Foundations of Nursing I
Subtopic:
Care and Treatment of Pressure Ulcers
Critical Role in Patient Safety
Pressure ulcers, also known as pressure injuries or bedsores, are localized areas of tissue damage caused by prolonged pressure, shear, or friction, often affecting immobile or debilitated patients. These preventable complications increase morbidity, prolong hospital stays, and compromise patient dignity. Effective care and treatment of pressure ulcers are central to nursing practice, requiring a blend of prevention, assessment, and evidence-based interventions. These notes outline the stages, prevention strategies, treatment approaches, and nursing responsibilities for pressure ulcer management, equipping students with essential skills for quality care.
Stages of Pressure Ulcers
Pressure ulcers are classified into stages based on tissue involvement, per the National Pressure Injury Advisory Panel (NPIAP):
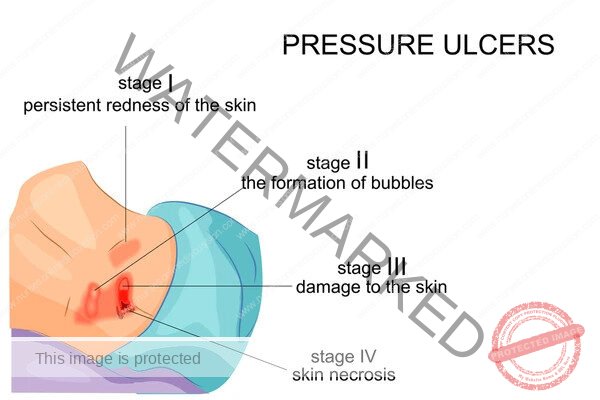
Stage 1: Non-blanchable erythema of intact skin; may be painful or warm.
Stage 2: Partial-thickness skin loss with exposed dermis; presents as a shallow ulcer or blister.
Stage 3: Full-thickness skin loss involving subcutaneous tissue; may include undermining or tunneling.
Stage 4: Full-thickness loss extending to muscle, bone, or tendons; often includes necrosis.
Unstageable: Obscured by slough or eschar, requiring debridement to determine depth.
Deep Tissue Injury: Persistent discoloration (purple/maroon) with intact or broken skin, indicating underlying tissue damage.
Prevention Strategies
Preventing pressure ulcers is a priority, guided by evidence-based practices:
Risk Assessment: Use tools like the Braden Scale to evaluate risk factors (mobility, nutrition, moisture, sensory perception).
Repositioning: Turn immobile patients every 2 hours, using 30-degree lateral tilts to offload pressure points (e.g., sacrum, heels).
Support Surfaces: Utilize pressure-relieving devices (e.g., foam mattresses, air overlays) for high-risk patients.
Skin Care: Keep skin clean and dry, apply moisturizers for dryness, and use barrier creams for incontinence.
Nutrition: Ensure adequate protein, calories, and hydration to support tissue repair; consult dietitians for deficiencies.
Patient Education: Teach patients and families about repositioning and skin inspection to promote self-care.
Treatment Approaches
Treatment varies by stage and requires a multidisciplinary approach:
Stage 1:
Relieve pressure using repositioning schedules and support surfaces.
Apply transparent films or hydrocolloid dressings to protect skin.
Monitor daily for progression.
Stage 2:
Cleanse with saline; avoid harsh antiseptics.
Use hydrocolloid or foam dressings to maintain a moist healing environment.
Reassess frequently for infection or worsening.
Stage 3/4:
Debride necrotic tissue (e.g., enzymatic or surgical debridement) in collaboration with wound care specialists.
Apply advanced dressings (e.g., alginate for exudate, silver dressings for infection).
Consider negative pressure wound therapy for large wounds.
Unstageable/Deep Tissue Injury:
Consult specialists for debridement and staging.
Protect surrounding tissue with appropriate dressings.
Infection Management:
Assess for signs (e.g., foul odor, increased exudate); obtain wound cultures if indicated.
Administer prescribed antibiotics and maintain aseptic technique during dressing changes.
Nursing Responsibilities
Nurses play a pivotal role in pressure ulcer care through:
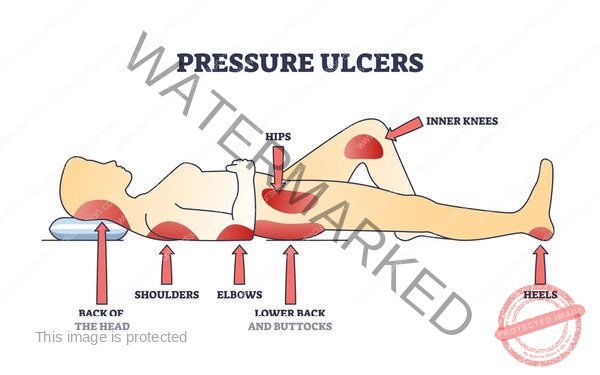
Assessment: Inspect skin daily, focusing on bony prominences (e.g., heels, sacrum); document stage, size, and wound characteristics.
Documentation: Record interventions, wound progress, and risk scores in the patient chart for continuity of care.
Implementation: Perform dressing changes using aseptic technique, reposition patients, and apply prescribed treatments.
Collaboration: Work with wound care nurses, dietitians, and physical therapists to optimize outcomes.
Patient Education: Teach patients and caregivers about prevention strategies, such as proper positioning and nutrition.
Advocacy: Ensure access to pressure-relieving devices and report barriers (e.g., inadequate staffing) to management.
Challenges in Pressure Ulcer Care
Obstacles include:
Patient Factors: Non-compliance with repositioning due to pain or cognitive impairment.
Resource Limitations: Lack of specialized mattresses or dressings in low-resource settings.
Time Constraints: High workloads may delay assessments or interventions.
Complexity: Managing advanced ulcers requires specialized knowledge and coordination.
Mitigation involves prioritizing high-risk patients, leveraging team support, and seeking continuing education on wound care.
Integration into Nursing Practice
Pressure ulcer care aligns with the nursing process:
Assessment: Evaluate skin and risk factors.
Diagnosis: Identify “Impaired Skin Integrity” or “Risk for Pressure Ulcer.”
Planning: Develop a care plan with repositioning and dressing schedules.
Implementation: Execute prevention and treatment strategies.
Evaluation: Monitor wound healing and adjust interventions as needed.
Related Topics
• General Principles and Rules of All Nursing Procedures
• Hospital Economy
• Use of Personal Protective Equipment
• Routine and Weekly Cleaning of the Ward
• Waste Management and Disposal
• Isolation of Infectious Patients
• Causes of Infection
• Medical Waste Disposal and Management
• Cleaning Methods
• Carry out Adequate Feeding of Patients
• Perform Bladder and Bowel Care
• Passing a Flatus Tube
• Administration of Enema
• Ward Report
• Lifting/Positioning a Patient
• Tepid Sponging
• General Principles in Patient Care
• Ethics in Nursing Care
• Principles of Infection Prevention and Control
• Body Mechanics
• Bed Making
• Vital Observations
• Bed Bath
• Oral Care/Mouth Care
• Care and Treatment of Pressure Ulcers
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

