Gynaecology
Genital Cancers
Table of Contents
A. Vaginal Cancer
Definition and Risk Factors
A rare cancer that forms in the vaginal lining.
Less common for cancer to begin in the vagina than for cancer to spread there (from uterus or cervix).
Higher risk groups: people above 60 or those having HPV.
Regular pelvic exams and PAP smears are important for early detection, as it often doesn’t cause symptoms.
Types of Vaginal Cancer
Type | Origin Cell | Notes |
|---|---|---|
Squamous cell carcinoma | Flat cells that line the vagina. | Most common type (nearly 90% of all cases). |
Adenocarcinoma | Gland cells in the vagina. | Most common in people above 50. In those below 50, often linked to diethylstilbestrol (DES) exposure in utero. |
Melanoma | Melanocytes (pigment cells). | |
Sarcoma | Connective tissue and muscle tissue of the vaginal wall. | Rhabdomyosarcoma (most common, mostly in children); Leiomyosarcoma (most often in people above 50). |
Signs and Symptoms
Vaginal bleeding unrelated to menstruation, especially after intercourse.
Vaginal bleeding after menopause.
Vaginal discharge that is watery, bloody, or foul-smelling.
Pain during intercourse.
A noticeable mass in the vagina.
Painful urination and pelvic pain.
Constipation or black-colored stools.
Feeling the urge to poop when the bowels are empty.
Diagnostics
History (based on symptoms).
Pelvic exam and Pap smear (Pap) test.
If abnormal cells: colposcopy and vaginal biopsy.
Staging (TNM): Determined by imaging and procedures:
Imaging: X-rays, CT scans, MRI (details about tumor size), and PET scans (show abnormal lymph nodes).
Cystoscopy: To check for cancer spread into the bladder.
Proctoscopy: To check for cancer spread into the rectum/small intestine.
Management and Treatment
Precancerous cells: Laser surgery and topical treatments.
Invasive vaginal cancer: Combination of surgery, radiation, and chemotherapy.
Surgery: Wide local excision, Vaginectomy (partial or radical), and pelvic exenteration.
Radiation: External or internal radiation therapy.
Chemotherapy: Used in conjunction with radiation therapy.
Prevention
Get regular pelvic exams and Pap tests.
Get the HPV vaccine.
Do not smoke.
B. Vulval Cancer
Epidemiology
Commonly a disease of the elderly (peak in the 70th decade of life).
Constitutes only 5% of gynecological cancers.
Often missed or mistaken for a dermatosis, leading to late detection.
Age-adjusted death rate is $0.2/100,000$ women.
Pathogenesis (Squamous Cell Carcinoma)
Majorly squamous cell carcinoma.
Starts at the junction between the keratinized and non-keratinized squamous cell mucosa of the vestibule.
Originates from areas of epithelial cell abnormalities, in VIN (Vulvar Intraepithelial Neoplasia).
Associated with: 65% of cases with VIN; 15-40% with lichen sclerosis.
Close association with oncogenic subtypes of HPV (31, 33, and 45), alongside other factors like smoking and HSV infection.
HPV-related carcinomas have a better prognosis and are more common in younger women.
The type independent of HPV is common among the elderly.
Clinical Features (Symptoms)
Pruritus (itching).
Visible vulva lesions.
Ulcerations of the vulva.
Bleeding.
Pain.
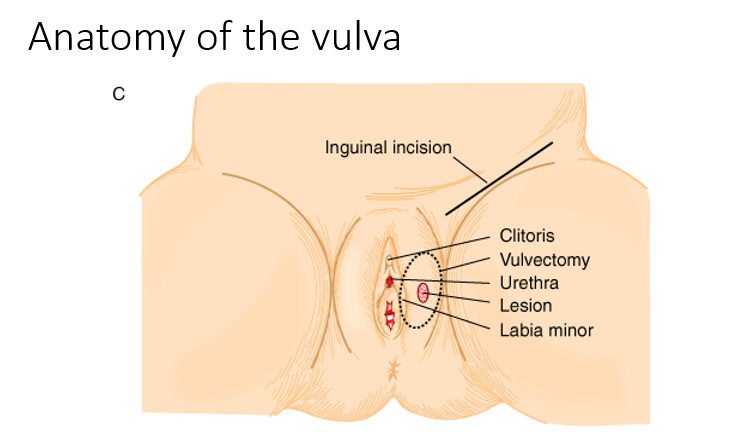
Tumor Spread
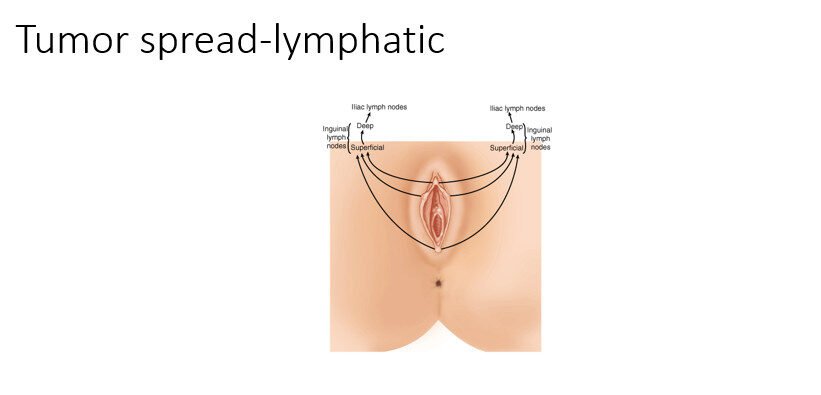
Lymphatic spread: To the superficial and deep inguinal lymph nodes, and potentially to the iliac lymph nodes.
Hematogenous spread: Follows the course of the pudendal arteries (anterior branch of the internal iliac arteries). The superficial external pudendal and deep pudendal arteries are branches of the femoral arteries which drain into the saphenous vein.
Local invasion.
Diagnosis
Vulvoscopy and VIA (Visual Inspection with Acetic Acid).
Vulval tissue biopsy.
Cystourethroscopy and rectosigmoidoscopy.
CT scan for lymph node involvement and distant metastases.
FNAB (Fine-Needle Aspiration Biopsy).
Staging: TNM Classification
Stage | Characteristic | TNM Classification |
|---|---|---|
I | Confined to vulva or perineum. | T1N0M0 |
IA | $\le 2\text{cm}$, stromal invasion $<1\text{mm}$. | |
IB | $\le 2\text{cm}$, stromal invasion $>1\text{mm}$. | |
II | Lesion confined to the vulva or perineum $>2\text{cm}$. | T2N0M0 |
III | Tumor of any size AND adjacent spread to the lower urethra, vagina, and anus OR unilateral lymph node involvement. | T3N0M0, T1N1M0, T2N1M0 |
IVA | Tumor invades any of the following: upper urethra, bladder, rectal mucosa, or bilateral lymph nodes. | |
IVB | Distant mets (metastases) including pelvic lymph nodes. |
Prognosis
Prognosis is dependent on stage, tumor subtype, and histologic differentiation.
Stage I & II: 5-year survival is 80-90%.
Stage III: 5-year survival is 48%.
Stage IV: 5-year survival is 15%.
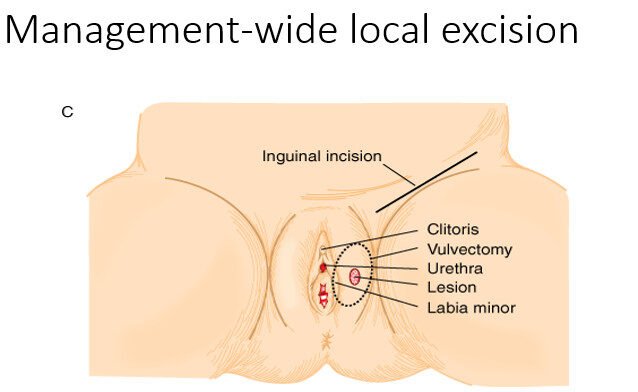
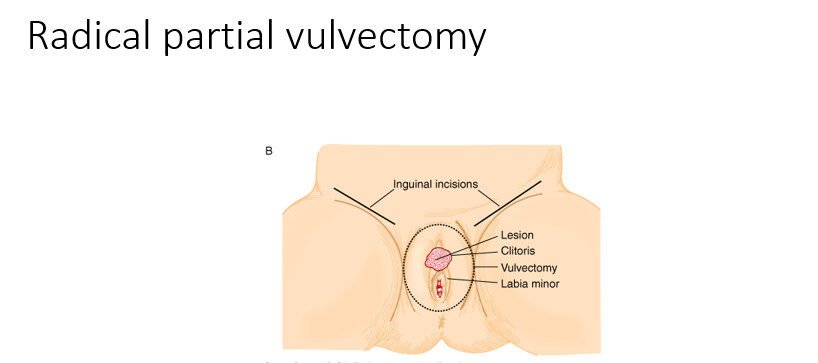
Management
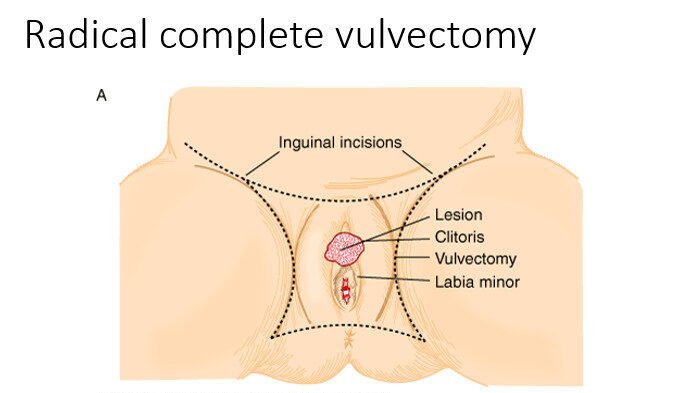
Wide local excision.
Radical partial vulvectomy.
Radical complete vulvectomy.
Other treatment modalities:
Chemo-radiotherapy for advanced vulvar cancers.
This treatment prevents radical and invasive surgeries.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

