Communicable Diseases
HEPATITIS
Table of Contents
Learning Objectives
- Identify the various causes of hepatitis, including viral, chemical, and autoimmune factors.
- Differentiate between Hepatitis A, B, and C based on their virus type, mode of spread, incubation period, and severity.
- Describe the pathophysiology of hepatitis, including the inflammatory process and immune response that lead to liver damage.
- Recognize the clinical features of hepatitis and explain their pathophysiological basis, such as jaundice and clay-colored stools.
- Explain the different syndromic classifications of hepatitis, including acute, chronic, and fulminant hepatitis.
- Outline the principles of management, prevention, and potential complications associated with hepatitis.
HEPATITIS
This is the inflammation of the liver characterized by the presence of inflammatory cells in the tissue of the organ. It may be acute < 6mths or chronic >6mnths depending on the histological appearance of the liver. It is usually a self limiting infection that is healing on its own or can progress to fibrosis or cirrhosis.
Causes
Viral
- Hepatitis A
- Hepatitis B
- Hepatitis C (non A non B)
- Hepatitis D
- Hepatitis E
The first three viruses are the main hepatitis common.
- C.M.V
- E.B.V
- Rubella
- Coxsackie viruses
- Marbug viruses
They cause acute inflammation of the liver.
Drugs and chemicals e.g Paracentamol
Chronic alcoholism
Auto-immnune disorders, fatty liver and metabolic disorders
To a less extent, bacteria, fungi, mycobacteria, protozoa have been seen to cause hepatitis as well.
People with inflammation due to any of above mentioned causes all experience liver inflammation only that the incubation period, MOA and severity of the illness differs.
TYPES
Hepatitis A also called infectious hepatitis is caused by an RNA virus of entero-family and transmitted by the fecal oral route. It commonly affects children and is endemic in areas of the world with poor sanitation. Its a disease of epidemic potential and has a relatively short incubation of (15-45)days.
Hepatitis B has incubation period of 28-180days. Contact with serum of an infected person is the main route of transmission, also other fluids like saliva and semen may also be amode. At most risky people are;H/W, People on B/T frequently and.
Non A non B (C); when an individual has hepatitis that is caused by un identifiable virus. Theses viruses and their antibodies haven’t been indentified and can only be diagnosed by r/o Hep A & B and other indentifiable viruses.
- MOA is acombination of the two A & B
- It has an incubation period of 7-8 weeks and is the commonest cause of chronic hepatitis
Hep D and E,,
Main differences between the three
| Feature | Type A | Type B | Type non A non B( C) |
|---|---|---|---|
| Viruses | RNA picorna virus | DNA Hepadna viruses | Probably 2 types |
| M O spread | Oro-fecal | -Parenteral -Sexual -Vertical transm’n | Oro-feacal Parenteral |
| Incubation period | 15-45days | 29-80days | Not actually known |
| Age of spread | Mostly in children | Mainly adults | All ages |
| Onset | Abrupt | Insidious | Gradual |
| Severity | Mild | Usually severe | Often mild but may be severe |
| Complications | Uncommon | Relatively frequent | Incidence unknown |
| Mortality | Less than 5% | Up to 10% | Unknown |
| Carriers | None | 10% | Frequency/unknown |
Pathophysiology of hepatitis
Each of the hepatitis viruses cause similar liver damage. The inflammatory process is activated throughout the whole liver, and hepatocytes are destroyed by cytotoxic cytokines and natural killer cells, both parts of the inflammatory process. Cellular necrosis takes place. If inflammation affects the periportal areas & cholestasis (the interruption of the flow of bile takes place). The liver is usually able to repair itself and regain complete function if no other complications occur.
- The antigen-antibody complexes that are formed from the interaction of the immune system with the infection circulate throughout the body, which activates the complement system. The person feels malaise, rash, arthritis, fever and angioedema from this activation even abnormal proteins are also produced in the blood, termed cryogloblinemia and the person may also develop vasculitis and glomerulonephritis
Clincal features
| SIGNS/SYMPTOMS | PATHOPHYSIOLOGICAL BASIS |
|---|---|
| Jaundice(conjuctiva,sclera,palms&soles of feet | Due to impaired excretion of bilirubin |
| Clay coloured stool | Bilirubin absence incases of obstructive jaundice &absence ofstercobilin |
| Dark orange urine | Bilirubin excreted in urine instead of faeces & absence of urobilinogen |
| Pluritis valvae & general skin itching | Bile salts accumulate in the skin |
| Right hypochondriac pain | Stretching of the capsules surrounding the liver |
| Fever (mild pyrexia) | Release of pyrogens in the inflammed liver |
| Anorexia,nausea,vomiting | Abdominal dysfunction due to hepatitis |
| Fatigue and weakness(general mailase) | Reduced energy metabolism by the liver |
| Bleeding tendencies | Reduced prothrombin synthesis by hepatocytes |
| Anaemia | Reduced fat soluble vit K absorption due to reduced bile in the intestines, decreased red blood cell life due to liver enzymes alteration |
Syndromic classification of hepatitis
Carrier state; state of the disease with out apparent illness(sub-clinical hepatits). May also be described as asymptomatic hepatistis where there is only serological evidence of infection.
Acute hepatitis; divided into: a) Pre-icteric phase(Prodromal phase )- This phase begins about 2 weeks after exposure to hepatitis. The infection is easily transmitted during this phase & the symptoms are those of acute infection including;
- Fever
- Anorexia/N&V
- Right upper guadrant pain
- Musculoskeletal pain and Rash. This stage ends when
b) Icteric phase; s$s are directly related due to changes in the liver. This is known as the actual phase of illness. It begins 1-2 weeks after the prodromal phase and continues for 2-6 weeks. These include
- Jaundice
- Dark urine
- Pale clay-coloured stools
- The liver becomes enlarged, tender and the person feels pain if the liver is per cussed
c) Convalescence; The recovery begins when the jaundice starts to clear. The liver stays enlarged and tender but the other symptoms start to diminsh. It usually begins 6-8 weeks after exposure. The liver regains normal function 2-12 weeks
Chronic hepatitis; diagnosed when inflammation continues beyond 6months. This may manifest in 2 forms
- a) Chronic persistent hepatitis; is defined as “the persistance of clinical picture and liver inflamm’n after acute hepatitis B, C, D. Liver function tests remain abnormal for > than 6 months, and hep B surface antigen (HbsAg) persists”
- b) Chronic active hepatitis; Is more severe form of the dse & usually leads to severe inflammation and necrosis that ends in fibrosis and cirrhosis. Extra hepatic abnormalities usually x-terise chronic active hepatitis
Fulminant hepatitis; Thisis the worst form of the dse x-terised by gross hepatic insufficiency and hepatic encephalopathy.
Alcoholic hepatitis; An acute and chronic inflamation of the liver due to heavy ETOH. It can be reversible after wthdraw but can lead to cirrhosis and poor prognosis if nt wthdrwn presenting wth;
- Anorexia, N& V
- Abd pain
- Spleenomegally
- Jaundice
- Ascites
- Fever and encephalopathy
Toxic hepatitis; This occurs after exposure to hepatotoxins. These are mostly drugs like;
- Acetaminophen
- Isonniazid
- Tetracycline
- Methotrexate
- Allopurinol
- Phentyoin
- Methyl dopa
- Sulfasalazine
- Aspirin
- CAF & COC’S
Lab Investigations
Diagnosis is made by:
- assessing an individual’s symptoms, physical exam, and medical history
- **Blood tests :**Blood testing includes blood chemistry, liver enzymes, serology and nucleic acid testing. Abnormalities in blood chemistry and enzyme results may be indicative of certain causes or stages of hepatitis
- Serological tests. If Hep B, detection of HBsAg is a diagnostic as HAsAg diagnoses Hep A. these antigens may be found in carriers.
- Imaging: Imaging can identify steatosis of the liver
- liver biopsy is required to demonstrate fibrosis and cirrhosis. Histology indicates neutrophitic / lymphocytic infiltration and hyperplasia of kuffer cells
- Urinalysis-other infections
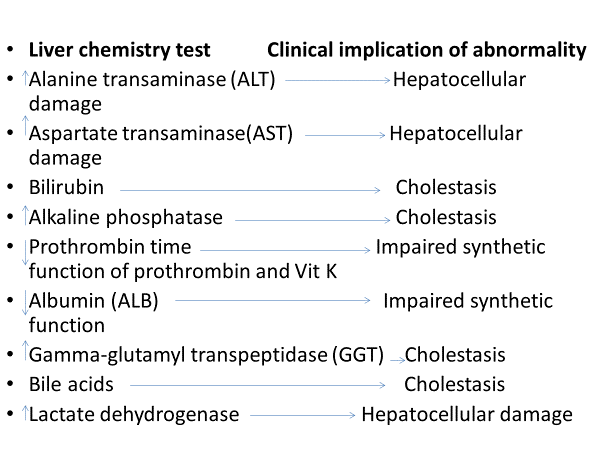
| Test | Clinical implication of abnormality |
|---|---|
| Alanine transaminase (ALT) | Hepatocellular damage |
| Aspartate transaminase(AST) | Hepatocellular damage |
| Bilirubin | Cholestasis |
| Alkaline phosphatase | Cholestasis |
| Prothrombin time | Impaired synthetic function of prothrombin and Vit K |
| Albumin (ALB) | Impaired synthetic function |
| Gamma-glutamyl transpeptidase (GGT) | Cholestasis |
| Bile acids | Cholestasis |
| Lactate dehydrogenase | Hepatocellular damage |
Differential Diagnosis
- Malaria
- Liver abscess
- CCF
- Liver cirrhosis
- Alcoholic hepatitis
- Renal diseases
MGT
Non pharmacological mgt
- Rest
- Proper diet- high glucose diet
- Reduce protein especially if there is impending hepatic encephalopathy
- Maintain adequate hydration
Pharmacological mgt
- Anti- emetics if vomiting e.g Promethazine, Diphenhydramine
- Anti- pyretics Avoid cetamol or give in small doz
- NB; Avoid mdxns that are toxic to the liver e.g Paracetamol
- Hep B Rx-Lamivudine & adefovir dipivoxil
- Hep C Rx-Combn of peginterferon and ribovarin
- Hep A & E- supportive Rx
- I.V- N/S 0.9% and Dex 5% in 2;1 ratio and given in cases of sever vomiting then fuid balanced chart monitored
Prevention
Hepatitis A;
- Passive Hep A Vaccination 1-18mths (2-3doses),6-12mth-boster dose
- Personal hygiene
- Good healthy water supply
- In restaurant,, screening of food handlers should be emphasized
- Good food hygiene
Hepatitis B
- Good control of blood, blood products and sharp instruments
- Personal protection eg using gloves and use of condom
- Immunisation, Hep B vaccine-3doses after testing negative
- Personal hygiene ( use personal tooth brushes, sponges, combs and razors
Nursing concerns
- Jaundice
- Fever
- Right hypochondriac pain
- Bleeding tendencies
- Limit infectiousness
Nursing dignosis
- Impaired skin integrity related to bilirubin accumulating under the skin evidenced by scratch marks due to itching.
- Hypochondriac pain related to inflamed and enlarged liver evidenced by patient’s verbalization and rating its severity on the pain scale.
- Fatigue related to reduced energy metabolism by the liver evidenced by general malaise of the patient.
Complications
- Chronic hepatitis
- Liver failure
- Hepatic coma
- Portal hypertension
- Liver cancer and cirrhosis
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

