:
The primary goal of treatment is to eradicate the S. Typhi infection and prevent complications.
Antibiotic Therapy: Antibiotics are the mainstay of treatment. The choice of antibiotic depends on local resistance patterns.
Fluoroquinolones (e.g., Ciprofloxacin, Ofloxacin): Highly effective and often used as first-line agents in areas with low resistance. Oral or intravenous administration is possible.
Third-Generation Cephalosporins (e.g., Ceftriaxone, Cefotaxime): Also effective and commonly used, particularly for severe cases or in areas with fluoroquinolone resistance. Administered intravenously or intramuscularly.
Azithromycin: A macrolide antibiotic that is also effective against S. Typhi and can be administered orally.
Older Antibiotics (e.g., Chloramphenicol, Trimethoprim-Sulfamethoxazole [Cotrimoxazole], Ampicillin, Amoxicillin): While historically used, resistance to these antibiotics is now widespread in many parts of the world, limiting their current utility.
Dosage and Duration: The specific antibiotic, dosage, and duration of treatment are determined by the severity of the illness and local antimicrobial susceptibility data. Treatment typically lasts for 7-14 days, although shorter courses may be used with some antibiotics.
Supportive Care:
Fluid and Electrolyte Management: Maintaining adequate hydration is crucial, especially if the patient has fever and diarrhea. Oral rehydration solutions or intravenous fluids may be necessary.
Nutritional Support: A balanced and easily digestible diet is recommended.
Antipyretics: Paracetamol (acetaminophen) can be used to manage fever and discomfort.
Hygiene Measures: Strict attention to hygiene is important to prevent the spread of infection.
Corticosteroids: In severe cases of typhoid fever with complications like encephalopathy or myocarditis, corticosteroids (e.g., dexamethasone) may be used as adjunctive therapy to reduce inflammation.
Management of Complications: Specific interventions are required for complications such as intestinal hemorrhage (blood transfusion, endoscopy), intestinal perforation (surgical repair), and neurological involvement (supportive care, anticonvulsants if needed).
Management of Chronic Carriers:
Antibiotics: Prolonged courses of antibiotics, such as ciprofloxacin or amoxicillin, are used to attempt to eradicate S. Typhi from the gallbladder.
Cholecystectomy: Surgical removal of the gallbladder may be considered for chronic carriers, particularly if antibiotic therapy fails or if the individual has gallstones.
Prognosis:
The prognosis of typhoid fever is generally good with early diagnosis and appropriate antibiotic treatment. The case fatality rate in treated patients is typically less than 1%. However, without treatment, the mortality rate can be as high as 10-20%. The development of complications significantly worsens the prognosis. Relapses can occur in a small percentage of treated patients.
Prevention:
Prevention strategies for typhoid fever focus on improving sanitation, hygiene, and vaccination.
Public Health Measures:
Improved Sanitation: Ensuring access to safe drinking water and proper sewage disposal is the most effective way to prevent typhoid fever.
Food Safety: Implementing and enforcing regulations for food handling, preparation, and storage.
Health Education: Educating the public about the importance of handwashing, safe food and water practices.
Surveillance and Outbreak Response: Monitoring for cases of typhoid fever and implementing rapid public health interventions to control outbreaks.
Individual Measures:
Handwashing: Frequent and thorough handwashing with soap and water, especially after using the toilet and before preparing or eating food.
Safe Water: Drinking safe water, which may involve boiling, chlorination, or using water filters.
Safe Food: Consuming thoroughly cooked food and avoiding raw or undercooked foods, especially in endemic areas. Avoiding ice from unknown sources.
Travel Precautions: Travelers to endemic areas should be particularly vigilant about food and water safety.
Vaccination: Two types of typhoid vaccines are available:
Ty21a (Oral, Live Attenuated Vaccine): Administered in a series of capsules taken over several days. Provides protection for approximately 5 years.
Vi Polysaccharide Vaccine (Injectable, Inactivated Subunit Vaccine): Administered as a single injection. Provides protection for approximately 2 years.
Recommendations: Vaccination is recommended for travelers to endemic areas, individuals in close contact with known carriers, and in response to outbreaks.
Test MCQ Questions
Question 1:
What is the primary mode of transmission for typhoid fever?
A) Mosquito bites
B) Contaminated food and water
C) Airborne droplets
D) Direct physical contact
Question 2:
Which bacterium is responsible for causing typhoid fever?
A) Escherichia coli
B) Salmonella typhi
C) Streptococcus pneumoniae
D) Staphylococcus aureus
Question 3:
Which of the following complications can occur in severe cases of typhoid fever?
A) Fractures
B) Renal failure
C) Dental caries
D) Cholecystitis
Question 4:
Which diagnostic test is used to identify the presence of Salmonella typhi in the blood?
A) Blood smear examination
B) Stool culture
C) Urinalysis
D) Blood culture
Question 5:
What is the recommended antibiotic therapy for treating typhoid fever?
A) Penicillin
B) Amoxicillin
C) Ciprofloxacin
D) Erythromycin
Question 6:
Why is hospital admission often recommended in severe cases of typhoid fever?
A) To provide psychological support to the patient
B) To administer vaccines for long-term immunity
C) To ensure isolation and prevent disease transmission
D) To allow close monitoring and provide appropriate medical care
Question 7:
What is the primary preventive measure to avoid typhoid fever transmission in the community?
A) Proper handwashing with soap and water
B) Mosquito net usage
C) Wearing masks in public places
D) Vaccination against other bacterial infections
Question 8:
Which gastrointestinal complication can occur due to typhoid fever?
A) Pneumonia
B) Peritonitis
C) Otitis media
D) Conjunctivitis
Question 9:
Which of the following is NOT a recommended step to prevent typhoid fever?
A) Drinking untreated water from natural sources
B) Cooking food thoroughly
C) Washing hands properly before eating
D) Proper waste disposal
Question 10:
Who should be excluded from handling food and providing care to children during a typhoid fever outbreak?
A) Asymptomatic carriers and infected individuals
B) Healthcare professionals only
C) Pregnant women
D) Children under 5 years of age
Answers:
1. B – Contaminated food and water
2. B – Salmonella typhi
3. D – Cholecystitis
4. D – Blood culture
5. C – Ciprofloxacin
6. D – To allow close monitoring and provide appropriate medical care
7. A – Proper handwashing with soap and water
8. B – Peritonitis
9. A – Drinking untreated water from natural sources
10. A – Asymptomatic carriers and infected individuals
Explanation:
1. Typhoid fever is primarily spread through contaminated food and water, making option B the correct answer.
2. Salmonella typhi is the bacterium responsible for causing typhoid fever, making option B the correct answer.
3. Cholecystitis is one of the gastrointestinal complications associated with typhoid fever, making option D the
correct answer.
4. Blood culture is used to identify the presence of Salmonella typhi in the blood, making option D the correct
answer.
5. Ciprofloxacin is one of the recommended antibiotics for treating typhoid fever, making option C the correct
answer.
6. Hospital admission is recommended in severe cases of typhoid fever for close monitoring and appropriate
medical care, making option D the correct answer.
7. Proper handwashing with soap and water is the primary preventive measure to avoid typhoid fever
transmission, making option A the correct answer.
8. Peritonitis is a gastrointestinal complication that can occur due to typhoid fever, making option B the correct
answer.
9. Drinking untreated water from natural sources is NOT a recommended step to prevent typhoid fever, making
option A the correct answer.
10. Asymptomatic carriers and infected individuals should be excluded from handling food and providing care to
children during a typhoid fever outbreak, making option A the correct answer
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

