Hematologic Disorders
Subtopic:
Leukemia
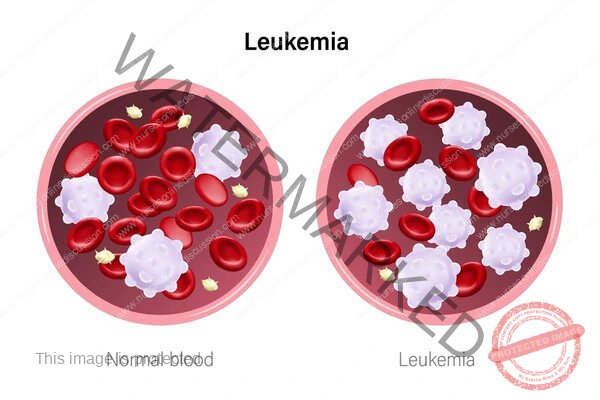
Leukemia is a malignant disorder originating in the hematopoietic stem cells of the bone marrow. It is characterized by the uncontrolled proliferation and accumulation of abnormal, immature, or mature white blood cells (leukemia cells) in the bone marrow and peripheral blood.
These abnormal cells disrupt normal hematopoiesis, leading to a deficiency in the production of functional red blood cells, white blood cells, and platelets. Leukemia is considered a systemic cancer, affecting the blood and bone marrow throughout the body, rather than forming a localized solid tumor. The name “leukemia” reflects the often elevated white blood cell count observed in affected individuals.
Classification
Leukemia is classified based on the speed of disease progression and the type of white blood cell affected. This classification is critical for determining the appropriate treatment strategy and prognosis.
Based on Speed of Progression:
Acute Leukemia: Rapid onset and progression. Involves the proliferation of very immature blast cells that are unable to mature and function normally. Requires immediate and aggressive treatment.
Chronic Leukemia: Slower onset and progression. Involves the proliferation of more mature, but still abnormal, blood cells. Symptoms may be mild or absent for a significant period.
Based on Type of White Blood Cell Affected:
Myeloid Leukemia: Arises from myeloid progenitor cells, which normally differentiate into granulocytes (neutrophils, eosinophils, basophils), monocytes, erythrocytes (red blood cells), and megakaryocytes (platelets).
Lymphoid Leukemia: Arises from lymphoid progenitor cells, which normally differentiate into lymphocytes (B cells, T cells, and natural killer cells).
Combining these criteria yields the four major types:
Acute Myeloid Leukemia (AML): Rapid proliferation of myeloid blasts. Predominantly affects adults.
Acute Lymphoblastic Leukemia (ALL): Rapid proliferation of lymphoid blasts (lymphoblasts). Most common childhood cancer.
Chronic Myeloid Leukemia (CML): Slow proliferation of myeloid cells, characterized by the Philadelphia chromosome. Primarily affects adults.
Chronic Lymphocytic Leukemia (CLL): Slow proliferation of mature B lymphocytes. Most common chronic leukemia in adults.
Other less common types include Hairy Cell Leukemia, Large Granular Lymphocytic Leukemia, and Juvenile Myelomonocytic Leukemia.
Pathogenesis and Etiology
Leukemia originates from genetic alterations (mutations) within a single hematopoietic stem cell or progenitor cell in the bone marrow. These mutations disrupt the intricate balance of cell proliferation, differentiation, and apoptosis.
The mutated cell gains a selective advantage, leading to its uncontrolled clonal expansion.
Pathogenesis:
Acute Leukemias: The genetic lesions primarily block the differentiation of immature progenitor cells, leading to the accumulation of non-functional blasts in the bone marrow. This accumulation suppresses normal hematopoiesis, resulting in pancytopenia (deficiency of red blood cells, normal white blood cells, and platelets). The blasts can also infiltrate extramedullary sites.
Chronic Leukemias: The genetic abnormalities typically affect pathways regulating cell survival and proliferation, leading to the accumulation of more mature, but functionally impaired, cells.
CML: Driven by the BCR-ABL1 fusion gene, a product of the Philadelphia chromosome translocation (t(9;22)). This gene encodes a hyperactive tyrosine kinase that promotes uncontrolled myeloid cell proliferation.
CLL: Involves complex genetic and epigenetic changes leading to the accumulation of abnormal B lymphocytes that resist apoptosis.
Etiology and Risk Factors: While the precise cause is often unknown, several factors are associated with an increased risk:
Exposure to Ionizing Radiation: High-dose radiation is a known risk factor for AML and CML.
Exposure to Certain Chemicals: Benzene and certain chemotherapy agents (alkylating agents, topoisomerase II inhibitors) are linked to increased risk of AML and ALL.
Smoking: Increases the risk of AML.
Genetic Syndromes: Conditions like Down syndrome, Fanconi anemia, and Bloom syndrome are associated with a higher incidence of specific leukemias.
Certain Hematologic Disorders: Myelodysplastic syndromes and myeloproliferative neoplasms can transform into AML.
Viral Infections: HTLV-1 is linked to adult T-cell leukemia/lymphoma.
Family History: A modest increase in risk is observed with a family history of leukemia.
Age and Sex: Risk profiles vary by leukemia type, with some more common in children (ALL) and others in adults (AML, CML, CLL), and a slight male predominance overall.
It is important to remember that many individuals with leukemia have no identifiable risk factors.
Signs and Symptoms
The clinical presentation of leukemia is diverse and depends on the type, rate of progression, and the extent of bone marrow failure and organ infiltration.
Symptoms of Acute Leukemia (Rapid Onset):
These symptoms are often sudden and related to the lack of normal blood cells:
Anemia: Fatigue, weakness, pallor, shortness of breath.
Neutropenia: Increased susceptibility to infections (fever, recurrent or severe infections).
Thrombocytopenia: Easy bruising, petechiae, purpura, nosebleeds, gum bleeding.
Bone/Joint Pain: Due to leukemia cell accumulation in the bone marrow.
Lymphadenopathy: Swollen lymph nodes (more prominent in ALL).
Hepatosplenomegaly: Enlarged liver and/or spleen, causing abdominal swelling or discomfort.
Constitutional Symptoms: Weight loss, loss of appetite.
CNS Symptoms: Headaches, vomiting, seizures, vision changes (due to CNS infiltration, more common in ALL).
Symptoms of Chronic Leukemia (Gradual Onset):
Often insidious, with many patients being asymptomatic at diagnosis.
Fatigue and Weakness:
Lymphadenopathy: Painless swelling of lymph nodes (especially in CLL).
Splenomegaly/Hepatomegaly: Enlarged spleen and/or liver, causing abdominal fullness or discomfort.
Constitutional Symptoms: Unexplained weight loss, fever, night sweats.
Increased Infections: Despite high white blood cell counts, the cells may be dysfunctional.
Bruising/Bleeding: Less common in early stages but can occur with advanced disease.
CML progresses through phases (chronic, accelerated, blast), and symptoms may worsen and resemble acute leukemia in the later stages.
Diagnosing Leukemia: The Process
Diagnosis relies on a combination of clinical evaluation and laboratory tests to identify abnormal blood cells and characterize the specific type of leukemia.
Complete Blood Count (CBC) with Differential: Initial blood test often showing abnormal white blood cell counts (high, normal, or low), presence of blasts in acute leukemia, anemia, and thrombocytopenia.
Peripheral Blood Smear: Microscopic examination of blood to assess cell morphology and identify blasts or other abnormal cells.
Bone Marrow Aspiration and Biopsy: The definitive diagnostic procedure. Samples are examined to determine blast percentage, cellularity, and cell morphology.
Cytogenetic Analysis: Analysis of chromosomes to identify specific abnormalities like the Philadelphia chromosome (CML) or other translocations (AML, ALL). Crucial for classification and prognosis.
Molecular Genetic Testing: Detects specific gene mutations or rearrangements, providing prognostic information and identifying targets for therapy.
Immunophenotyping: Uses techniques like flow cytometry to identify surface markers on leukemia cells, determining lineage (myeloid vs. lymphoid) and subtype.
Lumbar Puncture: Performed in some cases (especially ALL) to check for leukemia cells in the cerebrospinal fluid.
Imaging Studies: May be used to assess organ involvement (chest X-ray, CT, MRI).
Treating Leukemia: Approaches and Therapies
Leukemia treatment is highly individualized based on the type, subtype, patient characteristics, and presence of specific genetic abnormalities. The goal is to achieve remission and prevent relapse while managing symptoms and complications.
Treatment of Acute Leukemia (AML and ALL): Intensive, multi-phase therapy.
Induction Chemotherapy: High-dose chemotherapy to eliminate leukemia blasts and achieve remission.
Consolidation/Intensification Therapy: Additional chemotherapy cycles to eradicate residual leukemia cells and prevent relapse.
Maintenance Therapy: Lower-dose therapy over a longer period (primarily for ALL) to prevent relapse.
CNS Prophylaxis: Treatment to prevent or treat leukemia in the central nervous system (especially for ALL).
Hematopoietic Stem Cell Transplantation (HSCT): Potentially curative, involving replacing diseased bone marrow with healthy stem cells. Used for high-risk disease or relapse.
Treatment of Chronic Leukemia (CML and CLL): Often less intensive initially.
CML: Primarily treated with Tyrosine Kinase Inhibitors (TKIs) (e.g., imatinib), which target the BCR-ABL1 protein. HSCT is an option for TKI resistance or advanced phase disease.
CLL: May involve Observation (“Watch and Wait”) for asymptomatic early-stage disease. Treatment for symptomatic or advanced disease includes Chemotherapy, Targeted Therapies (e.g., BTK inhibitors, BCL-2 inhibitors), and Monoclonal Antibodies. HSCT is rarely used.
Supportive Care: Crucial throughout treatment. Includes blood transfusions, infection prevention and treatment, bleeding management, pain control, nutritional support, and psychosocial support.
Prognosis and Potential Challenges
The prognosis for leukemia varies widely. Factors influencing prognosis include the specific type and subtype, the patient’s age and overall health, and the presence of certain genetic abnormalities.
Prognosis:
Childhood ALL generally has a favorable prognosis with high cure rates.
Adult AML prognosis is more variable.
CML prognosis is significantly improved with TKIs, allowing many patients a near-normal lifespan.
CLL is often a chronic, indolent disease, but can be challenging to cure with conventional therapy.
Potential Complications:
Infections: Due to compromised immune function.
Bleeding: Due to low platelet counts.
Anemia: Causing fatigue.
Organ Dysfunction: Due to leukemia cell infiltration.
Tumor Lysis Syndrome: Metabolic complication during initial treatment.
Graft-versus-Host Disease (GVHD): Complication of allogeneic HSCT.
Relapse: Return of the disease.
Secondary Malignancies: Increased risk after certain treatments.
Treatment-Related Toxicity: Side effects from therapies.
Related Topics
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

