Communicable Diseases
YELLOW FEVER
Table of Contents

Learning Objectives
- Describe the etiology, epidemiology, and transmission cycles of the Yellow Fever virus.
- Identify the clinical signs and symptoms of both early and severe Yellow Fever infection.
- Explain the pathological effects of the virus on major organs like the liver and kidneys.
- Outline the diagnostic methods and supportive management strategies for a patient with Yellow Fever.
- List the primary measures for the prevention and control of Yellow Fever, including vaccination and vector control.
- Discuss the relevance of Yellow Fever to midwifery practice, particularly concerning pregnant women.
YELLOW FEVER
Yellow fever is a hemorrhagic fever of the tropics, caused by the yellow fever virus, a flavivirus.
- The Yellow fever virus is an arthropod-borne virus from the flavivirus genus of the family flaviviridae.
- It possesses a single stranded, positive polarity RNA genome.
- Viral particles are 43nm in size; they are made up of a ribonucleoprotein core and lipoprotein envelope.
- It is a zoonosis of monkeys in west and central Africa, south and central American tropical in forests where it may cause devastating epidemics.
Epidemiology
- Yellow fever is endemic in tropical Africa and South America.
- The disease is transmitted by mosquito vectors in jungle, savannah, and urban settings.
- Uganda experiences periodic outbreaks, particularly in forested and rural regions, due to favorable environmental conditions for mosquito breeding.
Modes of spread
- Infection is introduced to humans through infected mosquitoes or monkeys invading human settlements.
- There are two kinds of yellow fever:
- Urban yellow fever (from man to man).
- Jungle yellow fever (from infected mosquito to man).
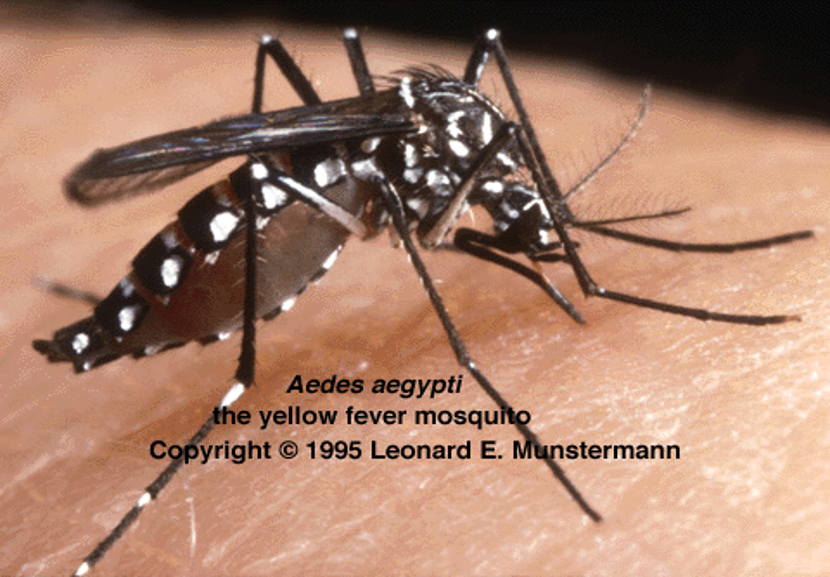
- Transmission occurs via the bite of infected Aedes aegypti and Haemagogus spp. mosquitoes.
- Transmission occurs in jungle (sylvatic), intermediate (savannah), and urban cycles. The virus is maintained in nature through these cycles.
VECTORS IN AFRICA
- Transmission is by tree top mosquitoes – Aedes africanus (Africa).
- Vectors include:
- Aedes africanus
- Aedes agypti
- Aedes simpsoni
- Aedes (Diceromyia) furcifer
Aedes aegypti
Aedes simpsoni

Aedes africanus

RISK FACTORS
- Living in or traveling to endemic regions (tropical Africa, South America).
- Lack of vaccination.
- Exposure to mosquito breeding areas (stagnant water, forests, urban slums).
- Occupation-related risks (forest workers, farmers, healthcare providers in endemic areas).
- Poor vector control measures (inadequate insecticide use, lack of bed nets).
- Climate change and deforestation increasing mosquito habitats.
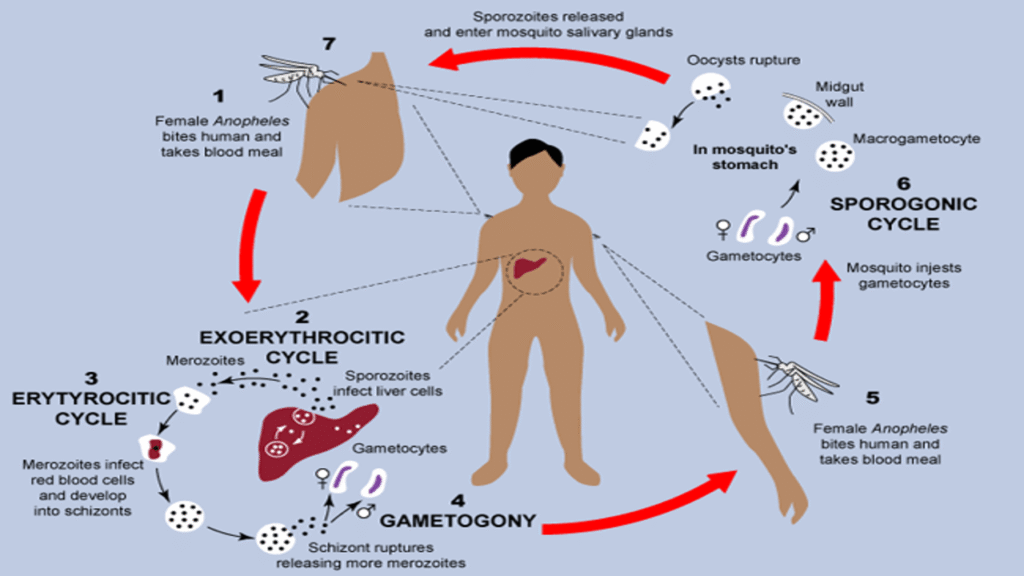
Lifecycle of the Yellow Fever Virus
- Mosquitoes acquire the virus when feeding on an infected primate or human.
- The virus replicates in the mosquito’s midgut and spreads to its salivary glands.
- When an infected mosquito bites a human, the virus is transmitted into the bloodstream.
- The virus incubates for 3–6 days before symptoms appear.
- The infection can either resolve or progress into the toxic phase, leading to severe complications like jaundice, bleeding, and organ failure.
PATHOLOGY
- After entry into the body through the sites of mosquito bite, the virus multiplies in lymph nodes and large organs such as liver, kidneys, heart, lungs, spleen, brain, and the digestive tract.
- The virus affects highly specialized epithelial or myocardial cells only. The changes range from cloudy swelling to generalized fatty changes, coagulation and necrosis of tissue cells.
- In the liver, epithelial cells in the liver lobes are destroyed.
- In the kidney, there is necrosis of the tubule of epithelium.
- In the GIT, there is hemorrhage due to damage of blood vessels.
- Death occurs from failure of liver or kidneys or both. The sino-arteriole nodes, bundles of His in the ileo-cardial cells may also be affected.
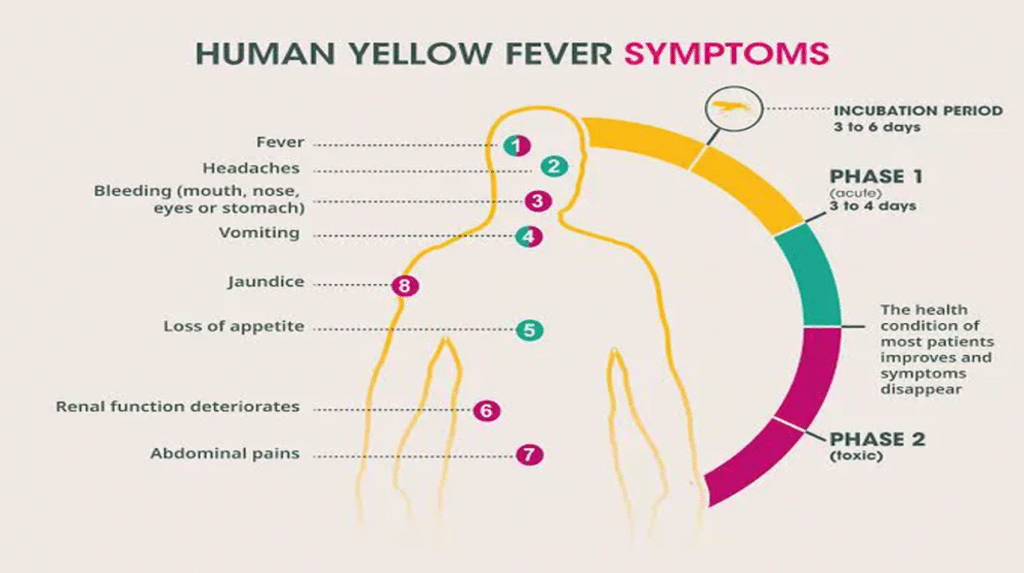
SIGNS AND SYMPTOMS
Yellow fever presents in stages:
Infection Stage (Early Symptoms)
- Sudden onset of fever.
- Chills, headache, back pain.
- Muscle pain, nausea, and vomiting.
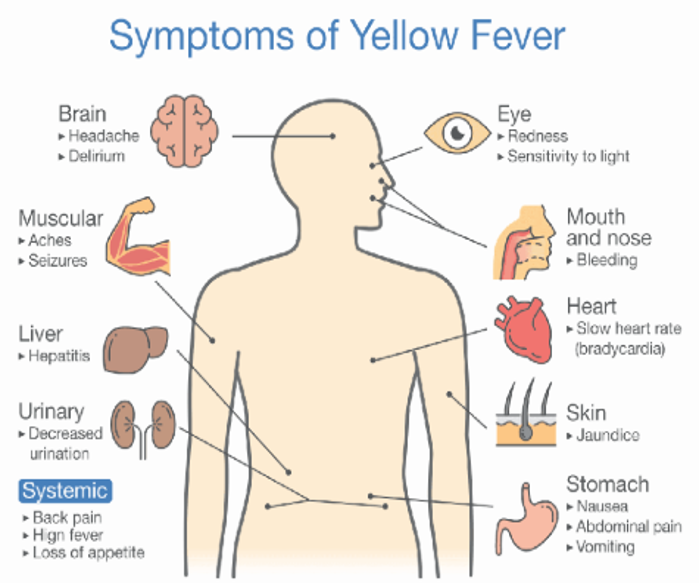
SEVERE INFECTIONS
- There may be a short period of recovery. Later, fever returns and the patient’s condition detoriates rapidly with development of liver and kidney failure.
- Sudden onset of fever of 40°C and chills.
- Severe headache and backaches without loins and limb pains.
- Nausea and vomiting with abdominal pain. Abdominal pain is continuous.
- Patient is dehydrated with dry tongue with halitosis.
- Yellow colouration on the conjuctiva which deepens with the appearance of jaundice on the skin.
- Bradycardia, despite increasing temperature (facets signs).
- The patient vomits, altered blood (coffee ground) or back vomit or fresh blood with maelena and diarrhoea which may be present.
- Bleeding may take place from the eyes, nose, mouth, bladder, rectum, and other organs.
- Heavy proteinuria with little urine output and presence of grannular cests, RBCs, Hb in urine.
- Death occurs with increasing proteinuria, haemorrhage, rising pulse, hypotension and oliguria.
Diagnosis & Investigations
- Serology (IgM ELISA): Detects yellow fever-specific antibodies.
- Polymerase Chain Reaction (PCR): Identifies viral RNA in blood samples.
- Liver Function Tests: Elevated liver enzymes (AST, ALT), bilirubin. Also listed as Liver function tests (LFTs).
- Complete Blood Count (CBC): Leukopenia, thrombocytopenia.
- Renal Function Tests (RFTs).
Management & Treatment
- No specific antiviral therapy available.
- Supportive care:
- Intravenous fluids for hydration.
- Pain and fever management with paracetamol (avoid NSAIDs due to bleeding risk).
- Monitoring of liver and kidney function.
- Hospitalization for severe cases.
MANAGEMENT OF YELLOW FEVER AIMS
- To limit the spread of the disease.
- Isolate the patient under the mosquito net and always from other people. Do not refer if not very ill to limit the spread.
- Management of fever.
- Manage pain, headache, myalhia with complete bed rest and analgesics.
- Manage dehydration and halitosis; give plenty of fluids to reduce fever and increase urine output.
- Good oral hygiene but take care of not triggering bleeding.
- Avoid rough and hot things in the mouth.
- Avoid drugs due to liver and kidney failure.
- Control any external bleeding.
- Restrict movement in cases of central nervous system involvement. Restrict movement until fully recovered.
- Notify the DDHS immediately.
- Apply the nursing care of patient in isolation.
- Early case findings and reporting.
- Immunization.
Advice before discharging patient home:
- Sleep under mosquito nets.
- Take plenty of fluids with high glucose level.
- Report back in care of any complication.
Complications
- Jaundice.
- Renal failure.
- GIT bleedings.
- Anaemia.
- Meningo-encephalitis.
Prevention & Control
- Yellow Fever Vaccination:
- A single dose provides lifelong immunity.
- Recommended for all individuals in endemic areas, including travelers.
- Vector Control:
- Use of insecticide-treated mosquito nets (ITNs).
- Elimination of mosquito breeding sites (stagnant water removal).
- Spraying using insectcides.
- Use of mosquito nets.
- Personal protective measures:
- Use of mosquito repellants.
- Wearing clothes that fully cover one’s body.
- People moving from a holo endemic areas to an endemic area should sleep in well screened housing.
- Surveillance and Rapid Response:
- Monitoring outbreaks and immediate response to cases.
- Quarantine measures in high-risk areas.
- CONTROL MEASURES:
- Patients should be isolated as their blood and body products may contain virus particles.
VACCINE USE
Target groups include:
- Persons Living or Traveling in Endemic Areas.
- Laboratory Personnel.
Relevance to Midwifery Practice
- Vaccination of Pregnant Women: Generally, yellow fever vaccine is contraindicated in pregnancy unless there is a high risk of exposure.
- Educate expectant mothers on vector control methods.
- Managing Pregnant Women with Yellow Fever:
- Supportive treatment to prevent complications.
- Monitoring for hepatic and renal dysfunction.
- Management of hemorrhagic complications and ensuring safe delivery.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

