circulatory system
Subtopic:
Arteriosclerosis
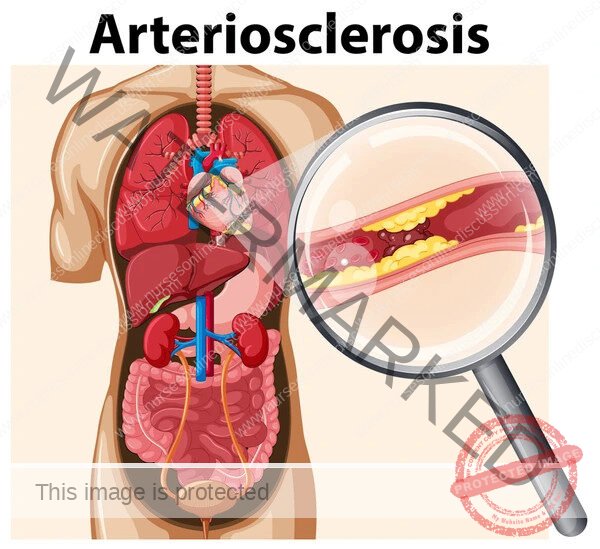
Arteriosclerosis is a general term that refers to the thickening, hardening, and loss of elasticity of the walls of arteries.
This process can lead to restricted blood flow, potentially causing serious cardiovascular diseases. It is a progressive condition that develops over time and is a major contributor to morbidity and mortality worldwide.
While often used interchangeably with atherosclerosis, arteriosclerosis is a broader term encompassing several distinct pathological processes affecting the arterial wall.
Types of Arteriosclerosis
Arteriosclerosis can be broadly classified into three main types:
Atherosclerosis: The most common and clinically significant type. It is characterized by the formation of plaques (atheromas) within the inner lining (intima) of large and medium-sized arteries. These plaques are composed of lipids, inflammatory cells, smooth muscle cells, and connective tissue.
Monckeberg’s Medial Calcific Sclerosis: Characterized by calcification within the media (middle layer) of muscular arteries. It typically affects the arteries of the extremities and is often seen in older individuals and those with diabetes. It does not usually narrow the arterial lumen significantly and is generally considered less clinically important than atherosclerosis, although it can affect arterial stiffness.
Arteriolosclerosis: Affects small arteries and arterioles. It is often associated with hypertension and diabetes. Two main forms exist:
Hyaline Arteriolosclerosis: Characterized by homogeneous, pink hyaline thickening of the arteriolar walls, leading to luminal narrowing. Commonly seen in benign hypertension and diabetes.
Hyperplastic Arteriolosclerosis: Characterized by concentric, laminated thickening of arteriolar walls (“onion-skin” appearance) due to proliferation of smooth muscle cells and thickened basement membranes. Typically seen in malignant hypertension.
Atherosclerosis: Pathogenesis
Atherosclerosis is a chronic inflammatory process initiated by injury to the endothelial lining of the artery. While the exact mechanisms are complex and not fully understood, key steps include:
Endothelial Dysfunction: Damage to the endothelium can be caused by various factors, including dyslipidemia (especially high LDL cholesterol), hypertension, smoking, diabetes, and inflammatory mediators. This dysfunction increases endothelial permeability and promotes the adhesion of leukocytes.
Lipid Accumulation: Lipoproteins, particularly oxidized LDL (oxLDL), accumulate in the subendothelial space (intima).
Inflammatory Response: Monocytes adhere to the dysfunctional endothelium, migrate into the intima, and differentiate into macrophages. These macrophages engulf the accumulated lipids, becoming foam cells, which are a hallmark of early atherosclerotic lesions (fatty streaks).
Smooth Muscle Cell Migration and Proliferation: Smooth muscle cells from the media migrate into the intima and proliferate. They contribute to the formation of the fibrous cap of the plaque and produce extracellular matrix components.
Plaque Formation and Progression: The accumulation of foam cells, smooth muscle cells, lipids, and extracellular matrix leads to the formation of a fibrous plaque. The plaque can grow over time, narrowing the arterial lumen (stenosis) and restricting blood flow.
Plaque Instability and Rupture: Advanced plaques can become unstable due to thinning of the fibrous cap, increased lipid core size, and ongoing inflammation. Rupture of an unstable plaque exposes the thrombogenic contents to the bloodstream, leading to rapid thrombus formation.
Thrombosis: Thrombus formation on a ruptured plaque can acutely occlude the artery, leading to sudden cessation of blood flow and clinical events such as myocardial infarction (heart attack) or stroke.
Atherosclerosis: Risk Factors
Risk factors for atherosclerosis can be broadly categorized as modifiable and non-modifiable:
Modifiable Risk Factors:
Dyslipidemia: High levels of LDL cholesterol, low levels of HDL cholesterol, and high triglycerides.
Hypertension: High blood pressure damages the endothelium and accelerates plaque formation.
Smoking: Damages the endothelium, promotes inflammation, and increases thrombosis risk.
Diabetes Mellitus: Contributes to endothelial dysfunction, dyslipidemia, and inflammation.
Obesity: Associated with hypertension, dyslipidemia, insulin resistance, and inflammation.
Physical Inactivity: Contributes to obesity, dyslipidemia, and hypertension.
Unhealthy Diet: High intake of saturated and trans fats, cholesterol, and sodium.
Metabolic Syndrome: A cluster of conditions including abdominal obesity, high blood pressure, high blood sugar, and abnormal lipid levels.
Non-Modifiable Risk Factors:
Age: The risk of atherosclerosis increases with age.
Sex: Men are generally at higher risk than premenopausal women. After menopause, the risk in women increases and approaches that of men.
Family History: A family history of premature cardiovascular disease increases the risk.
Genetics: Certain genetic predispositions can increase susceptibility.
Atherosclerosis: Clinical Manifestations
The clinical manifestations of atherosclerosis depend on the location and severity of arterial narrowing or occlusion. Symptoms typically appear when the arterial lumen is significantly narrowed (usually > 70%) or when plaque rupture and thrombosis occur.
Coronary Artery Disease (CAD): Atherosclerosis of the coronary arteries supplying the heart muscle. Can lead to:
Angina Pectoris: Chest pain or discomfort, typically triggered by exertion and relieved by rest or nitroglycerin, due to insufficient blood flow to the myocardium (ischemia).
Myocardial Infarction (Heart Attack): Death of myocardial tissue due to complete or near-complete occlusion of a coronary artery, usually by thrombus on a ruptured plaque.
Sudden Cardiac Death: Often caused by fatal arrhythmias resulting from severe ischemia or infarction.
Cerebrovascular Disease: Atherosclerosis of the arteries supplying the brain (carotid and vertebral arteries). Can lead to:
Transient Ischemic Attack (TIA): Temporary neurological symptoms (e.g., weakness, numbness, vision loss, difficulty speaking) due to transient reduction in blood flow to the brain. Often a warning sign of impending stroke.
Ischemic Stroke: Death of brain tissue due to complete or near-complete occlusion of a cerebral artery, usually by thrombus.
Peripheral Artery Disease (PAD): Atherosclerosis of the arteries supplying the limbs, most commonly the legs. Can lead to:
Intermittent Claudication: Pain, cramping, or fatigue in the leg muscles during exercise, relieved by rest, due to insufficient blood flow to the muscles.
Critical Limb Ischemia: Severe pain at rest, non-healing ulcers, or gangrene due to severe reduction in blood flow.
Renal Artery Stenosis: Atherosclerosis of the renal arteries supplying the kidneys. Can lead to:
Hypertension: Often difficult to control.
Chronic Kidney Disease: Due to reduced blood flow and damage to kidney tissue.
Mesenteric Ischemia: Atherosclerosis of the arteries supplying the intestines. Can lead to abdominal pain, especially after eating, and weight loss. Acute occlusion can cause severe abdominal pain and bowel infarction.
Atherosclerosis: Diagnosis
Diagnosis involves assessing risk factors, clinical symptoms, and using various diagnostic tests:
Clinical History and Physical Examination: Detailed assessment of symptoms, risk factors, and signs of vascular disease (e.g., reduced pulses, bruits).
Blood Tests: Lipid profile (total cholesterol, LDL, HDL, triglycerides), blood glucose (for diabetes), and inflammatory markers (e.g., high-sensitivity C-reactive protein – hs-CRP).
Electrocardiogram (ECG): Can show evidence of past or current myocardial ischemia or infarction.
Stress Testing: Evaluates for exercise-induced myocardial ischemia.
Echocardiography: Assesses cardiac structure and function, including wall motion abnormalities suggestive of ischemia.
Ankle-Brachial Index (ABI): A simple test for PAD, comparing blood pressure in the ankles to that in the arms.
Duplex Ultrasound: Used to visualize arteries and assess blood flow, particularly in the carotid arteries and peripheral arteries.
Computed Tomography Angiography (CTA) or Magnetic Resonance Angiography (MRA): Provide detailed images of blood vessels.
Invasive Angiography: A procedure where contrast dye is injected into arteries and X-rays are taken to visualize blockages. Considered the gold standard for assessing the severity of stenosis but is invasive.
Coronary Artery Calcium (CAC) Scoring: A CT scan that measures the amount of calcium in the coronary arteries, which is indicative of atherosclerotic plaque burden.
Atherosclerosis: Management
Management of atherosclerosis focuses on preventing its development and progression, managing symptoms, and preventing acute cardiovascular events.
Lifestyle Modifications:
Healthy Diet: Low in saturated and trans fats, cholesterol, and sodium; rich in fruits, vegetables, whole grains, and lean protein.
Regular Exercise: At least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week.
Weight Management: Achieving and maintaining a healthy body mass index (BMI).
Smoking Cessation: The single most important lifestyle change for smokers.
Blood Pressure Control: Maintaining blood pressure within target ranges (e.g., < 130/80 mmHg for most adults).
Diabetes Management: Maintaining blood glucose levels within target ranges.
Pharmacological Management:
Statins: Cholesterol-lowering medications that are the cornerstone of atherosclerosis prevention and treatment. They reduce LDL cholesterol and have pleiotropic anti-inflammatory effects.
Antiplatelet Agents: Medications like aspirin and clopidogrel reduce the risk of blood clots forming on atherosclerotic plaques, preventing MI and stroke. Aspirin is often recommended for primary prevention in individuals at high risk and for secondary prevention in those with established cardiovascular disease.
Blood Pressure Medications: Various classes (e.g., ACE inhibitors, ARBs, calcium channel blockers, diuretics) are used to control hypertension.
Diabetes Medications: Used to manage blood glucose levels in patients with diabetes.
Other Lipid-Lowering Agents: Ezetimibe, PCSK9 inhibitors, and fibrates may be used in addition to statins to further lower cholesterol or triglycerides.
Revascularization Procedures:
Percutaneous Coronary Intervention (PCI): Also known as angioplasty with stent placement. A minimally invasive procedure to open narrowed or blocked coronary arteries.
Coronary Artery Bypass Grafting (CABG): A surgical procedure to create new pathways for blood flow around blocked coronary arteries using grafts from other blood vessels.
Carotid Endarterectomy or Stenting: Procedures to remove plaque or place a stent in narrowed carotid arteries to reduce stroke risk.
Peripheral Artery Angioplasty or Bypass Surgery: Procedures to restore blood flow in narrowed or blocked arteries in the limbs.
Monckeberg’s Medial Calcific Sclerosis
As mentioned earlier, this type involves calcification of the media of muscular arteries. It is often asymptomatic and does not typically lead to luminal narrowing or ischemia. However, the calcification can make arteries rigid, potentially affecting blood pressure measurements and increasing the risk of arterial injury during surgical procedures. It is more prevalent in individuals with diabetes and chronic kidney disease.
Arteriolosclerosis
This affects small arteries and arterioles and is strongly associated with hypertension and diabetes.
Hyaline Arteriolosclerosis: The hyaline thickening leads to luminal narrowing, which can cause ischemia in the tissues supplied by these arterioles. In the kidneys, it contributes to nephrosclerosis and chronic kidney disease.
Hyperplastic Arteriolosclerosis: Severe luminal narrowing can lead to significant reduction in blood flow and tissue ischemia. In the kidneys, it is associated with malignant hypertension and can cause acute kidney injury.
Prognosis and Complications
The prognosis of arteriosclerosis, particularly atherosclerosis, depends on the extent and location of the disease, the presence of risk factors, and the effectiveness of management. It is a progressive disease, and complications can be severe and life-threatening.
Complications of Atherosclerosis:
Myocardial Infarction
Stroke
Peripheral Artery Disease complications (critical limb ischemia, amputation)
Renal failure
Mesenteric ischemia
Aneurysm formation and rupture (weakening of the arterial wall due to plaque formation can lead to dilation and rupture, particularly in the aorta).
Related Topics
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

