Antimicrobial Agents
Subtopic:
Antibiotics
Antibacterials (Antibiotics)
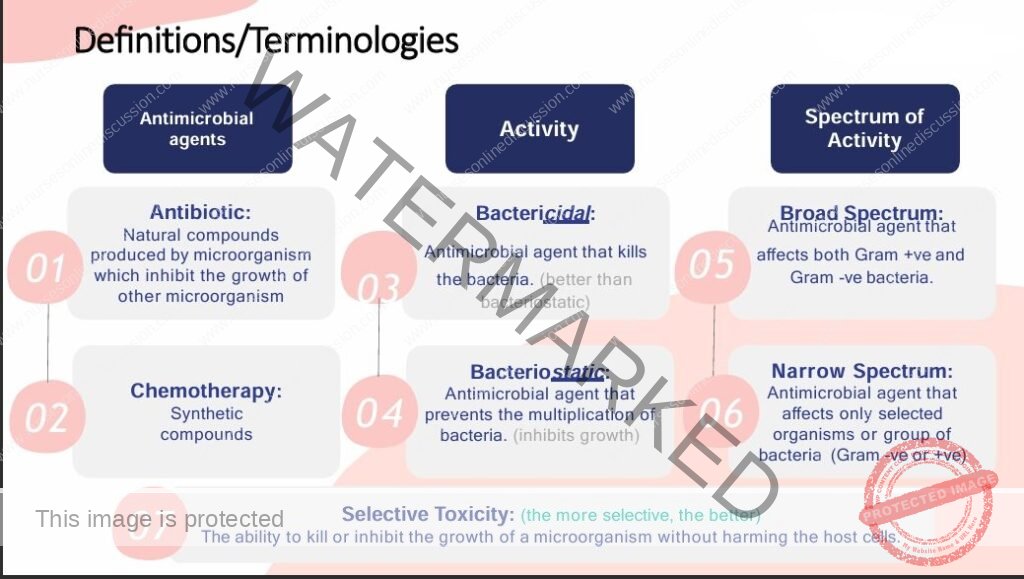
1. Definitions
Antibiotics:
Substances derived from living microorganisms that kill or inhibit the growth of other microorganisms.Antibacterials:
Drugs specifically used to treat bacterial infections.
➤ In practice, the terms antibacterials and antibiotics are often used interchangeably.
➤ Antibiotics are among the most commonly used—and misused—drugs.
2. Properties of Ideal Antibacterial Agents
High selective toxicity to pathogenic microorganisms.
Minimal or no adverse effects on the host.
Low tendency for the development of bacterial resistance.
Rapid and widespread tissue distribution.
Minimal interactions with other drugs.
Cost-effective and accessible.
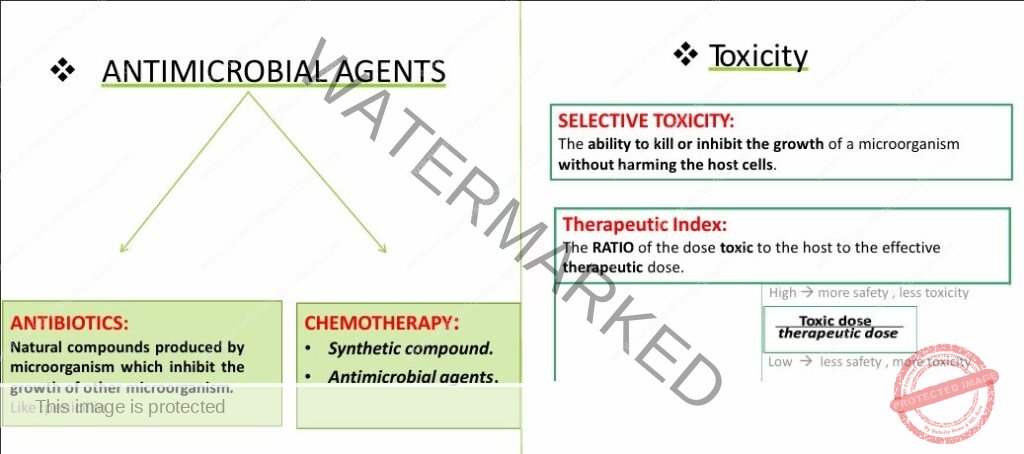
3. Selective Toxicity
Definition: The ability of an antibiotic to kill or inhibit harmful bacteria without damaging host cells.
Antibiotics work by targeting features unique to bacteria (e.g., cell wall, ribosomal subunits), ensuring selective toxicity.
4. Antibacterial Spectrum
Antibacterial spectrum refers to the range of bacterial species against which an antibiotic is effective.
Antibiotics may have either a broad or narrow spectrum of activity.
5. Broad Spectrum Antibiotics
Definition: Active against a wide variety of bacterial species (both Gram-positive and Gram-negative).
Uses:
Empirical therapy when the causative organism is unknown.
Mixed infections.
Risks:
Higher risk of superinfections due to disruption of normal flora (e.g., vaginal candidiasis with tetracyclines).
Examples:
Amoxicillin
Ampicillin
Doxycycline
Tetracycline
Ceftriaxone
Erythromycin
Ciprofloxacin
Cephalexin
6. Narrow Spectrum Antibiotics
Definition: Effective against a limited range of bacterial species.
Uses:
Recommended for definitive therapy when the specific pathogen is identified.
Selection guided by culture and sensitivity tests.

Mode of Action of Antibiotics
1. Classification by Action
Antibiotics are classified as:
Bacteriostatic: Inhibit the growth and reproduction of bacteria, allowing the host’s immune system to eliminate the infection.
Bactericidal: Directly kill bacteria, leading to bacterial cell death.
2. Choosing Between Bacteriostatic and Bactericidal
The selection depends on:
Severity of the infection
Immune status of the patient
Bactericidal antibiotics are preferred when:
The infection is severe or life-threatening.
The patient is immunocompromised or has a weakened immune response.
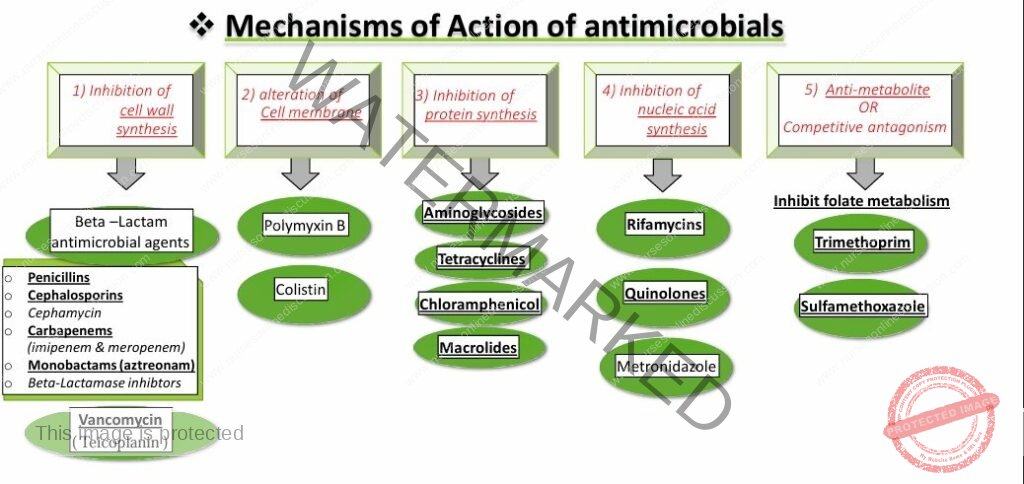
Mechanisms of action of antimicrobial agents

Mechanisms of Action of antimicrobials
Antibiotics and Antibacterial Therapy
1. Mode of Action
Bacteriostatic antibiotics:
Inhibit bacterial growth.
Require a functioning immune system to clear the infection.
Some may act bactericidal at higher doses or against specific bacteria.Examples:
Tetracyclines (e.g. doxycycline, minocycline)
Macrolides (e.g. erythromycin, azithromycin)
Sulphonamides (e.g. sulphadimidine)
Chloramphenicol
Bactericidal antibiotics:
Kill bacteria directly.
Preferred in severe infections and immunocompromised patients.
Do not depend on immune system action.Examples:
Penicillins (e.g. amoxicillin, benzylpenicillin)
Cephalosporins (e.g. cephalexin, ceftriaxone)
Aminoglycosides (e.g. gentamycin, amikacin)
Quinolones (e.g. ciprofloxacin, levofloxacin)
2. Antibiotic Resistance
Definition: Reduced effectiveness of antibiotics against certain bacteria.
Types:
Natural resistance: Exists without prior antibiotic exposure.
▸ Examples:Streptococcus pneumoniae is naturally resistant to ciprofloxacin
Pseudomonas aeruginosa is resistant to penicillin G
Acquired resistance: Develops after exposure to antibiotics that were previously effective.
▸ Examples:N. gonorrhoeae became resistant to ciprofloxacin
Staphylococcus aureus became resistant to penicillin G
Mechanisms of resistance:
Enzyme production that destroys antibiotic structure
Altered cell wall or membrane permeability
Modified target sites for antibiotics
Development of alternative metabolic pathways
Prevention:
Avoid unnecessary antibiotic use
Use full, appropriate dosages
Avoid prolonged topical antibiotic use
Prefer narrow-spectrum antibiotics
Use combination therapy or alternate regimens when necessary
3. Indications for Antibiotic Use
Definitive Therapy:
Based on culture and sensitivity testing
Pathogen is known
Narrow-spectrum antibiotics preferred
Empirical Therapy:
Based on best clinical judgment (before lab results)
Broad-spectrum or combination therapy used
Common in resource-limited settings (e.g. Uganda)
Surgical Prophylaxis:
Given before surgery to prevent infection
Single effective dose preferred
Common antibiotics: cefazolin, ceftriaxone, clindamycin
4. Antibiotic Combinations
Definition: Use of two or more antibiotics simultaneously
Uses:
Prevent resistance (e.g., in TB)
Treat mixed infections (e.g., PID, sepsis)
Lower toxicity by reducing doses
Enhance effectiveness (e.g., gentamycin + benzylpenicillin for sepsis)
Disadvantages:
Increased risk of side effects
Higher chance of superinfections (e.g., candidiasis)
Increased cost
Risk of drug antagonism
5. Factors to Consider in Antibiotic Selection
Spectrum of activity: Ensure coverage of suspected pathogens
Tissue penetration: Ability to reach infection site
▸ Considerations:Blood supply (e.g., diabetic foot)
Abscesses (may require drainage)
Chronic infections (e.g., prostatitis)
Antibiotic resistance: Use local resistance patterns when possible
▸ Example: 96% resistance of N. gonorrhoeae to ciprofloxacinSafety profile: Prefer drugs with mild side effects
Patient factors:
Pregnancy, age, allergies
Some antibiotics are contraindicated during pregnancy, breastfeeding, or childhood
Organ function:
Check liver and kidney status
Adjust dose or avoid certain drugs in renal or hepatic impairment
Cost:
Select cost-effective options to improve access
Compliance:
Recommend antibiotics with fewer daily doses if adherence is a concern
Route of administration:
Injectables for severe infections
Oral switch after ~72 hours if clinical improvement occurs
Oral route preferred for mild/moderate infections
6. Causes of Antibiotic Failure
Resistance
Incorrect diagnosis
Wrong dose or duration
Poor tissue penetration (e.g., due to pus)
Substandard antibiotics
Non-compliance
Incomplete pathogen coverage
Drug interactions
7. Common Antibiotic Classes
Penicillins
Cephalosporins
Macrolides
Quinolones
Tetracyclines
Aminoglycosides
- Sulphonamides
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

