Foundations of Nursing 1
Subtopic:
Causes of Infection
Learning Objectives
Identify and classify different types of infectious agents (bacteria, viruses, fungi, parasites, prions).
Recognize mechanisms by which pathogens invade and damage the host.
Understand the reservoirs and sources of infection in clinical settings.
Explain various transmission modes (contact, airborne, droplet, vector-borne, vehicle).
Analyze risk factors that increase susceptibility to infections.
Describe pathogenesis of infection from entry to systemic spread.
Distinguish between infection types: primary, secondary, opportunistic, nosocomial, and community-acquired.
Explain factors driving antimicrobial resistance (AMR).
Articulate the nurse’s role in preventing and managing infection
Infections
Infections are among the most significant clinical concerns in nursing practice. They occur when pathogenic microorganisms such as bacteria, viruses, fungi, or parasites invade and multiply within the body, causing illness or disease. Understanding the causes of infections is critical for nurses, as it enables the application of appropriate infection prevention and control strategies, ensures safe patient care, and reduces the risk of healthcare-associated infections (HAIs).
The causes of infections are multifactorial, encompassing microbial agents, human susceptibility, environmental conditions, and transmission modes. This section elaborates on the various causes of infection and explores their implications in the healthcare setting.
Infection
Infection is the successful invasion and multiplication of micro-organism in the body to cause disease. There are many different species of micro-organisms that affect the human body as a host and cause a disease. Some of the factors involved in transmission of infection are as follows;
Reservoir of infection:
- Men
- Animals
Mode of escape of micro-organisms:
- Nose – exhalation, sneezing (expired air).
- Mouth – coughing.
- Urinary system – urine.
- Gastrointestinal tract – faeces.
- Wounds and ulcers – discharge, pus.
- Skin – sweat e.g. Ebola, Hep.B.
Vehicle for transmission:
- Contaminated hands.
- Air
- Water
- Food
- Linen
- Crockery and cutlery
Mode of entry:
- Nose – inhalation
- Mouth – ingestion
- Urethra – direct contact
- Trans – placental
- Genital tract – direct contact with fluids
- Mucous membranes and unhealthy skin – direct contact i.e. gonorrhea can be got through kissing.
Susceptible host:
- People with low immunity.
Causes of infection
Infection happens when tiny living things called micro-organisms successfully enter the body and multiply, causing disease. There are many different types of micro-organisms that can affect the human body and cause illness.
For an infection to happen, there needs to be a chain of events. Breaking any link in this chain can prevent infection. The chain involves:
- Reservoir: Where the micro-organisms live and multiply (e.g., people, animals, environment).
- Mode of escape: How micro-organisms leave the reservoir (e.g., nose/mouth when coughing or sneezing, urine, feces, wounds, skin).
- Vehicle for transmission: How micro-organisms travel from the reservoir to another person (e.g., contaminated hands, air, water, food, linen).
- Mode of entry: How micro-organisms enter a new person’s body (e.g., nose/mouth through breathing or eating, urethra, cuts in the skin).
- Susceptible host: A person who is at risk of getting the infection, usually because they have low immunity or are already weak.
Ways in which infection can be prevented (breaking the chain of infection)
Breaking the chain of infection is crucial in nursing. Key methods include: Isolation or barrier nursing: Is the separation of the patient and his unit from others to prevent the direct or indirect contact of infectious agents to a susceptible person e.g. droplet infection, clothing etc. Hand washing: Is the single most important means of preventing the transmission of infection. Careful washing of hands using soap, water and nail brush reduces the number of bacteria.
Use of protective gears: Gears such as gloves, gowns, masks, gargles, gumboots; help protect the nurse from pathogen. They serve as a barrier when handling articles which are contaminated.
Principles of Infection Control
There are five basic universal principles of infection control;
- Hand washing Routing hand washing
- Antiseptic hand washing
- Alcohol hand rub
- Surgical hand scrub
- Adequate protective gears Gloves; – sterile surgical single use gloves, examination disposable gloves, heavy-duty utility gloves
- Plastic aprons; – Wear these for all procedures where there is a potential of contamination from splashing of blood and body fluids, handling of soiled dressings and used linen from all patients.
- Gowns; – Worn in operating theatres and other areas where a patient may bleed heavily.
- Eye/face protection; – Protective eye wear and face masks be made fully available and worn where applicable.
- Boots; – Worn in places where spillage of blood, body fluids, secretion and excretions are anticipated. NB. Clean bots with soap and water immediately after use. In case of contamination with blood or body fluids; disinfect.
- Surgical masks; – Wear a mask to protect the mucous membranes of the nose and mouth from splashes of body fluids.
Proper sterilization Sterilization policy is a code of practice, which if correctly followed will ensure a clean and safe health unit, where multiplication and spread of harmful microbes is kept under control. Proper sharp disposal Sharps should be handled with extreme caution to avoid injuries during use, disposal or reprocessing. Where possible, all sharps should be disposable. Safe waste management It is essential that every health care worker without exception, who handles and disposes the waste, understands the nature of waste and risks, the color code of waste bins, uses personal protective equipment, is conversant with emergency procedures, and is aware they are liable to discipline for non-compliance.
Principles of infection prevention and control
Infection prevention and control are very important in nursing to protect patients, healthcare workers, and the community. The main goal is to break the chain of infection. There are five basic universal principles of infection control:
- Hand washing: This is the single most important way to prevent the spread of infection. Proper hand washing with soap and water or using alcohol hand rub reduces the number of bacteria.
- Use of personal protective equipment (PPE): Wearing gloves, gowns, masks, and other protective gear creates a barrier to protect nurses from pathogens and prevents the spread of micro-organisms.
- Cleaning, disinfection, and sterilization: Cleaning removes visible dirt and most micro-organisms. Disinfection destroys most pathogenic micro-organisms. Sterilization destroys all micro-organisms, including tough spores and viruses. These processes are essential for making instruments and surfaces safe to handle.
- Safe waste management and disposal: Handling and disposing of medical waste correctly prevents the spread of infection. Waste should be segregated (sorted) at the point of generation.
- Isolation of infectious patients: Separating patients with infectious diseases from others helps prevent direct
I. Classification of Infectious Agents (Pathogens)
1. Bacteria

Bacteria are single-celled microorganisms that can exist independently, symbiotically, or parasitically. While many bacteria are harmless or beneficial, some are pathogenic and capable of causing diseases.
Examples of bacterial infections:
Streptococcus pneumoniae: causes pneumonia
Mycobacterium tuberculosis: causes tuberculosis
Escherichia coli: causes urinary tract infections (UTIs)
Staphylococcus aureus: can cause skin infections, sepsis, or pneumonia
Mechanism of Infection: Bacteria enter the body through breaks in the skin, mucous membranes, inhalation, ingestion, or catheterization, multiplying and producing toxins that damage host tissues.
2. Viruses

Viruses are the smallest infectious agents, composed of genetic material (DNA or RNA) encased in a protein coat. They require a host cell to replicate.
Examples of viral infections:
Influenza virus: causes flu
HIV (Human Immunodeficiency Virus): causes AIDS
Hepatitis B and C viruses: cause liver infections
SARS-CoV-2: causes COVID-19
Mechanism of Infection: Viruses attach to and penetrate host cells, hijacking cellular machinery to reproduce. The release of new viral particles damages host tissues and triggers immune responses.
3. Fungi
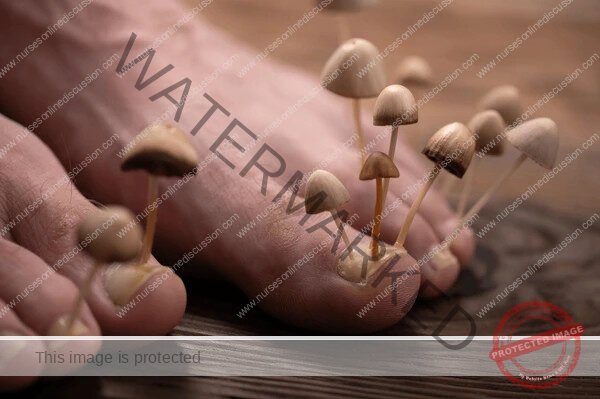
Fungi include yeasts and molds. Some are opportunistic pathogens, particularly affecting immunocompromised individuals.
Examples of fungal infections:
Candida albicans: causes oral thrush and vaginal yeast infections
Aspergillus: causes respiratory infections
Dermatophytes: cause skin infections like athlete’s foot and ringworm
Mechanism of Infection: Fungi can colonize skin, mucosa, or lungs and may produce spores that disseminate via air or contact.
4. Parasites

Parasites are organisms that live on or within a host, deriving nutrients at the host’s expense. They can be protozoa, helminths (worms), or ectoparasites (lice, mites).
Examples of parasitic infections:
Plasmodium falciparum: causes malaria
Giardia lamblia: causes giardiasis
Ascaris lumbricoides: causes intestinal obstruction
Pediculus humanus capitis: head lice infestation
Mechanism of Infection: Parasites may enter the body through ingestion of contaminated food or water, vector bites, or skin penetration.
5. Prions

Prions are misfolded proteins capable of inducing abnormal folding of normal proteins in the brain, leading to neurodegenerative diseases.
Examples of prion diseases:
Creutzfeldt-Jakob disease (CJD)
Bovine spongiform encephalopathy (mad cow disease)
Mechanism of Infection: Unlike other pathogens, prions do not replicate but induce the conversion of normal proteins into abnormal forms.
II. Sources of Infection
The source or reservoir of infection is the habitat where the pathogen normally lives and multiplies. Understanding sources is vital in breaking the chain of infection.
1. Human Reservoirs
Humans can harbor pathogens with or without symptoms.
Symptomatic carriers: Individuals actively showing signs of disease
Asymptomatic carriers: Individuals who harbor pathogens but show no symptoms (e.g., Typhoid Mary)
2. Animal Reservoirs
Some infections are zoonotic, originating from animals.
Examples:
Rabies from dogs and bats
Plague from rodents
Avian flu from birds
3. Environmental Reservoirs
Non-living environments can harbor infectious agents.
Examples:
Soil: Clostridium tetani (tetanus)
Water: Vibrio cholerae (cholera)
Surfaces and equipment in hospitals: harbor resistant organisms like MRSA
III. Modes of Transmission
Pathogens are transmitted through various mechanisms. Understanding these pathways is essential for nurses to implement effective infection control measures.
1. Contact Transmission
Direct contact: Physical contact with an infected individual (e.g., touching wounds, body fluids)
Indirect contact: Contact with contaminated objects (fomites) such as doorknobs, stethoscopes, or medical devices
2. Droplet Transmission
Occurs when respiratory droplets containing pathogens are expelled during coughing, sneezing, or talking and land on the mucosa of another person.
Diseases: Influenza, COVID-19, pertussis
3. Airborne Transmission
Involves small particles or aerosols that remain suspended in air and are inhaled.
Diseases: Tuberculosis, measles, varicella (chickenpox)
4. Vector-Borne Transmission
Vectors such as mosquitoes, ticks, or fleas transmit infections through bites or contact.
Diseases: Malaria (mosquito), Lyme disease (tick), plague (flea)
5. Common Vehicle Transmission
Occurs when a single contaminated source spreads infection to multiple hosts.
Examples: Contaminated food, water, medications, or intravenous fluids
IV. Risk Factors That Promote Infection
1. Host Susceptibility
A person’s immune system plays a critical role in defense against infection. Certain conditions increase susceptibility:
Age: Infants and the elderly have weaker immune defenses
Chronic diseases: Diabetes, cancer, HIV/AIDS
Nutritional status: Malnutrition weakens immunity
Medications: Immunosuppressants, chemotherapy, long-term antibiotics
Stress and fatigue: Reduce immune responses
Breaks in skin integrity: Wounds, surgery, burns
2. Hospital/Healthcare Environment
Healthcare settings are high-risk areas due to the presence of vulnerable patients and invasive procedures.
Catheters and IV lines: Breach natural barriers
Surgical procedures: Increase infection risk
Healthcare workers: Can act as vectors
Contaminated equipment: May harbor resistant bacteria
Poor hand hygiene: Major contributor to HAIs
3. Invasive Medical Devices
Urinary catheters: Associated with UTIs
Central lines: Associated with bloodstream infections
Endotracheal tubes: Linked to ventilator-associated pneumonia
V. Pathogenesis of Infection
Pathogenesis refers to the process by which an infection leads to disease. Several stages characterize this process:
1. Entry of Pathogen
Pathogens enter through specific portals:
Respiratory tract (e.g., flu)
Gastrointestinal tract (e.g., cholera)
Urogenital tract (e.g., gonorrhea)
Skin or mucosal breaches (e.g., tetanus)
2. Adhesion to Host Cells
Pathogens must adhere to host tissues using pili, fimbriae, or adhesive proteins.
3. Invasion and Multiplication
After attachment, pathogens invade tissues and multiply, often avoiding immune responses.
4. Host Damage
Damage occurs via:
Toxin production (e.g., botulinum toxin)
Immune-mediated injury
Direct tissue invasion
5. Spread of Infection
Infections may remain localized or spread systemically via blood or lymphatic system (sepsis, bacteremia).
VI. Types of Infections Based on Cause or Source
1. Primary vs. Secondary Infection
Primary infection: The initial infection caused by a pathogen
Secondary infection: Occurs due to lowered immunity from the primary infection or treatment
2. Opportunistic Infections
Caused by organisms that do not typically cause disease in healthy individuals but infect immunocompromised hosts.
Examples: Pneumocystis jirovecii pneumonia in HIV patients
3. Nosocomial or Hospital-Acquired Infections (HAIs)
Infections acquired during hospital stay after 48 hours of admission.
Common sites: Urinary tract, surgical sites, bloodstream, respiratory tract
Common pathogens: MRSA, VRE, Clostridium difficile
4. Community-Acquired Infections
Infections acquired outside healthcare settings.
VII. Emerging and Re-Emerging Infections
Increased globalization, climate change, and microbial adaptation have led to the emergence of new pathogens and the re-emergence of old ones.
Emerging infections: SARS, COVID-19, Ebola
Re-emerging infections: Tuberculosis, measles
Factors contributing to emergence:
Antibiotic resistance
Urbanization
International travel
Poor sanitation
VIII. Antimicrobial Resistance (AMR)
A critical modern cause of persistent infections is antimicrobial resistance.
Definition: The ability of microorganisms to resist the effects of drugs
Common resistant pathogens:
Methicillin-resistant Staphylococcus aureus (MRSA)
Vancomycin-resistant Enterococci (VRE)
Multidrug-resistant TB (MDR-TB)
Causes:
Overuse and misuse of antibiotics
Inadequate infection control
Poor patient compliance
Agricultural use of antibiotics
Impact:
Prolonged hospital stays
Increased mortality
Higher treatment costs
IX. Role of Nurses in Preventing Infections
Nurses play a pivotal role in preventing and controlling infections:
Hand hygiene: Most effective infection prevention measure
Aseptic techniques: During invasive procedures
Use of PPE: Gloves, masks, gowns to prevent cross-contamination
Patient education: Promoting hygiene, vaccination, and medication adherence
Sterilization and disinfection: Of equipment and environment
Surveillance and reporting: Early identification and containment of outbreaks
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
- History of Nursing
- The Role of the Nurse
- Code of Conduct for Nurses
- Principles of Professional Nursing Ethics and Etiquette
- Patient’s Rights
- Nursing and the Law
- Nursing Standards and Qualities of a Nurse
- General Principles and Rules of All Nursing Procedures
- Hospital Economy
- Use of Personal Protective Equipment
- Routine and Weekly Cleaning of the Ward
- Waste Management and Disposal
- Isolation of Infectious Patients
- Causes of Infection
- Medical Waste Disposal and Management
- Cleaning Methods
- Carry out Adequate Feeding of Patients
- Perform Bladder and Bowel Care
- Passing a Flatus Tube
- Administration of Enema
- Ward Report
- Lifting/Positioning a Patient
- Tepid Sponging
- General Principles in Patient Care
- Ethics in Nursing Care
- Principles of Infection Prevention and Control
- Body Mechanics
- Bed Making
- Vital Observations
- Bed Bath
- Oral Care/Mouth Care
- Care and Treatment of Pressure Ulcers
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

