Specialized Nursing Care Procedure
Subtopic:
Lumbar Puncture
Learning Objectives
Identify the key indications for performing a lumbar puncture, including diagnostic and therapeutic uses.
Recognize contraindications and patient risk factors to ensure safe procedure execution.
Describe the equipment setup and preparation steps for a sterile lumbar puncture.
Explain the nursing roles before, during, and after the procedure, including patient education and monitoring.
Understand normal cerebrospinal fluid (CSF) parameters and their diagnostic relevance.
List common complications of lumbar puncture and strategies to prevent or manage them.
A lumbar puncture
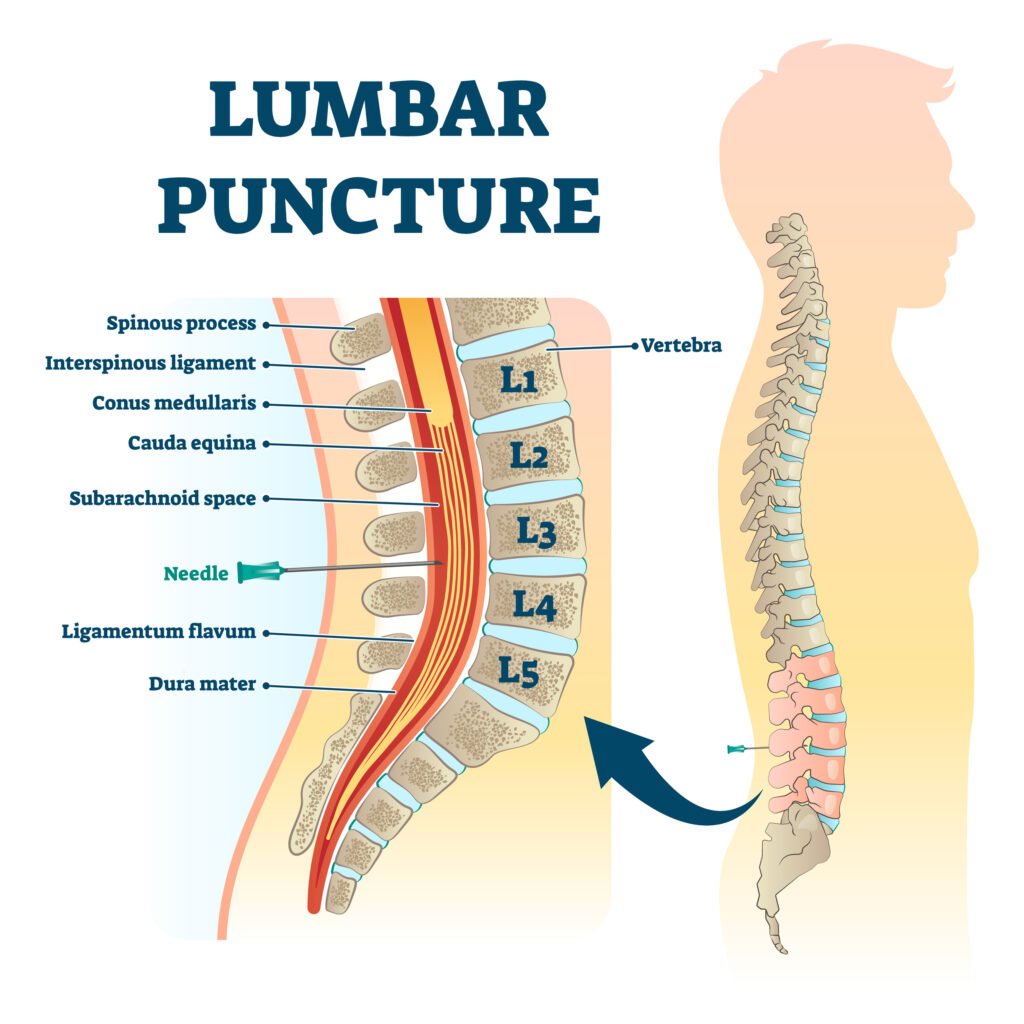
A lumbar puncture (also known as a spinal tap) is a medical procedure that involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF). This is done by inserting a special needle into the subarachnoid space – the space between the spinal cord and its protective covering (the meninges) – typically between the third and fourth or fourth and fifth lumbar vertebrae. This location is chosen because the spinal cord ends higher up, minimizing the risk of damaging it with the needle.
CSF is the fluid that surrounds the brain and spinal cord.
Indications for Lumbar Puncture
A lumbar puncture may be performed for several reasons, including:

CSF Pressure Measurement: To measure the pressure of the cerebrospinal fluid (CSF), which can be elevated in conditions like idiopathic intracranial hypertension or meningitis.
Diagnosis of CNS Infections: To aid in the diagnosis of infections affecting the central nervous system (CNS), such as:
Bacterial or Viral Meningitis: Inflammation of the membranes surrounding the brain and spinal cord.
Meningoencephalitis: Inflammation of both the brain and the meninges.
Diagnosis of Bleeding: To detect bleeding within the skull, such as:
Intracranial Hemorrhage: Bleeding within the brain tissue.
Subarachnoid Hemorrhage: Bleeding in the space between the brain and the meninges.
Diagnosis of Certain Cancers: To identify some malignant disorders that may affect the CNS.
Evaluation of Demyelinating and Inflammatory CNS Diseases: To assist in diagnosing conditions like:
Multiple Sclerosis (MS): An autoimmune disease affecting the CNS, where CSF analysis may reveal oligoclonal bands.
Guillain-Barré Syndrome (GBS): An autoimmune disorder affecting the peripheral nervous system, often showing elevated protein in the CSF.
Acute Disseminated Encephalomyelitis (ADEM): A rare inflammatory disease of the brain and spinal cord.
Administration of Medications: To deliver medications directly into the CSF, such as:
Spinal Anesthesia: To numb the nerves in the spinal canal for surgical procedures.
Chemotherapy: To treat certain cancers affecting the CNS.
Radiological contrast procedures To administer contrast agents into the CSF for imaging studies, such as:
Myelography: To visualize the spinal canal and nerve roots.
Cisternography: To evaluate CSF flow.
Other Therapeutic Uses:
Normal Pressure Hydrocephalus: To treat the accumulation of excess CSF in the brain.
Cerebrospinal Fistulas: To help manage abnormal connections between the CSF space and other areas.
Idiopathic Intracranial Hypertension (IIH): To treat increased intracranial pressure of unknown cause.
Placement of a Lumbar CSF Drainage Catheter: To drain excess CSF.
Contraindications for Lumbar Puncture
A lumbar puncture may be contraindicated (should not be performed) in the following situations:
Suspected Space-Occupying Lesion: If there is suspicion of a brain tumor, abscess, or other space-occupying lesion causing increased intracranial pressure, a CT scan or MRI should be performed before considering a lumbar puncture. This is because removing CSF in such cases could lead to brain herniation (shifting of brain tissue), a life-threatening complication.
Severe Bleeding Disorders (Coagulopathy): Patients with severe bleeding disorders or those taking blood thinners are at increased risk of bleeding complications, such as an epidural hematoma (a collection of blood around the spinal cord).
Severe Degenerative Joint Disease of the Spine: Conditions like spinal stenosis, which involves narrowing of the spinal canal, can make it technically difficult to insert the needle.
Severe Spinal Deformities: Conditions like severe scoliosis can increase the risk of complications during the procedure.
Skin Infection at the Puncture Site: An infection near the puncture site increases the risk of introducing bacteria into the CSF.
Patient Refusal: A lumbar puncture should not be performed if the patient refuses the procedure.
Equipment for Lumbar Puncture

Procedure for Lumbar Puncture
| Steps | Action | Rationale |
| 1. | Adhere to standard clinical protocols and guidelines. | To ensure best practice and patient safety. |
| 2. | Offer the patient a bedpan or urinal before the procedure begins. | To enhance patient comfort during the procedure. |
| 3. | Position the patient appropriately, choosing from: i) Sitting upright on a stool, bending forward with head lowered towards knees; ii) Lying on their side (lateral decubitus) near the bed edge, knees and hips maximally flexed and drawn up towards the chest, with a pillow supporting the head and a firm surface beneath if required. | A flexed posture widens the spaces between vertebrae, facilitating needle insertion. A firm surface stabilizes the patient. |
| 4. | Encourage the patient to maintain the flexed position and remain still throughout the procedure. | To minimize movement and potential trauma during needle insertion. |
| 5. | Ensure patient is appropriately covered, exposing only the lumbar region for the procedure. | To maintain patient dignity and privacy. |
| 6. | Provide focused and adequate lighting onto the lumbar area. | To ensure clear visualization of the puncture site. |
| 7. | Organize and prepare the sterile equipment from the top shelf of the trolley for immediate use. | To facilitate efficient workflow and access to necessary sterile supplies. |
| 8. | Pour antiseptic solution into a gallipot. The clinician will cleanse the intended puncture site thoroughly using aseptic technique and drape the area with sterile drapes. | For infection prevention and to maintain a sterile field during the procedure. |
| 9. | Perform hand hygiene, dry hands thoroughly, and put on sterile gloves. | To maintain sterility and prevent infection. |
| 10. | Assist the clinician as needed during skin preparation, administration of local anesthetic, and performance of the lumbar puncture, typically between the L3/L4 or L4/L5 intervertebral spaces. | To support the clinician in performing the procedure safely and accurately, minimizing risk to the spinal cord. |
| 11. | Open specimen bottles and position them close to the needle insertion point, approximately 1cm below, to collect cerebrospinal fluid directly. | To minimize contamination risk during CSF collection. |
| 12. | Reassure the patient continuously and monitor their condition, including color, pulse, respiratory rate, and report any changes or concerns promptly. | To detect and manage potential complications swiftly. |
| 13. | Properly label all specimen containers and promptly send them to the laboratory along with the completed laboratory request form. | For accurate diagnosis and timely processing of specimens. |
| 14. | Assist the clinician in sealing the puncture site with tincture benzoin or collodion and applying a sterile dressing. | To prevent CSF leakage from the puncture site. |
| 15. | Instruct the patient to remain lying flat in bed, with minimal movement unless necessary, for a minimum of 12 hours post-procedure. | To minimize the risk of post-lumbar puncture headache and backache. |
| 16. | Dispose of used equipment appropriately according to healthcare waste management protocols. | To maintain ward cleanliness and prevent hazards. |
| 17. | Monitor the patient’s condition regularly (e.g., every 15 mins for the first hour, then half-hourly, hourly, and 4-hourly for 24 hours) depending on their stability and clinical status. | To promptly identify and manage any post-procedure complications. |
| 18. | Clear away the trolley and perform hand hygiene. | To prevent cross-infection. |
| 19. | Document the procedure details, patient response, and any complications in the patient’s medical record. | To ensure comprehensive patient record-keeping and facilitate follow-up care. |
Points to Remember:
A manometer should be readily available for the clinician to measure cerebrospinal fluid pressure if clinically indicated.
Meticulous aseptic technique is paramount throughout the entire lumbar puncture procedure to minimize infection risks.
Post-procedure, it is advisable to encourage the patient to lie flat in bed for the recommended duration to help prevent complications like headache.
Nursing Roles in Lumbar Puncture
Before the Procedure:
Patient Education: Explain the procedure to the patient, including its purpose, where it will be performed, and who will perform it.
Informed Consent: Ensure the patient understands the procedure and signs a consent form if required by the institution.
Dietary Instructions: Inform the patient that fasting is typically not required before a lumbar puncture.
Promote Comfort: Encourage the patient to empty their bladder and bowel before the procedure.
Baseline Assessment: Obtain baseline vital signs and perform a neurological assessment of the legs, including movement, strength, and sensation.
Positioning: Assist the patient into the correct position, typically either:
Lateral Decubitus (Fetal) Position: Lying on their side near the edge of the bed with knees drawn up to the chest and chin tucked to the chest.
Sitting Position: Sitting on the edge of the bed, leaning forward over a bedside table.
Immobility: Instruct the patient to remain completely still during the procedure to prevent injury.
During the Procedure:
Equipment Arrangement: Organize the necessary equipment for easy access by the physician.
Bed Protection: Place a waterproof pad (mackintosh) and a draw sheet on the bed to protect it.
Patient Positioning and Support: Help position the patient correctly and provide support to maintain the position throughout the procedure.
Provide a Stool: Ensure a stool is available for the physician to sit on.
Site Exposure: Expose the lumbar puncture site.
Patient Monitoring: Assist in monitoring the patient’s vital signs and overall condition.
Reassurance: Offer reassurance and encouragement to the patient to help them remain calm and still.
Hand the manometer to the doctor to measure CSF if needed.
After the Procedure:
Pressure on Puncture Site: Apply brief pressure to the puncture site to minimize bleeding and cover it with a small sterile dressing.
Bed Rest: Position the patient flat in bed, as per the physician’s order. Usually, patients are advised to stay flat for 4-6 hours. They may turn from side to side, but should not lift their head.
Monitoring: Monitor vital signs, neurological status, and intake and output every 4 hours for 24 hours.
Puncture Site Assessment: Regularly inspect the puncture site for signs of CSF leakage, bleeding, or infection. Observe for symptoms like positional headache, nausea, vomiting, neck stiffness, light sensitivity (photophobia), imbalance, ringing in the ears (tinnitus), and sensitivity to sound (phonophobia).
Hydration: Encourage increased fluid intake (up to 3,000 ml in 24 hours, if not contraindicated) to help replace the CSF that was removed.
Specimen Handling: Label and number the CSF specimen tubes correctly and send them to the laboratory immediately.
Pain Management: Administer analgesics as prescribed for post-lumbar puncture headache.
Normal Results of Lumbar Puncture
Pressure: 70-180 mm H2O
Appearance: Clear and colorless
Total Protein: 15-45 mg/dL
Gamma Globulin: 3-12% of total protein
Glucose: 50-80 mg/dL (or greater than 2/3 of blood glucose level)
Cell Count: 0-5 white blood cells (WBCs) per microliter (all mononuclear cells), no red blood cells (RBCs)
Chloride: 118-130 mEq/L
Complications of Lumbar Puncture
Lumbar puncture should be performed with strict aseptic technique and careful attention to detail to minimize complications. Potential complications include:
Post-Lumbar Puncture Headache: The most common complication, occurring in about 25% of patients, often due to CSF leakage from the puncture site.
Meningitis: Infection of the meninges (brain and spinal cord coverings).
Bleeding into the Spinal Canal: Can cause nerve damage or other neurological problems.
Sudden Death: A very rare but serious complication, sometimes associated with increased intracranial pressure.
Spinal Cord Compression: Pressure on the spinal cord.
Edema or Hematoma at Puncture Site: Swelling or a collection of blood at the puncture site.
CSF Leakage: Persistent leakage of CSF from the puncture site.
Reaction to Anesthetic: Adverse reaction to the local anesthetic used during the procedure.
Epidural or Subdural Abscess: Infection in the spaces around the spinal cord.
Difficulty Voiding: Temporary difficulty urinating after the procedure.
Brain Herniation: Shifting of brain tissue due to pressure changes, particularly if there is pre-existing increased intracranial pressure.
Local Pain: Pain at the puncture site due to nerve root irritation.
Prevention of Post-Lumbar Puncture Headache
Minimize Lighting: Keep the environment dimly lit to reduce visual stimulation.
Encourage Hydration: Promote adequate fluid intake to help restore CSF volume.
Analgesics: Administer prescribed pain relievers.
Positioning: Elevating the foot of the bed (Trendelenburg position) may help reduce CSF leakage and pressure on the puncture site, although this is less commonly used now. Current practice favors a period of lying flat.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Foundations of Nursing (III)
- Apply Nursing process to the management of patients
- Administer prescribed medicine appropriately
- Instilling medication (general)
- Blood transfusion
Specialized Nursing Care Procedures
- Perform Shortening and removal of drains
- Perform Colostomy Care
- Prepare Abdominis Paracentesis (Abdominal Tapping)
- Prepare Lumbar Puncture
- Perform Gastrostomy Feeding
- Carry out gastric Lavage
- Perform Tracheostomy Care
- Ophthalmological Care
- Care of the patient`s ears
- Pre-Operative Eye Care
- Ear Care
- Peri-Operative Care:
- Orthopedic Nursing Care
- Prepare for Neurological Assessment
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

