Microbiology
Subtopic:
Fluid & Electrolyte Imbalance
Body Fluid and Electrolytes
Body fluid refers to the water content within the body, which serves as a medium for numerous physiological processes. Electrolytes are minerals that carry an electric charge when dissolved in body fluid. They are crucial for maintaining fluid balance, nerve and muscle function, acid-base balance, and other vital processes.
Fluid: Approximately 50-60% of an adult’s body weight is water. This percentage varies with age, sex, and body fat content (lean tissue contains more water).
Electrolytes: Key electrolytes include:
Cations (positively charged): Sodium (Na+), Potassium (K+), Calcium (Ca2+), Magnesium (Mg2+).
Anions (negatively charged): Chloride (Cl−), Bicarbonate (HCO3−), Phosphate (PO43−), Sulfate (SO42−), Proteins.
2. Fluid Compartments
Body water is distributed among several compartments, separated by semipermeable membranes.
Intracellular Fluid (ICF): Fluid within the cells. It constitutes approximately two-thirds of total body water. The primary cation in ICF is K+, and the primary anions are phosphates and proteins.
Extracellular Fluid (ECF): Fluid outside the cells. It constitutes approximately one-third of total body water. The primary cation in ECF is Na+, and the primary anion is Cl−. ECF is further divided into:
Interstitial Fluid: Fluid in the spaces between cells (interstitium). It makes up about 80% of the ECF.
Intravascular Fluid (Plasma): The liquid component of blood, found within blood vessels. It makes up about 20% of the ECF. Plasma contains a higher concentration of protein (albumin) than interstitial fluid, which contributes to oncotic pressure.
Transcellular Fluid: A small, specialized portion of ECF found in specific cavities (e.g., cerebrospinal fluid, synovial fluid, pleural fluid, peritoneal fluid, digestive secretions).
3. Movement of Fluid and Electrolytes
Movement of water and electrolytes between compartments occurs through various passive and active processes:
Osmosis: The movement of water across a selectively permeable membrane from an area of lower solute concentration to an area of higher solute concentration. This is the primary mechanism regulating water movement between ICF and ECF, driven by osmotic pressure (determined by solute concentration, particularly electrolytes like Na+).
Diffusion: The movement of solutes from an area of higher concentration to an area of lower concentration, down their concentration gradient. This can occur across cell membranes or through interstitial fluid.
Facilitated Diffusion: Diffusion that requires the assistance of membrane proteins (channels or carriers) but does not require energy.
Active Transport: The movement of solutes against their concentration gradient, requiring energy (ATP) and membrane proteins (pumps), e.g., the Na+/K+ pump.
Hydrostatic Pressure: The pressure exerted by a fluid within a confined space (e.g., blood pressure in capillaries). It tends to push fluid out of the compartment.
Oncotic Pressure (Colloid Osmotic Pressure): The osmotic pressure exerted by large molecules, particularly proteins (like albumin) in the plasma, that cannot easily cross capillary walls. It tends to pull fluid into the compartment.
Fluid movement across capillary walls is governed by the balance between hydrostatic pressure and oncotic pressure (Starling forces).
4. Regulation of Fluid Balance
Maintaining fluid balance involves regulating both fluid intake and output, primarily controlled by thirst and hormonal mechanisms.
Thirst Mechanism: Triggered by osmoreceptors in the hypothalamus that sense increased ECF osmolality (indicating dehydration) and by baroreceptors that sense decreased blood volume.
Antidiuretic Hormone (ADH), also known as Vasopressin: Produced by the hypothalamus and released by the posterior pituitary gland. ADH increases water reabsorption in the renal tubules, reducing water excretion and concentrating urine. Release is stimulated by increased ECF osmolality or decreased blood volume/pressure.
Renin-Angiotensin-Aldosterone System (RAAS): Activated by decreased renal blood flow or Na+ levels. Renin release leads to the production of Angiotensin II, a potent vasoconstrictor that also stimulates the release of Aldosterone from the adrenal cortex.
Angiotensin II: Causes vasoconstriction, increases blood pressure, stimulates ADH release, and promotes thirst.
Aldosterone: Acts on the renal tubules to increase Na+ and water reabsorption and increase K+ excretion. This expands ECF volume.
Atrial Natriuretic Peptide (ANP) and Brain Natriuretic Peptide (BNP): Hormones released by the heart in response to increased atrial or ventricular stretch (indicating increased blood volume). ANP and BNP promote Na+ and water excretion by the kidneys, inhibit RAAS, and cause vasodilation, thus reducing blood volume and pressure.
5. Regulation of Electrolyte Balance
Electrolyte balance is tightly regulated through intake, absorption, distribution, and excretion, with the kidneys playing a central role. Hormones also influence the balance of specific electrolytes.
Sodium (Na+): The primary determinant of ECF volume and osmolality. Regulation is closely linked to fluid balance via RAAS and ANP/BNP. Kidneys regulate Na+ excretion and reabsorption.
Potassium (K+): The primary intracellular cation, crucial for nerve and muscle excitability, including cardiac function. Regulation is primarily by the kidneys, influenced by Aldosterone (promotes K+ excretion) and acid-base status.
Calcium (Ca2+): Important for bone health, nerve and muscle function, blood clotting, and cellular signaling. Regulated by Parathyroid Hormone (PTH), Vitamin D, and Calcitonin, which influence Ca2+ absorption from the gut, reabsorption in the kidneys, and release from bone.
Magnesium (Mg2+): Involved in enzyme activity, nerve and muscle function, and DNA synthesis. Regulated by the kidneys and influenced by PTH. Often imbalances mirror those of K+ and Ca2+.
Phosphate (PO43−): A component of bone, ATP, and nucleic acids, involved in energy metabolism and acid-base buffering. Regulated by the kidneys, influenced by PTH and Vitamin D (PTH decreases phosphate reabsorption, Vitamin D increases intestinal absorption).
6. Fluid Volume Imbalances
Imbalances in the total amount of water in the body, often coupled with changes in sodium concentration.
Fluid Volume Deficit (FVD) / Hypovolemia: A state of decreased intravascular volume.
Causes: Excessive fluid loss (hemorrhage, vomiting, diarrhea, excessive sweating, polyuria from diabetes mellitus or insipidus), inadequate fluid intake, third-spacing (fluid shifting into interstitial or transcellular spaces, e.g., burns, sepsis, ascites).
Signs & Symptoms: Thirst, dry mucous membranes, decreased skin turgor, decreased urine output (oliguria), concentrated urine, weakness, dizziness, orthostatic hypotension (drop in BP upon standing), tachycardia, flattened neck veins, cool and clammy skin. In severe FVD, signs of shock may be present (hypotension, weak pulse, altered mental status).
Management Principles: Identify and treat the underlying cause. Administer fluid replacement (oral rehydration for mild FVD, intravenous fluids – crystalloids or colloids – for moderate to severe FVD). Monitor vital signs, intake and output, and laboratory values.
Fluid Volume Excess (FVE) / Hypervolemia: A state of increased intravascular volume.
Causes: Excessive fluid intake (especially intravenous fluids), decreased fluid excretion (renal failure, heart failure, liver failure, conditions causing excessive Aldosterone or ADH release).
Signs & Symptoms: Weight gain, peripheral edema (swelling in extremities), pulmonary edema (shortness of breath, crackles in lungs, cough), distended neck veins, increased blood pressure, bounding pulse, polyuria (if kidneys are attempting to excrete excess fluid).
Management Principles: Identify and treat the underlying cause. Restrict fluid and sodium intake. Administer diuretics to promote fluid excretion. Monitor vital signs, intake and output, weight, and laboratory values.
7. Electrolyte Imbalances
Deviations from the normal concentration of specific electrolytes in the body fluids.
Sodium Imbalances: Primarily affect ECF volume and osmolality.
Hyponatremia (Low Serum Na+ < 135 mEq/L):
Causes: Excessive water intake, Syndrome of Inappropriate ADH (SIADH), diuretic use, fluid loss replaced only with water, renal failure, heart failure, liver failure.
Signs & Symptoms: Neurological symptoms are common due to osmotic shift of water into brain cells: headache, confusion, lethargy, seizures, coma. Muscle cramps, weakness.
Management Principles: Treat the underlying cause. Fluid restriction (if due to excess water). Administration of hypertonic saline (for severe, symptomatic hyponatremia). Careful monitoring to avoid rapid correction, which can cause osmotic demyelination syndrome.
Hypernatremia (High Serum Na+ > 145 mEq/L):
Causes: Inadequate water intake, excessive water loss (diabetes insipidus, osmotic diuresis, excessive sweating, diarrhea), excessive sodium intake/administration.
Signs & Symptoms: Primarily neurological due to osmotic shift of water out of brain cells: restlessness, irritability, lethargy, seizures, coma. Thirst (if conscious). Dry mucous membranes, decreased urine output.
Management Principles: Treat the underlying cause. Administer hypotonic fluids (e.g., 0.45% saline or D5W) to gradually lower serum sodium. Careful monitoring to avoid rapid correction, which can cause cerebral edema.
Potassium Imbalances: Primarily affect neuromuscular and cardiac function.
Hypokalemia (Low Serum K+ < 3.5 mEq/L):
Causes: Excessive K+ loss (diuretics, diarrhea, vomiting, hyperaldosteronism), inadequate K+ intake, shift of K+ into cells (alkalosis, insulin administration).
Signs & Symptoms: Muscle weakness, fatigue, leg cramps, decreased bowel motility (constipation, ileus), cardiac arrhythmias (potentially life-threatening), flattened T waves or prominent U waves on ECG.
Management Principles: Treat the underlying cause. Administer potassium replacement (oral for mild, intravenous for moderate to severe – MUST be administered cautiously and diluted, never IV push). Monitor cardiac rhythm and serum K+ levels.
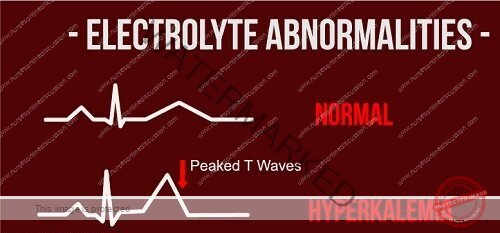
Hyperkalemia (High Serum K+ > 5.0 mEq/L):
Causes: Decreased K+ excretion (renal failure, hypoaldosteronism, potassium-sparing diuretics), excessive K+ intake/administration, shift of K+ out of cells (acidosis, tissue injury, certain medications).
Signs & Symptoms: Muscle weakness, paralysis, paresthesias, potentially life-threatening cardiac arrhythmias (peaked T waves, widened QRS, sine wave on ECG), abdominal cramping, diarrhea.
Management Principles: Treat the underlying cause. Medications to shift K+ into cells (insulin and glucose, sodium bicarbonate, beta-agonists). Medications to remove K+ from the body (kayexalate – sodium polystyrene sulfonate, diuretics). Calcium gluconate to stabilize cardiac cell membranes (does not lower K+). Dialysis for severe, refractory hyperkalemia. Monitor cardiac rhythm and serum K+ levels.
Calcium Imbalances: Affect neuromuscular excitability, bone health, and cardiac function.
Hypocalcemia (Low Serum Ca2+ < 8.5 mg/dL or ionized Ca2+ < 4.5 mg/dL):
Causes: Decreased PTH (hypoparathyroidism), Vitamin D deficiency, renal failure, pancreatitis, massive blood transfusion (citrate binds Ca2+), certain medications.
Signs & Symptoms: Increased neuromuscular excitability: muscle cramps, twitching (Chvostek’s sign – facial twitching with tapping of facial nerve; Trousseau’s sign – carpal spasm with inflation of blood pressure cuff), paresthesias (tingling), tetany, seizures. Prolonged QT interval on ECG.
Management Principles: Treat the underlying cause. Administer calcium replacement (oral for mild, intravenous for acute/severe – administer slowly). Administer Vitamin D if deficient. Monitor serum Ca2+ and ECG.
Hypercalcemia (High Serum Ca2+ > 10.5 mg/dL or ionized Ca2+ > 5.5 mg/dL):
Causes: Increased PTH (hyperparathyroidism), malignancy (bone metastases, PTH-related peptide secretion), excessive Vitamin D intake, prolonged immobilization.
Signs & Symptoms: Decreased neuromuscular excitability: fatigue, weakness, lethargy, decreased reflexes. Gastrointestinal symptoms: nausea, vomiting, constipation. Renal symptoms: polyuria, polydipsia, kidney stones. Cardiac: shortened QT interval on ECG, arrhythmias. Bone pain.
Management Principles: Treat the underlying cause. Hydration with normal saline to promote Ca2+ excretion. Loop diuretics (after hydration). Medications to inhibit bone resorption (bisphosphonates, calcitonin). Dialysis for severe, symptomatic hypercalcemia.
Magnesium Imbalances: Often associated with other electrolyte imbalances, affect neuromuscular and cardiac function.
Hypomagnesemia (Low Serum Mg2+ < 1.5 mEq/L):
Causes: Inadequate intake, impaired absorption (malabsorption syndromes, chronic diarrhea), excessive loss (diuretics, alcoholism, certain medications), often coexists with hypokalemia and hypocalcemia.
Signs & Symptoms: Increased neuromuscular excitability: tremors, twitching, hyperactive reflexes, seizures. Cardiac arrhythmias (especially torsades de pointes). Weakness, fatigue.
Management Principles: Treat the underlying cause. Administer magnesium replacement (oral for mild, intravenous for moderate to severe). Correct associated electrolyte imbalances. Monitor serum Mg2+ and ECG.
Hypermagnesemia (High Serum Mg2+ > 2.5 mEq/L):
Causes: Decreased renal excretion (renal failure), excessive magnesium intake/administration (antacids, laxatives, IV magnesium).
Signs & Symptoms: Decreased neuromuscular excitability: muscle weakness, decreased deep tendon reflexes, lethargy. Respiratory depression. Hypotension. Bradycardia, cardiac arrest. Nausea, vomiting.
Management Principles: Treat the underlying cause. Discontinue magnesium intake. Administer IV fluids and loop diuretics to enhance renal excretion (if renal function is adequate). Calcium gluconate to antagonize neuromuscular and cardiac effects. Dialysis for severe hypermagnesemia in renal failure.
Phosphate Imbalances: Affect energy metabolism, bone, and nerve/muscle function.
Hypophosphatemia (Low Serum PO43− < 2.5 mg/dL):
Causes: Inadequate intake/absorption, increased excretion (diuretics, hyperparathyroidism), intracellular shift (refeeding syndrome, respiratory alkalosis).
Signs & Symptoms: Often non-specific until severe: muscle weakness, respiratory failure, cardiac dysfunction, confusion, seizures.
Management Principles: Treat the underlying cause. Administer phosphate replacement (oral for mild, intravenous for severe).
Hyperphosphatemia (High Serum PO43− > 4.5 mg/dL):
Causes: Decreased renal excretion (renal failure), excessive intake/administration, extracellular shift (tissue injury, chemotherapy – tumor lysis syndrome).
Signs & Symptoms: Often asymptomatic. Symptoms may be related to associated hypocalcemia (tetany, paresthesias) due to calcium-phosphate precipitation. Soft tissue calcification in chronic cases.
Management Principles: Treat the underlying cause. Phosphate binders with meals. Administer IV fluids and diuretics to enhance renal excretion (if renal function is adequate). Dialysis for severe hyperphosphatemia in renal failure.
8. Diagnosis of Fluid and Electrolyte Imbalances
Diagnosis relies on integrating information from several sources:
Clinical Assessment: Detailed history (fluid intake/output, symptoms, medications, underlying conditions), physical examination (vital signs, skin turgor, mucous membranes, presence of edema, neurological status, lung sounds).
Laboratory Tests:
Serum Electrolytes: Measurement of Na+, K+, Cl−, HCO3−, Glucose, BUN (Blood Urea Nitrogen), Creatinine.
Serum Osmolality: Reflects the concentration of solutes in the serum, primarily Na+, Urea, and Glucose. Helps assess hydration status and detect osmolality imbalances.
Urine Studies: Urine output, urine specific gravity (reflects urine concentration), urine osmolality, urine electrolyte levels. Provide information about kidney function and the body’s attempt to conserve or excrete fluid and electrolytes.
Arterial Blood Gas (ABG): Assesses acid-base status, which is closely linked to electrolyte balance (e.g., K+ shifts in acidosis/alkalosis).
Other Electrolyte Levels: Serum Calcium, Magnesium, Phosphate.
9. General Management Principles
Management of fluid and electrolyte imbalances involves a multi-faceted approach:
Identify and Treat the Underlying Cause: Addressing the root problem is essential for long-term correction.
Fluid Management:
For FVD: Administer appropriate fluids (oral or intravenous) to restore intravascular volume.
For FVE: Restrict fluid and sodium intake, administer diuretics.
Electrolyte Correction:
For Deficiencies: Administer the deficient electrolyte (oral or intravenous).
For Excesses: Promote excretion of the excess electrolyte (diuretics, dialysis) or shift it into cells.
Monitoring: Close monitoring of vital signs, intake and output, daily weight, clinical status, and serial laboratory electrolyte levels is crucial to assess the response to treatment and detect complications.
Patient Education: Educating patients about their condition, medications, dietary modifications (e.g., fluid or sodium restriction, potassium-rich foods), and the importance of reporting symptoms.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

