Eye Conditions
Subtopic:
Corneal Ulcer
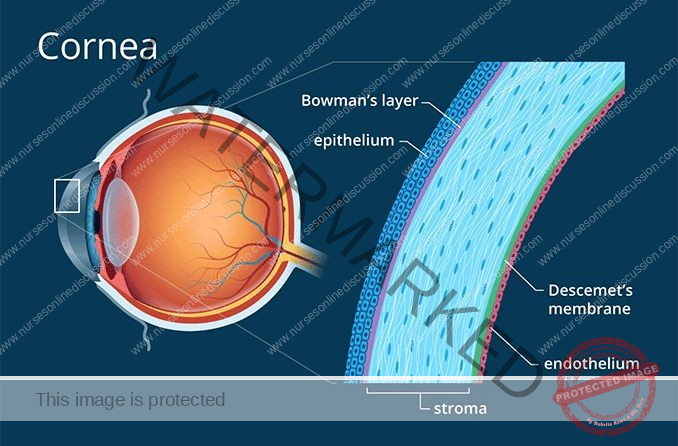
Corneal ulcers are open wounds or breaks in the surface layer (epithelium) of the cornea. This disruption of the corneal surface is accompanied by inflammation in the underlying corneal tissue. The cornea is the clear, dome-shaped front part of the eye, covering the iris and pupil, and plays a vital role in focusing light.
These ulcers can often be seen as areas on the cornea that appear less clear than the surrounding tissue, ranging in color from a hazy gray to an opaque white. While some ulcers are readily visible to the naked eye, others may be very small and require magnification to be detected.

The cornea’s clarity is essential for proper vision, as it helps to focus light onto the retina. Corneal ulcers pose a significant threat to vision if left untreated, potentially leading to permanent vision loss.
Cornea Structure
The cornea is the clear front surface of the eye, acting like a window. It sits in front of the iris, which is the colored part of the eye. Between the cornea and the iris is a space filled with a fluid called aqueous humor, known as the anterior chamber of the eye.
Causes of Corneal Ulcers
Corneal ulcers can arise from various factors, broadly categorized as:
Infections:
Bacterial Infections: Common bacteria like Staphylococcus and Pseudomonas are frequent causes. These bacteria can invade the cornea, especially if its surface has been damaged in some way. Individuals who wear contact lenses have a higher risk, particularly if they don’t follow proper hygiene practices or wear their lenses for extended periods.
Viral Infections: The herpes simplex virus (the same virus that causes cold sores) and the varicella-zoster virus (which causes chickenpox and shingles) are known to cause corneal ulcers. These viral infections can sometimes recur, leading to ongoing (chronic) ulceration of the cornea.
Fungal Infections: These infections are more likely to occur with improper care of contact lenses or after prolonged use of corticosteroid eye drops. Common fungal culprits include Fusarium and Candida species.
Trauma:
Mechanical Injuries: Small cuts or scratches caused by objects like metal shavings, wood splinters, glass fragments, or any other foreign particle can injure the cornea. This damage creates an opening where infection can take hold. Even seemingly minor injuries can lead to significant problems if not treated promptly and correctly.
Chemical Burns: When the eye comes into contact with strong chemicals or irritating substances, it can cause burns on the cornea, potentially leading to ulceration. Alkali burns, caused by substances like ammonia or lye, are particularly dangerous because these chemicals can penetrate deeper into the corneal tissue.
Pre-existing Eye Conditions:
Dry Eye Syndromes: Conditions where the eyes don’t produce enough tears, like keratoconjunctivitis sicca, result in a reduced protective tear film. This makes the cornea more vulnerable to injury and subsequent infection.
Eyelid Disorders: Problems that prevent the eyelids from fully closing, such as Bell’s palsy (facial paralysis), can leave the cornea exposed to the environment, making it dry and more likely to develop an ulcer. Additionally, entropion (where the eyelid turns inward) and trichiasis (where eyelashes grow inward) can cause constant rubbing and irritation against the cornea, eventually leading to ulcer formation.
Immunological Disorders:
Autoimmune Diseases: Certain autoimmune diseases, such as rheumatoid arthritis and lupus, can increase the risk of corneal ulcers. This can happen either through direct inflammation of the eye tissues or by making the eye more susceptible to secondary infections. Furthermore, immune-related conditions like scleritis (inflammation of the white part of the eye) can also contribute to the development of corneal ulcers.
Signs and Symptoms of Corneal Ulcers
The presence of a corneal ulcer can manifest through several signs and symptoms:
Redness: The conjunctiva (the clear outer layer of the white part of the eye) and the anterior chamber (the space between the cornea and the iris) may appear red due to the widening of blood vessels in response to inflammation.
Eye Pain: The level of pain can vary from mild discomfort to severe, intense pain. Often, the pain gets worse when exposed to bright light (photophobia).
Visual Disturbance: Vision may become blurred, especially if the ulcer is located in the central part of the cornea, which is critical for focusing.
Tearing and Discharge: The affected eye may produce excessive tears. There might also be a discharge, which could be pus-like or thick.
Foreign Body Sensation: Individuals often experience a persistent feeling as if something is stuck in their eye.
Swelling: The eyelids may become swollen, and there might be noticeable swelling or puffiness around the area of the corneal ulcer.
Visible Ulcer: In some cases, a whitish or grayish, often round, spot may be visible on the normally clear cornea.

Investigations
To properly diagnose and assess a corneal ulcer, several investigations are typically performed:
Slit Lamp Examination: This is a detailed examination of the eye using a specialized microscope called a slit lamp. The intense light and magnification allow the doctor to carefully inspect the cornea for any abnormalities. Often, a special dye called fluorescein is applied to the surface of the eye. This dye highlights any defects or breaks in the corneal surface, making the ulcer more easily visible, especially when viewed under a blue light.
Microbial Cultures: To identify the specific organism causing the ulcer (bacteria, virus, or fungus), a small sample is taken from the ulcer. This can involve gently swabbing the area or taking a tiny scraping. The sample is then sent to a laboratory for analysis. Microscopy allows for direct visualization of potential pathogens. Culture involves placing the sample in a growth medium to see if any organisms multiply, identifying the specific type. Sensitivity testing determines which medications will be most effective in treating the infection.
Corneal Sensitivity Test: This test evaluates the sensitivity of the cornea to touch. A reduced sensitivity can be indicative of certain conditions, such as viral ulcers or chronic corneal problems.
Management of Corneal Ulcers
The treatment approach for corneal ulcers depends on the underlying cause and the severity of the ulcer.
Medical Treatment:
Anti-Infective Agents: These are the mainstay of treatment when an infection is present. The specific type of medication used depends on the identified organism:
Antibacterial: Antibiotic eye drops or ointments are used to combat bacterial infections.
Antiviral: Antiviral eye drops or ointments are used for viral ulcers. In some cases, oral antiviral medications may also be prescribed for a more systemic approach.
Antifungal: Antifungal eye drops or ointments are used to treat fungal infections.
Cycloplegics: These are eye drops, such as cyclopentolate or atropine, that temporarily paralyze the muscles in the eye responsible for focusing and constricting the pupil. This helps to dilate the pupil, which can relieve pain caused by spasms of the ciliary muscle (a muscle in the eye involved in focusing).
Steroids: Steroid eye drops may be considered to reduce inflammation and scarring. However, their use requires careful monitoring by an ophthalmologist and is generally only initiated once the infectious cause is under control. Using steroids too early can worsen an infection.
Surgical Management:
Surgical intervention may be necessary in certain situations:
Eyelash Removal: If an ingrown eyelash is constantly rubbing against the cornea and causing the ulcer, the offending lash, including its root, may be removed. For recurrent issues, a procedure called electrolysis can be performed to permanently destroy the hair follicle.
Eyelid Surgery: If the ulcer is being caused by an inward turning of the eyelid (entropion), which causes the eyelashes to rub against the cornea, surgery to correct the eyelid position may be required.
Corneal Transplant (Keratoplasty): In cases where the ulcer has caused significant thinning or damage to the cornea, a corneal transplant might be necessary to restore the structural integrity and clarity of the cornea. This involves replacing the damaged corneal tissue with healthy donor tissue.
Preventive Measures
Taking certain precautions can significantly reduce the risk of developing corneal ulcers:
Eye Protection: Always wear appropriate protective eyewear when engaging in activities that pose a risk of eye injury. This includes working with tools, chemicals, or in environments where there might be flying particles or debris.
Proper Contact Lens Care: If you wear contact lenses, meticulous hygiene is essential:
Always wash your hands thoroughly with soap and water before handling contact lenses.
Never use saliva to wet contact lenses. Your mouth contains bacteria that can be harmful to the cornea.
Avoid using tap water to clean or store lenses, as it can contain microorganisms that can cause serious eye infections.
Do not wear contact lenses overnight unless they are specifically designed and approved for extended wear by your eye doctor.
Lubrication: If you have dry eyes or if your eyelids don’t close completely, use artificial tear eye drops regularly to keep the cornea moist and prevent it from drying out and becoming more vulnerable to damage.
Early Treatment: If you experience persistent redness or irritation in your eye that doesn’t improve with over-the-counter lubricating eye drops within 24 hours, seek medical attention from an eye care professional promptly.
Complications
If left untreated or not managed effectively, corneal ulcers can lead to serious complications:
Corneal Scarring: Even after a corneal ulcer heals, it can leave behind a scar on the cornea. If this scar is located in the central part of the cornea, it can permanently impair vision.
Secondary Infections: An existing corneal ulcer can become infected with additional organisms, worsening the initial infection and making treatment more challenging.
Corneal Perforation: In severe cases, the ulcer can erode through the entire thickness of the cornea, creating a hole or perforation. This is a serious complication that can potentially lead to the loss of the eye.
Endophthalmitis: This is a severe infection of the inner structures of the eye. It’s a rare but serious complication that can arise from an untreated corneal ulcer and can cause significant vision loss.
Blindness: If corneal ulcers are not treated appropriately and in a timely manner, they can ultimately lead to significant vision loss or even complete blindness.
Additional Preventive Measures
Always wear eye protection when using power tools or in situations where small particles could enter the eye (such as when using a grinding wheel or a weed whacker).
If you suffer from dry eyes or your eyelids do not close completely, consistently use artificial tear drops to keep your eyes lubricated.
If your eye becomes red and irritated and the condition worsens or doesn’t improve after a day of using over-the-counter (OTC) eye drops, contact an ophthalmologist without delay.
Individuals who wear contact lenses need to be especially diligent about their lens care routine.
Always ensure your hands are clean by washing them thoroughly before handling contact lenses.
Never use saliva to wet or lubricate contact lenses, as your mouth contains bacteria that can be harmful to your cornea.
Remove your contact lenses every evening and clean them according to the instructions provided by your eye doctor or the lens manufacturer.
Avoid using tap water to clean your contact lenses or their case.
Never sleep in contact lenses that are not specifically designed and approved for overnight wear.
Store your contact lenses overnight in a disinfecting solution recommended by your eye doctor.
If your eyes become irritated, remove your contact lenses and refrain from wearing them until the irritation and redness have completely resolved.
Clean your contact lens case regularly and replace it as recommended by your eye doctor. Carefully read and follow all instructions regarding contact lens care that are provided by the lens manufacturer. Consider using daily disposable contact lenses to minimize the risk of infection.
NURSING CARE PLAN FOR CORNEAL ULCER
Assessment: Observation of severe eye pain, redness, tearing, and photophobia.
Nursing Diagnosis: Acute pain related to inflammation and ulceration of the cornea as evidenced by patient verbalizing severe eye pain and sensitivity to light.
Goals/Expected Outcomes: To reduce eye pain and discomfort within 3 days.
Interventions:
Assess pain level using a recognized pain scale to effectively quantify the patient’s pain and monitor any changes in pain intensity over time.
Administer prescribed analgesics and/or topical anesthetics as ordered by the healthcare provider to manage pain.
Apply cool compresses to the affected eye to help alleviate discomfort and reduce inflammation.
Encourage the patient to rest in a dimly lit room and avoid bright lights to minimize light exposure, thereby reducing photophobia.
Rationale:
Pain assessment is crucial for evaluating the effectiveness of pain management interventions and adjusting the plan as needed.
Analgesics and topical anesthetics are essential for directly reducing pain sensations and providing relief to the patient.
Cool compresses help to reduce inflammation in the affected eye and soothe the area, contributing to pain reduction.
Resting in a dimly lit environment minimizes light exposure to the sensitive eye, which is a key factor in reducing photophobia and associated discomfort.
Evaluation: Patient reports a decrease in eye pain and discomfort, with less sensitivity to light.
Assessment: Presence of a white or grayish spot on the cornea and purulent discharge.
Nursing Diagnosis: Risk for infection related to bacterial or fungal invasion of the corneal ulcer.
Goals/Expected Outcomes: To prevent the spread of infection and promote healing within 1 week.
Interventions:
Administer prescribed antibiotic or antifungal eye drops as ordered to target the specific type of infection.
Educate the patient on the critical importance of completing the full course of medication, even if symptoms improve, to ensure complete eradication of the infection.
Instruct the patient on proper hand hygiene practices, emphasizing the need to wash hands thoroughly before and after applying eye drops to prevent contamination.
Advise the patient to avoid the use of contact lenses until the corneal ulcer has completely healed to prevent further complications and hinder the healing process.
Rationale:
Antibiotics or antifungals are essential medications for treating the underlying infection and promoting the corneal healing process.
Completing the full course of medication is vital to ensure that the infection is fully eradicated and to minimize the risk of recurrence or antibiotic resistance.
Proper hand hygiene significantly reduces the risk of further contamination and spread of infection to the affected eye and surrounding areas.
Contact lenses can aggravate the corneal ulcer, potentially leading to complications and delaying the healing process, therefore avoidance is crucial.
Evaluation: Patient’s eye is healing, infection is contained, and discharge has subsided.
Assessment: Assessment of visual acuity and patient’s ability to perform daily activities.
Nursing Diagnosis: Impaired vision related to corneal ulceration as evidenced by blurred vision and difficulty performing daily activities.
Goals/Expected Outcomes: To maintain or improve vision and functional ability within 2 weeks.
Interventions:
Perform visual acuity tests regularly to monitor any changes in vision and track the progression of the ulcer’s impact.
Educate the patient on the crucial need to avoid activities that strain the eyes, such as reading or using screens for extended periods, to promote healing.
Encourage the use of protective eyewear to shield the eye from dust, bright sunlight, and foreign particles that could cause further irritation or injury.
Arrange for assistance with daily activities as needed to ensure patient safety and well-being during the recovery period when vision may be compromised.
Rationale:
Visual acuity tests provide objective data to track the progression of the corneal ulcer and its impact on the patient’s vision over time.
Avoiding eye strain supports the natural healing process of the cornea and reduces discomfort associated with eye fatigue.
Protective eyewear is a physical barrier that prevents further injury and contamination of the affected eye from external irritants, promoting a cleaner healing environment.
Assistance with daily activities ensures the patient’s safety and overall well-being while they are experiencing vision impairment due to the corneal ulcer.
Evaluation: Patient’s vision remains stable or improves, with no significant impairment in performing daily activities.
Assessment: Patient expresses concern about potential vision loss and the appearance of the eye.
Nursing Diagnosis: Anxiety related to fear of vision loss and changes in eye appearance as evidenced by the patient expressing concern about the condition.
Goals/Expected Outcomes: To reduce anxiety and improve the patient’s understanding of the condition within 1 week.
Interventions:
Provide comprehensive information about corneal ulcers, including their causes, treatment options, and expected prognosis, to address knowledge gaps and reduce fear of the unknown.
Reassure the patient that early and appropriate treatment can effectively prevent permanent vision loss in most cases, offering hope and reducing anxiety related to worst-case scenarios.
Offer emotional support and actively encourage the patient to express their fears and concerns about their vision and eye appearance in a safe and supportive environment.
Refer the patient to a support group or counselor if anxiety persists or is severe, providing access to professional mental health resources.
Rationale:
Education empowers the patient with knowledge about their condition, reducing anxiety that stems from uncertainty and lack of information.
Reassurance helps the patient feel more confident in the treatment process and reduces fear associated with potential negative outcomes like permanent vision loss.
Emotional support fosters a therapeutic relationship and directly addresses the patient’s psychological needs related to their health condition.
Support groups or counseling can provide additional emotional and psychological support beyond what can be offered in a typical clinical setting, especially for persistent or severe anxiety.
Evaluation: Patient reports feeling less anxious and demonstrates understanding of the condition and treatment plan.
Assessment: Assessment of the patient’s adherence to treatment and follow-up care.
Nursing Diagnosis: Knowledge deficit related to unfamiliarity with the treatment regimen and follow-up care as evidenced by the patient asking questions about the medication and care plan.
Goals/Expected Outcomes: To ensure the patient understands and adheres to the treatment plan within 1 week.
Interventions:
Provide clear, step-by-step instructions on how to administer eye drops and other medications correctly, ensuring proper technique and dosage.
Educate the patient on the importance of attending all scheduled follow-up appointments to monitor healing and adjust treatment as needed.
Provide written materials or visual aids to reinforce teaching and ensure the patient has resources to refer back to at home for continued understanding.
Encourage the patient to ask questions and seek clarification about any aspect of the treatment plan they are unsure about, fostering open communication and addressing knowledge gaps.
Rationale:
Clear instructions ensure proper medication administration and enhance adherence to the prescribed treatment regimen.
Follow-up appointments are essential for monitoring the corneal ulcer’s healing progression and making any necessary adjustments to the treatment plan in a timely manner.
Written materials or visual aids enhance understanding and retention of information, particularly for complex medical instructions and care plans.
Encouraging questions ensures that the patient fully understands the treatment plan and care instructions, promoting active participation and adherence.
Evaluation: Patient demonstrates proper administration of eye drops and expresses confidence in managing the treatment plan.
Related Topics
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

