Reproductive Health
Subtopic:
Post Abortion Care

Post-abortion care (PAC) is a multifaceted approach designed to minimize injuries and fatalities resulting from incomplete or unsafe abortions, as well as any complications that may arise from such procedures. It forms a vital part of comprehensive abortion services and encompasses five key elements.
Components of PAC
Emergency Treatment of Incomplete Abortion and Life-Threatening Complications:
Providing immediate medical attention for incomplete abortions and any related life-threatening complications.
Performing uterine evacuation to prevent further health risks to the patient.
Post-Abortion Counseling:
Offering psychological support to help women process and overcome any trauma experienced.
Educating patients on how to recognize and respond to potential post-abortion complications, such as fever, severe hemorrhage, and acute lower abdominal pain.
Providing clear instructions on when to seek medical attention if complications arise.
Initiation of Post-Abortal Family Planning Counseling and Services:
Educating women about the rapid return to fertility following an abortion (typically within about 10 days).
Offering information on various family planning methods available.
Supporting the patient in choosing a suitable contraceptive method and providing access to it in order to prevent future unintended pregnancies.
Integration with the Reproductive Health Care System:
Ensuring that post-abortion emergency services are a seamless part of the broader reproductive health care services.
Providing access to comprehensive reproductive health services including STI/HIV screening and cervical cancer prevention.
Community Participation in Complication Prevention:
Educating community members on the dangers and signs of abortion complications, which can include:
Bleeding
Foul-smelling discharge
Abdominal pain
Fever
Promoting measures to prevent complications through:
Personal hygiene practices
Treatment of Sexually Transmitted Infections (STIs)
Consistent use of post-abortion family planning methods
Importance of Post-Abortion Care
Life-Saving Services: PAC significantly reduces the risk of maternal mortality and morbidity linked to unsafe abortions.
Reduces Fertility Problems: PAC helps to prevent long-term reproductive health issues that can result from unsafe abortions.
Prevents Unwanted Pregnancies: Provides effective family planning and contraceptive services to prevent future unintended pregnancies.
Accessible Quality Health Services: Ensures women can access necessary and appropriate health care services.
Improves Overall Health: Supports the physical, social, spiritual, and psychological well-being of women.
Better Referral Management: Streamlines the process for accessing more advanced medical care when needed.
Encourages Proactive Health-Seeking Behavior: Empowers women to promptly seek medical assistance when necessary.
Comprehensive Abortion Care
Comprehensive abortion care involves the primary, secondary, and tertiary prevention of unsafe abortions and integrates abortion care with other reproductive health services. The overall aim is to minimize and prevent negative outcomes associated with abortion.
Components of Comprehensive Abortion Care:
Prevention of Unintended Pregnancies:
Providing comprehensive sexuality education.
Promoting safe sex practices.
Ensuring access to contraception and family planning services.
Providing access to emergency contraception.
Involving the community in reproductive health education and support.
Provision of Abortion Services to the Full Extent of the Law:
Offering legally sanctioned and safe abortion procedures.
Providing access to both medical and surgical abortion options.
Post-Abortion Care (PAC), which includes five elements:
Emergency treatment of abortion complications, including uterine evacuation for incomplete abortions.
Providing post-abortion and family planning counseling.
Providing various family planning methods.
Linking abortion care services with other reproductive health services, such as STI/HIV prevention and cervical cancer screening.
Ensuring community involvement in support and prevention efforts.
Management of Abortion
(Note: More detailed management information can be found in Gynecology resources.)
Triage for Abortion Patients:
Monitor vital signs such as blood pressure and pulse.
Assess for signs of shock, severe pain, altered consciousness, general condition, vaginal bleeding, and fever.
Resuscitate as needed before taking a detailed history.
Specific Types of Abortion and Their Management:
Threatened Abortion:
Admit the patient to the maternity ward for close monitoring.
Administer medications such as ferrous sulfate, nifedipine, and an antispasmodic if needed.
Advise the patient to rest in bed and avoid strenuous activities.
Follow up in the antenatal clinic if bleeding stops; reassess if bleeding persists.
Inevitable Abortion:
Hospitalization and medical management.
Perform Manual Vacuum Aspiration (MVA) for pregnancies less than 16 weeks; administer oxytocin or misoprostol for pregnancies beyond 16 weeks.
Schedule a follow-up appointment and offer post-abortion care (PAC).
Incomplete Abortion:
Hospitalization and surgical management.
Use forceps for cases with minimal bleeding or MVA for cases with more profuse bleeding.
Administer oxytocin or misoprostol for pregnancies beyond 16 weeks.
Provide post-abortion care (PAC) before discharge.
Complete Abortion:
Usually, no need for uterine evacuation is required
Monitor the patient for bleeding, and provide post-abortion care (PAC).
Administer antibiotics before discharge.
Complications of Abortion
Acute Complications:
Incomplete abortion
Sepsis (systemic infection)
Hemorrhage (excessive bleeding)
Uterine perforation (puncture of the uterus)
Bowel injury
Long-Term Complications:
Chronic pelvic pain
Pelvic inflammatory disease (PID)
Tubal blockage and secondary infertility
Ectopic pregnancy (pregnancy outside the uterus)
Increased risk of spontaneous abortion or premature delivery in future pregnancies.
Barriers to PAC
Several factors can hinder the effective delivery of post-abortion care (PAC):
Knowledge Gap Among Health Workers: Insufficient training and understanding of PAC protocols among healthcare providers.
Inadequate Infrastructure and Facilities: Lack of suitable facilities and resources to provide comprehensive PAC services.
Insufficient Supportive Laws and Policies: Absence or inadequacy of legal frameworks and policies that support women’s access to PAC.
Long Distances to Health Facilities: Geographical barriers that limit access to PAC services, especially in rural areas.
Lack of Necessary Equipment: Shortages of essential medical equipment and supplies needed to provide effective PAC.
Mandatory Waiting Periods: Imposed delays before accessing care, which can cause unnecessary suffering and risk.
High Costs of Care: Financial burdens that prevent women from seeking and receiving needed PAC services.
Social Stigma: Negative societal attitudes and judgments surrounding abortion, leading to avoidance of care.
Health Workers’ Refusal Based on Personal Beliefs: Healthcare providers declining to provide PAC due to their personal moral or religious convictions.
Prevention of abortion
Prevention of abortion is achieved through a multi-tiered approach:
Primary Prevention: Focuses on preventing unintended pregnancies through education, access to contraception, and family planning services.
Secondary Prevention: Aims to prevent unsafe abortions by ensuring access to safe and legal abortion services when needed.
Tertiary Prevention: Involves managing post-abortion complications effectively and preventing future unsafe abortions through comprehensive PAC.
Strategies for Prevention:
Counseling and Universal Access to Family Planning: Providing accessible and comprehensive counseling and family planning services to prevent unintended pregnancies.
Increase Availability of Safe Abortion Services: Expanding access to safe and legal abortion services, in accordance with legal frameworks.
Improve Quality and Accessibility of PAC: Ensuring that PAC is readily available and of high quality to prevent complications from unsafe abortions.
Educate Communities: Educating communities about reproductive health, the dangers of unsafe abortion, and available services.
Advocate for Policy Changes: Promoting policy changes that protect women’s reproductive health and rights.
Promote Gender Equality and Decision-Making: Empowering women through promoting gender equality and giving them decision-making power over their reproductive health.
Support Education for Girls and Employment for Women: Enabling girls and women through access to education and economic opportunities.
Encourage Attendance at Antenatal Service Centers: Promoting early and regular antenatal care to ensure healthy pregnancies and deliveries.
Provide Social Protection: Supporting abandoned women with the social protection measures to reduce their vulnerability.
Offer Non-Judgmental Counseling: Providing supportive and non-judgmental counseling services to women facing unplanned pregnancies.
Ensure Access to Emergency Contraceptives: Making emergency contraception readily available to prevent unintended pregnancies after unprotected intercourse.
Detailed Post-Abortion Care (PAC)
Post-abortion care encompasses several critical elements to safeguard the health and well-being of women who have undergone an abortion:
Emergency Treatment of Abortion Complications:
Aspiration and Evacuation: For incomplete abortions, the uterus must be evacuated. The method of evacuation depends on the gestational age of the pregnancy:
For pregnancies below 12 weeks, Manual Vacuum Aspiration (MVA) is the preferred method.
For pregnancies below 9 weeks, Misoprostol can be used to terminate first-trimester intrauterine pregnancies. A standard dose of 800 micrograms can be administered orally, sublingually, or vaginally.
Intravenous Fluids and Resuscitation: In cases of shock, immediately administer intravenous normal saline (1 liter in 15-20 minutes). Plasma expanders may also be used if available.
Blood Transfusion: If blood transfusion is needed, carefully monitor the amount of blood transfused and the patient’s response to treatment.
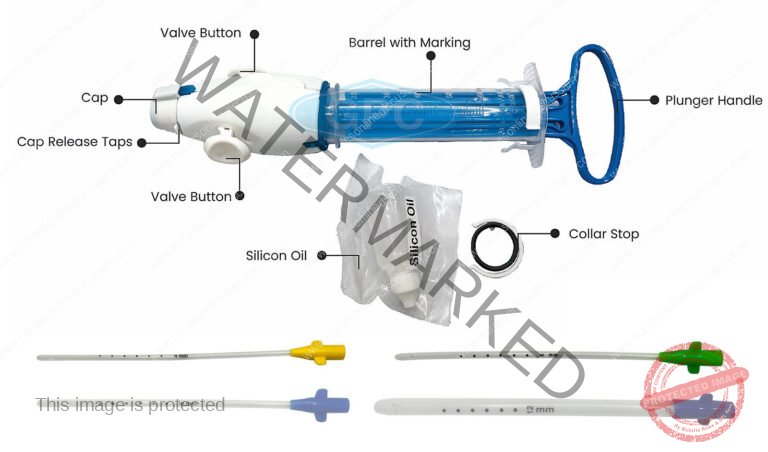
Manual Vacuum Aspiration (MVA)
Manual Vacuum Aspiration (MVA) is a method of pregnancy termination where a healthcare provider uses a handheld device (an aspirator) to gently remove the contents of the uterus using suction. The procedure is typically performed while the patient is awake. A narrow tube (cannula) attached to a syringe is used to empty the womb through aspiration, which is a process of gentle suction. Local anesthetic is injected into the cervix (neck of the womb) to minimize discomfort during the procedure.
MVA is a preferred, appropriate, and cost-effective method for managing abortion, particularly in resource-limited settings. It is highly effective up to 12 weeks of pregnancy and has demonstrated high efficacy in numerous randomized controlled trials. MVA has largely replaced dilation and curettage (D&C) in many industrialized and developing countries.
Preparation:
Ensure the patient is prepared, the room is set up correctly, all equipment and supplies are readily available, and an assistant is present.
Select the appropriate size of the cannula based on the gestational age and size of the uterus.
Requirements for MVA Procedure:
Trolley (Top Shelf):
Sterile MVA set
Casco speculum
Vulsellum (or tenaculum)
Uterine sound
Receiver
Bowl of cotton swabs
Sponge-holding forceps
Appropriate-sized cannulas
Local anesthetic (Lidocaine or bupivacaine)
Syringe and needle
KY Jelly
Antiseptic solution
Trolley (Bottom Shelf):
Gumboots
Buckets
Screens
Apron
Bedside Setup:
Items for immediate use during the procedure.
Procedure for Manual Vacuum Aspiration:
Review Indications: Confirm appropriate indications such as:
Inevitable abortion before 16 weeks
Incomplete abortion
Molar pregnancy
Delayed postpartum hemorrhage due to retained placental fragments
Provide Emotional Support and Encouragement: Ensure the patient feels supported and reassured throughout the procedure.
Offer Pain Relief: Administer paracetamol 30 minutes before the procedure or perform a para-cervical block to numb the area.
Prepare the MVA Syringe:
Assemble the syringe, close the pinch valve, and pull back on the plunger until the plunger arms lock.
For molar pregnancy, have three syringes prepared. For very early pregnancy, insert the cannula without prior cervical dilation.
Administer Oxytocin or Ergometrine: Give oxytocin 10 units intramuscularly (IM) or ergometrine 0.2 mg IM to firm the uterine muscle and reduce the risk of perforation.
Perform a Bimanual Pelvic Examination: Re-assess the size and position of the uterus and the conditions of the fornices (the spaces around the cervix).
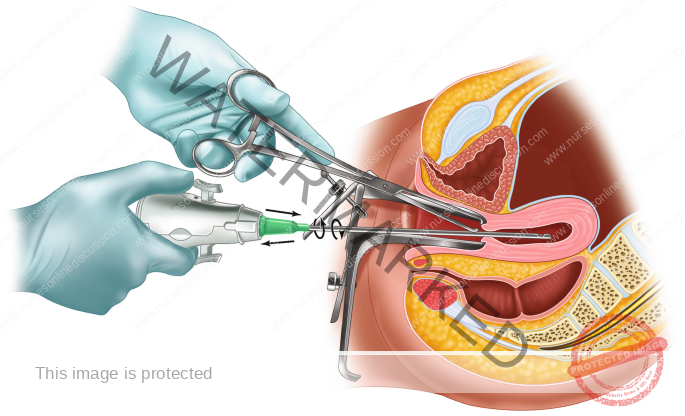
Insert Sterile Speculum and Visualize the Cervix: Apply antiseptic solution to the vagina and cervix, particularly around the os (the opening of the cervix).
Check the Cervix for Tears or Protruding POC: Remove any visible products of conception (POC) with ring (or sponge) forceps.
Gently Grasp the Anterior Lip of the Cervix: Use ring forceps or a single-toothed tenaculum. If using a tenaculum, first inject 1 mL of 0.5% lignocaine solution into the cervix to minimize pain.
Dilate the Cervix if Needed: For a missed abortion or prolonged retention of POC, use mechanical or osmotic dilators, or cervical priming with mifepristone or prostaglandin.
Insert the Cannula: While applying gentle traction to the cervix, carefully insert the cannula through the cervix into the uterine cavity, just past the internal os.
Attach the Prepared MVA Syringe: Hold the ring forceps (or tenaculum) and the end of the cannula in one hand and the syringe in the other. Release the pinch valve(s) to transfer the vacuum to the uterine cavity.
Evacuate Remaining Contents: Gently rotate the syringe from side to side and move the cannula back and forth within the uterine cavity to ensure complete evacuation without losing the vacuum.
Check for Signs of Completion: Look for signs such as:
Red or pink foam without tissue
A grating sensation as the cannula moves along the uterine wall
The uterus contracting around the cannula
Withdraw the Cannula: Detach the syringe, place the cannula in a decontamination solution, and empty the syringe contents into a strainer.
Perform a Bimanual Examination: Check the size and firmness of the uterus after the procedure.
Inspect the Tissue Removed: Ensure complete evacuation, assess for molar pregnancy, and if needed, strain and rinse the tissue for examination.
Address Absence of POC: If no products of conception are seen, consider a complete abortion, breakthrough bleeding, or a possible ectopic pregnancy.
Reinsert Speculum and Examine for Bleeding: If there is persistent bleeding or the uterus feels soft, repeat the evacuation procedure.
Post-Procedure Care:
Administer paracetamol 500 mg as needed for pain relief.
Consider antibiotics to prevent infection.
Encourage the patient to eat, drink, and walk.
Offer other necessary health services.
Discharge Uncomplicated Cases:
Discharge the patient within 1-2 hours if the case is uncomplicated.
Provide clear instructions on symptoms that require immediate medical attention.
Precautions for Performing MVA:
Delay the procedure if conditions such as shock, severe vaginal bleeding, or intra-abdominal injury are present. Stabilize the patient first.
Stabilization involves providing oxygen, intravenous fluids, antibiotics for sepsis, and blood transfusion if needed.
Shock Management:
Recognize symptoms such as:
Rapid, weak pulse
Low blood pressure
Pallor
Sweatiness
Rapid breathing
Anxiousness, confusion, or unconsciousness
Treat with oxygen, intravenous fluids, antibiotics, and blood transfusion if necessary.
Severe Vaginal Bleeding:
Identify symptoms such as:
Heavy, bright red bleeding
Pallor
Blood-soaked materials
Assess all sources of bleeding, stabilize the patient, and evacuate POC.
Intra-Abdominal Injury:
Recognize symptoms such as:
Distended abdomen
Decreased bowel sounds
Rigid abdomen
Rebound tenderness
Nausea and vomiting
Pain, fever, or cramping
Immediate management involves intravenous fluids, antibiotics, and potential surgery. Perform MVA after stabilization.
Related Topics
- Reproductive Health
- Pillars of Safe Motherhood
- Methods of Family Planning
- Management of STI’s/HIV/AIDS
- Adolescent Health and Development
- Adolescent and Reproductive Health
- Adolescent Friendly Health Services
- Post Abortion Care
- Signs and Symptoms of Pregnancy
- Signs and Symptoms of Labor
- Management of 2nd Stage of Labor
- Management of 3rd Stage of Labor
- Care of a Baby’s Cord
- Health Education of Mothers
- Referral System for Mother
- Signs and symptoms of 3rd stage of labor
- Examination of placenta
- Identification of mothers at risk and their referral
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

