Reproductive Health
Subtopic:
Pillars of Safe Motherhood
Pillars of Safe Motherhood
Safe Motherhood
- Define safe motherhood
- Explain milestones of Safe Motherhood
- State the aims of safe motherhood
- Explain the pillars of Safe Motherhood
- Define maternal mortality
- State Causes of maternal mortality
- Explain the delays that can lead to maternal mortality
Definition
- Means that no woman and child should die or be harmed by pregnancy or birth.
- Safe motherhood: is defined as a series of initiatives, practices, protocols and service delivery guidelines designed to ensure that women receive high quality gynecological, family planning, prenatal, delivery and post partum care in order to achieve optimal health for the mother, fetus and infants during pregnancy, childbirth and post partum.
NB safe motherhood is the concept that no woman or fetus or baby should die or be harmed by pregnancy or childbirth. This is made possible by providing timely appropriate and comprehensive quality obstetric care during:
- Preconception
- Pregnancy
- Childbirth
- Puerperium
Milestones of Safe Motherhood
- The history of global safe motherhood programs begun in 1987, the global strategy for safe motherhood was launched in Nairobi, Kenya in 1987 at the international conference on safe motherhood. This conference was co-sponsored by the WHO in partnership with the World Bank, the United nation Funds for Development Activity (UNFPA) and United Nation Development Program (UNDP).
- During the program of Action of the international conference on population and Development (ICPD) in 1994, a consensus was reached that meeting the reproductive health needs of women and men is a critical requirement for human and social development.
- The conference affirmed that reproductive health care is an integral component of primary health care and should be provided in that context. The elements (components) of reproductive health have a profound impact on the course and outcome of pregnancy and health service requirements for addressing them are closely related.
- It was during this conference that consensus was built to adopt a strategy that addresses all aspects of reproductive health and provide an opportunity to develop an integrated approach to safe delivery and hence the WHO Mother Baby Package. After about 5 years of introduction of the Mother Baby Package, WHO and partners introduced the need to improve maternal health and reduce maternal mortality through making pregnancy safer strategy highlighted below.
- The making pregnancy safer strategy emphasizes the importance of the health sector interventions highlighted:
- Advocacy
- Partnerships
- Improving national capacity
- Standard setting and tool development
- Research and development
- Monitoring and evaluation
According to national and international human right treaties, safe motherhood is considered a human right issue. Therefore it is considered that maternal death is the reflection of “social disadvantage” not merely “a health disadvantage”.
Aims of safe motherhood
- To ensure that all deliveries are conducted hygienically and according to accepted medical practices, thereby preventing complications that are caused or exacerbated by poor care.
- Identify complications promptly and manage them appropriately either by treating or referring them to a higher level of care.
- Provision of high quality, culturally appropriate care, ensuring necessary follow up and linkages with other services including antenatal and post partum care as well as family planning, post abortion care and treatment of STIs.
- To enhance the quality and safety of girls‟ and women‟ lives through adaptation of a combination of health and non health related strategies.
NB:maternal and child health promotion is one of the key commitments in the WHO constitutions. Safe motherhood initiative is a global effort and it is designed to operate through its partner i.e.
- Government agencies
- NGOs
- Other groups and individuals
It aims to improve women’s health through social, community and economic interventions.
Pillars of Safe Motherhood
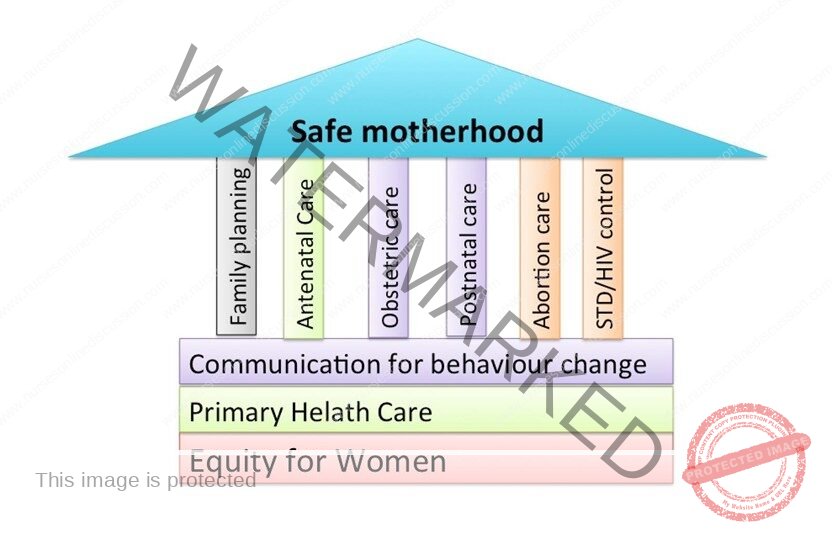
Pillars of safe motherhood
- Family planning; to ensure that individuals and couples have the information and services to plan the timing, number and spacing of pregnancies and thus the number of unsafe abortion.
- Antenatal care; to prevent complications where possible and ensure that complications of pregnancy are treated appropriately and very serious conditions referred within the shortest possible time.
- Clean/safe delivery and post natal care; to ensure that all birth attendants have the knowledge, skills and equipment to perform a clean and safe delivery and provide post partum care to the mother and baby, all women should have access to basic maternity care during delivery.
- Emergency obstetric care; to ensure that essential care for high risk pregnancies and complications is made available to all women and girls who need it. It is estimated that about 15 % of all normal pregnancies end up with complications therefore the need to always be prepared for emergency obstetric care.
- Basic maternity care
- Primary health care
- Equity for women
Components of safe motherhood
- Per-conception care
- Antenatal care
- Post partum care
- Post abortion care
- Emergency obstetric care
- Care of the newborn
Requirements for safe motherhood
- Achieving safe motherhood and reducing maternal mortality requires a 3 way strong strategy:
- All women have access to contraception to avoid unintended pregnancies.
- All pregnant women have access to skilled care at the time of birth.
- All women with complications have timely access to quality emergency obstetric care.
Maternal Mortality
- This is the death of a woman/mother while pregnant or within 42 days of the termination of pregnancy irrespective of the duration and the sites of pregnancy from any cause related to or aggravated by the pregnancy or its management BUT not from accidental or incidental causes.
- Maternal mortality rate
- This is the ratio of the total number of maternal deaths occurring in a period of time (usually a year) to the total number of live births occurring in the same period expressed as a percentage (or per 1,000 or 100,000).
- Assignment
- Look at the incidence and prevalence of maternal mortality in the world, Africa and Uganda
Factors contributing to the high maternal mortality in Uganda
- Poverty
- Gender issue
- Inadequate and inaccessible health services
- Limited health workers
- Poor attitudes of health workers towards mothers.
- Early marriages
- Illiteracy
- Beliefs, customs and taboos(harmful traditional practices)
- Poor transport and communication infrastructures
- High child mortality
- Desire for more children
- Sex preferences in children
- High fertility rate
- Underutilization of the existing services
- Inadequate drug supplies and other medical related equipment are most often interrelated are responsible for increased number of avoidable deaths.
- Poor attitudes by the health workers
- Non involvement of the husbands
- Lack of awareness/ignorance
- Disrespect for human rights
- Gender stereotypes and inequalities
- Poor referral systems for handling emergency
Delays that can lead to maternal mortality
- Delays at the individual woman’s levels
- Inability to make decision on life threatening health conditions in time for appropriate response
- Delay at the level of the family and community levels in decision making to assist the woman /husband’s issues/ in laws’ issues.
- Delay at the level of accessing services. Usually transport is a major problem and or lack of resources.
- Delay in the health units to institute the necessary interventions.
- Inadequate skills
- Failure to make appropriate decision ØLack of drug supplies etc.
Note: Not only mothers die, babies too die. 4000,000 new born deaths occur globally yet almost all are due to preventable conditions.
- Causes of maternal mortality There are several causes of maternal mortality broadly grouped into direct and indirect causes.
- A direct death is one resulting from obstetric complications of pregnancy, delivery or from interventions, omissions or incorrect treatment or a chain of events resulting from the above.
- An indirect death is one resulting from a previously existing diseases (present before) or developed during pregnancy and was not due to obstetric causes but aggravated by the physiological effects of pregnancy.
Direct Causes of Maternal Mortality
- i) Sepsis
- ii) Hemorrhage
- iii) Early pregnancy deaths
- iv) Hypertensive conditions
- v) Others
- Thrombosis and thrombo-embolism
- ØGenital trauma
Indirect causes of maternal mortality
- i) Cardiovascular diseases
- Pulmonary hypertension
- Endocarditis
- ii) HIV/AIDs
- iii) Malnutrition
- iv) Diabetes
- v) Thyroid diseases
- Vi) Anemia
Prevention of maternal mortality
- Eighty percent (80%) of these deaths can be prevented through actions that are effective and available in developing country’s settings. This is a coordinated long term effort within the families, countries and health systems, national legislation and policy.
- Primary prevention
- Girl child education
- Education keeps girl at school until when they are old enough to marry and have children.
- Proper nutrition of the girl child
- Malnutrition during childhood and puberty has been closely related to the inadequate development of the pelvis (contracted).
- Family planning: complications are as a result of unwanted pregnancies
- Quality antenatal care
- All pregnant women should be encouraged to have timely attendance of at least 4 quality antenatal visits, to assess for possible risks
- Immunization
- All women in the reproductive age should be immunized against tetanus, HEP-B because they are at a higher risk of developing the infections
Secondary prevention
- A skilled attendant should be present at every birth. Functional referral systems is very essential here
- Emergency obstetric care services is to be provided and made accessible to the people
- Transport and communication networks need to be improved to gain access to all health facilities. Transport means like ambulances
- Health facilities should be equipped with adequate equipments, operating theatres which should be functional, blood storage facilities in case of any emergency, equipments in good working conditions and drugs. The government should always ensure a steady supply of essential drugs.
- Adequate referral systems for complications should be instituted.
- Proper evaluation and reporting of maternal deaths and timely intervention taken
- Decentralization of services to make them available to all women
- Barriers to the access to health care facilities should be removed; policies should increase women’s decision making power as regards to their own health and reproduction.
- Recruitment of skilled staffs to balance of the workload
- Improving the standard and quality of care by organizing refresher courses for the health care personnel.
Tertiary prevention
This involves the control and management of complications that may arise ØEmergency obstetric care services should be provided.
Maternal Morbidity
- Definitions
- Obstetric morbidity originates from any cause related to pregnancy or its management any time during ante partum, intra-partum and post partum period usually up to 42 days ( weeks) after confinement.
- 1 Parameters of Maternal Morbidity
- Fever more than 38 degree centigrade
- Blood pressure greater than 140/90mmHg
- Recurrent vaginal bleeding
- Hemoglobin level less than 10.5gdl irrespective of gestational age
- Asymptomatic bacteriuria of pregnancy
i) Direct obstetric morbidity
Temporary (mild)
- APH, PPH, eclampsia, obstructed labor
- Rupture uterus
- Sepsis Ø Ectopic pregnancy
- Molar pregnancy etc.
Permanent (chronic)
- Vesico-vaginal fistula and rectovaginal fistula
- Dysparuria (persistent genital pain that occur before during and after intercourse)
- Prolaps
- Secondary infertility
- Obstetric palsy (paralysis that affect upper limb of the newborn due to brachial plexus injury in normal delivery associated with shoulder dystocia)
Indirect
- These conditions are only expression of aggravated previous existing diseases like malaria, hepatitis, tuberculosis, anemia etc. by changes in the various systems during pregnancy.
Perinatal Mortality
- This is defined as deaths among fetuses weighing 1000g or more at birth (greater than 28 weeks gestation) that die before or during delivery or within the first 7 days of delivery.
- The Perinatal mortality rate closely reflects both the standards of medical care and effectiveness of public and social health measures.
Incidence
- Worldwide nearly 4 million newborns die within the first week of life and another 3 million are born dead.
- Perinatal deaths could be reduced by at least 50% worldwide if key interventions are applied for the newborn.
- Perinatal mortality is less than 10 per 1000 total births in the developed countries while in the developing it is much higher.
Predisposing factors to perinatal mortality
- Many factors influence the perinatal mortality in Uganda and theses are briefly discussed below;
Maternal factors
- Age over 35 years
- Teenage pregnancies
- Multiparty
- Low social economic condition(poverty)
- Poor maternal nutritional status
NB. All the above adversely affect the pregnancy outcome
Medical disorders
- Anemia (Hemoglobin level less than 8g/dl)
- Hypertensive disorders
- Syphilis
- Diabetic mellitus
- Prematurity
- Congenital malformation (baby)
- Malaria
- Other infections
Obstetric complications
- Ante partum hemorrhage (APH) particularly abruptio placentae is responsible for about 10% of Perinatal death due to severe hypoxia
- Pre-eclampsia, eclampsia is associated with high Perinatal loss either due to placental insufficiency or prematurity
- Rhesus iso immunization
- Cervical incompetence
Complications of Labor
- Dystocia from disproportion, mal-presentation and abnormal uterine action
- Premature rupture of membranes (PROM) may result in hypoxia, amionitis and birth injuries contributing to Perinatal death
Fetal-placental factors (causes)
- Multiple pregnancy, most often leads to preterm delivery and usual complications
- Congenital malformation and chromosomal abnormalities are responsible for 15% of Perinatal death
- Intrauterine growth restriction and low birth weight babies
- Unexplained causes
- About 20% of still births have no obvious fetal, placental, maternal or obstetric causes.
Causes of Perinatal mortality
- Infection
- Sepsis
- Meningitis
- Pneumonia
- Neonatal tetanus, congenital
- Birth asphyxia and trauma
- Hypothermia
- Prematurity and/ low birth weight
- Congenital malformation
Control and prevention of perinatal mortality
- Pre pregnancy health care and counseling
- Genetic counseling in high risk cases and prenatal diagnosis to detect genetic, chromosomal or structural abnormalities are essential
- Regular antenatal care with advice regarding health, diet and rest
- Detection and early management of medical disorders in pregnancy such as anemia, diabetes, hypertension
- Screening of high risk clients where mandatory hospital delivery is instituted like those from poor social economic status, high parity, extreme of age etc.
- Careful monitoring and management of Labour to detect hypoxia, early evidence of traumatic vaginal delivery etc.
- Skilled birth attendance to minimize sepsis
- Provision of neonatal referral services especially to look after the preterm babies
- Health education of the mothers about the care of a new born such as early exclusive breastfeeding and prevention of hypothermia
- Educating the community to utilize family planning services and also to utilize the available maternity and child health care services
- Increased resource allocation towards maternal and child health services
- Regular review of perinatal death cases and ensuring effective supervision, monitoring and evaluation to realize the missing gaps
- Improving on social infrastructures like health care, transport and communication network
- Continuous decentralization of maternal and child health care services
PRE-CONCEPTION CARE
By the end of the session, learners should be able to:
- Explain the meaning of: Pre-conception care
- Discuss the purposes of pre-conception care
- Mention where pre- conception care can be provided
- Outline services offered during conception care
- Discuss how to reach out to special groups
Introduction
- Definition
- Preconception care;- is the provision of biomedical, behavioural and social health interventions to women and couples before conception occurs, aimed at improving their health status, and reducing behaviours and individual and environmental factors that could contribute to poor maternal and child health outcomes.
- Its ultimate aim is improved maternal and child health outcomes, in both the short and long term.
Introduction
- Note to be confused with;
- Periconception care; – provision of preventive, promotive or curative health and social interventions in the period extending from 3 months before to 3 months after conception occurs;
- Interconception care; – provision of preventive, promotive or curative health and social interventions between two pregnancies.
Aims of preconception care
- To improve maternal and child health both in short and long term; through reducing behaviors and individual and environmental factors that contribute to poor maternal and child health outcomes.
- To provide opportunities for prevention and control of diseases; through promotion of good life style behaviors.
- To secure optimal health & nutritional condition in both parents not only improving the chances of conception but also reducing possibility of parental death & many congenital anomalies.
- To ensure that women and their partners are in optimal state of physical and emotional health at onset of pregnancy.
- To promote prenatal health.
Purpose of preconception care
- To establish lifestyle behaviors to maintain optimum health
- To identify and treat risk (e.g. medical condition, substance abuse) before
- To enable conception of a pregnancy without necessary risk factors
- To prepare people psychologically for pregnancy and the responsibilities of parenthood
Why preconception care?
- Preconception care has a range of positive effect on a range of health outcome. Among others it can;
- Reduce maternal and child mortality
- Prevent unwanted pregnancies
- Prevent complications during pregnancy and delivery
- Prevent still births, preterm births and low birth weights
- Prevent birth defects
- Prevent neonatal infections
- Prevent underweight and stunting
- Prevent vertical transmission of HIV/STIs
- Lower the risk of some forms of childhood cancers
- Lower the risk of type diabetes and cardiovascular diseases later in life.
Areas addressed by the preconception care package.
- Nutritional deficiencies and disorders oVaccine-preventable infections oTobacco use oEnvironmental risks oGenetic disorders
- Early pregnancies, unwanted pregnancies, and pregnancies in rapid
- succession
- Sexually transmitted infections (STIs), including human
- immunodeficiency virus (HIV)
- Infertility and subfertility oFemale genital mutilation
- Mental health disorders, including epilepsy oPsychoactive substance use oIntimate partner and sexual violence
Components of preconception care
Nutritional conditions
- Screening for anaemia and diabetes
- Supplementing iron and folic acid
- Information, education and counselling
- Monitoring nutritional status
- Supplementing energy and nutrient-defense foods.
- Management of DM including counselling of people with DM.
- Promotion of exercise
- Iodization of salt
Tobacco use
- Screening of women and girls for tobacco use at all clinical visits using the 5As; (ask, advise, assess, assist, arrange).
- Providing brief tobacco cessation advise, pharmacotherapy (including nicotine replacement) and intensive behavioral counselling services.
- Screening of all non-smokers and advising them about the harm of second-hand smoke, its harmful effects on pregnant woman and the unborn children.
Genetic conditions
- Taking a thorough family history to identify risk factors for genetic conditions
- Family planning
- Genetic counselling
- Carrier screening and testing
- Appropriate treatment of genetic conditions
- Community-wise or national screening among populations at high risk.
Environmental health
- Providing guidance and information on environmental hazards and prevention
- Protecting from unnecessary radiation exposure in occupational, environmental and medical settings.
- Avoiding unnecessary pesticide use.
- Protecting from lead exposure
- Informing women of child bearing age about levels of methyl mercury in fish
- Promoting use of improved stoves and cleaner liquids/gaseous fuel.
Infertility/subfertility
- Creating awareness and understanding of fertility and infertility and their preventable and unpreventable causes.
- Defusing stigmatization of infertility and assumption of fate
- Screening and diagnosis of couples after 6-2 months of attempting pregnancy and management of underlying causes of infertility/sub-fertility including past STI
- Counselling of individuals/couples diagnosed with unpreventable causes of infertility/sub-fertility.
Potential benefits preconception care
- In the short term;
- preconception care could reduce pregnancies that are too early, too close, and unplanned.
- Preconception care could contribute to reducing the risk of genetic disorders and environmental exposure, to reducing maternal and childhood mortality, and to improving maternal and child health outcomes.qIt could also contribute to improving the health and well-being of women in other areas of public health, such as nutrition, infertility and subfertility, mental health, intimate partner and sexual violence, and substance use.
- In the long term;
- Preconception care could contribute to improving the health of babies and children as they grow into adolescence and adulthood.
- By supporting women to make well-informed and well-considered decisions about their fertility and their health, preconception care could contribute to the social and economic development of families and communities.
- By creating awareness of the importance of men’s health and men’s behaviours on maternal and child health outcomes, and by promoting male involvement, preconception care could result in additional benefits.
- From the programmatic perspective, preconception care provides a window to include interventions that have not traditionally been included in maternal, newborn and child health programmes, such as reduction in use of and exposure to tobacco
Related Topics
- Reproductive Health
- Pillars of Safe Motherhood
- Methods of Family Planning
- Management of STI’s/HIV/AIDS
- Adolescent Health and Development
- Adolescent and Reproductive Health
- Adolescent Friendly Health Services
- Post Abortion Care
- Signs and Symptoms of Pregnancy
- Signs and Symptoms of Labor
- Management of 2nd Stage of Labor
- Management of 3rd Stage of Labor
- Care of a Baby’s Cord
- Health Education of Mothers
- Referral System for Mother
- Signs and symptoms of 3rd stage of labor
- Examination of placenta
- Identification of mothers at risk and their referral
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

