Introduction to Midwifery
Key Terminologies in Midwifery
Table of Contents
Definition
Cervical cancer (CaCx), is an abnormal, uncontrolled growth of the cells of the cervix that spread or capable of spreading to other parts of the body and interfere with normal body functions.
It’s one of the many cancers that affect the reproductive system and thus sexual & reproductive health.
Causes of CaCx
It’s caused by infection of the cervix with high risk Human Papilloma Virus (HPV) types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 & 59.
HPV is sexually transmitted, peak of infection at 20-24 yrs.
HPV types-16, 18 & 45 account for 94% of CaCx.
HPV types 16 & 18 account for 70% of cases.
HPV type 16 is the most carcinogenic.
HPV types 6 & 11 cause genital warts & respiratory papillomatosis.
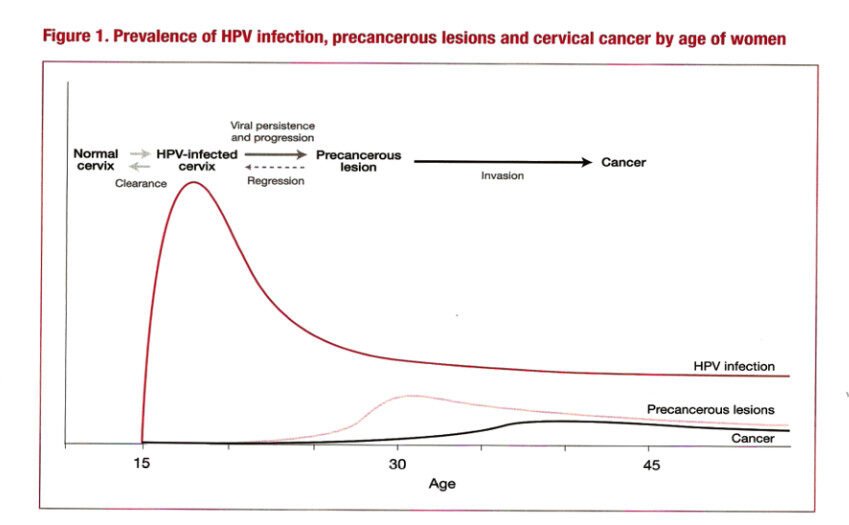
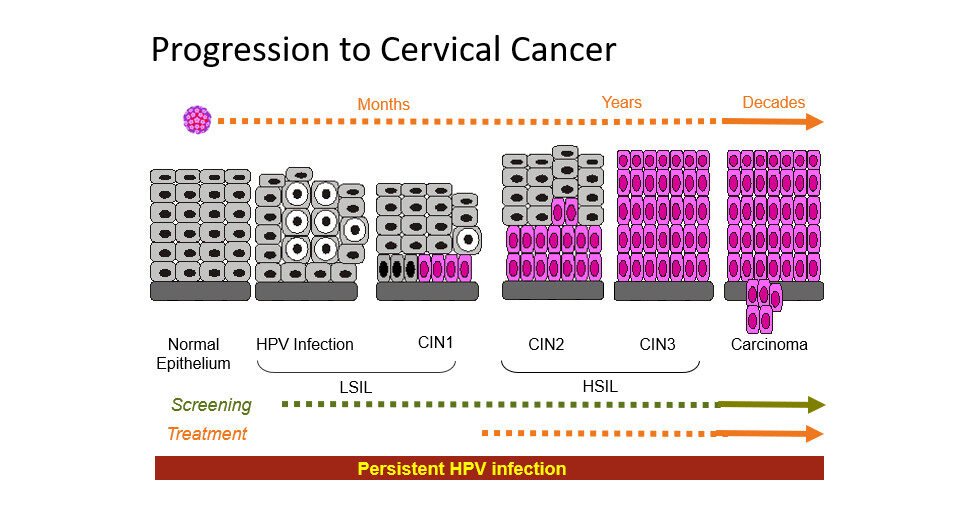
Progression to Cervical Cancer
| Stage | Description |
|---|---|
| Normal Epithelium | Healthy cervical tissue |
| HPV Infection | Initial viral infection |
| CIN1 | Cervical Intraepithelial Neoplasia grade 1 |
| CIN2 | Cervical Intraepithelial Neoplasia grade 2 |
| CIN3 | Cervical Intraepithelial Neoplasia grade 3 |
| Carcinoma | Development of invasive cancer |
Persistent HPV infection leads to progression from LSIL (Low-grade Squamous Intraepithelial Lesion) to HSIL (High-grade Squamous Intraepithelial Lesion) and eventually carcinoma.
Risk Factors for Cervical Cancer
Infection with high-risk HPV
Early sexual intercourse (before 20 years)
Having multiple sexual partners or a partner with multiple sexual partners
Immunosuppression (e.g., HIV infection)
High parity (3 or more children)
Local cervical trauma during childbirth
High rates of cervical abnormalities during pregnancy
High detection rate of HPV among pregnant women
Additional risk factors include:
Long-term use of Combined Oral Contraceptives (COCs) – Estrogen acts as an anti-apoptotic agent, promoting the proliferation of HPV-infected cells and increasing vulnerability to mutations.
Smoking – Smokers have twice the risk compared to non-smokers. Tobacco products are found in cervical mucus and may damage DNA, predisposing to cancer.
Low socioeconomic status – Associated with limited education, poverty, old age, low access to information, poor health care, and lack of screening.
Lack of regular screening for cervical cancer.
Signs and Symptoms of Cervical Cancer
Early stages may be asymptomatic.
Common symptoms include:
Abnormal vaginal bleeding: during or after sexual intercourse, between menstrual periods, or after menopause.
Abnormal vaginal discharge: foul-smelling, watery, thick, mucoid, bloody, or purulent (pus-like).
Pain: lower abdominal pain, lower back pain, and pain during sexual intercourse (dyspareunia).
Abnormal bowel or urinary symptoms: due to pressure on the bladder or rectum or metastasis; may present as constipation, blood in stool, rectal bleeding, hematuria, dysuria, urinary frequency, or obstruction.
On vaginal/speculum examination:
Abnormal cervix with cervical mass or growth (fungating), ulcer, or easily bleeding on contact.
The cervix may be fixed, enlarged, or hard.
Adnexa may be free or fixed with possible vaginal involvement.
Weight loss—common in advanced stages.
Over 80% of women are diagnosed at a late stage, when cure is no longer achievable. Many cases remain undocumented.
Staging of Cervical Cancer (FIGO Classification)
Stage I: Cancer confined to the cervix
IA: Microscopic lesions with stromal invasion ≤5 mm deep and ≤7 mm wide
IA1: Invasion ≤3 mm in depth
IA2: Invasion >3 mm depth
IB: Macroscopic lesions confined to the cervix
IB1: Lesions ≤4 cm in size
IB2: Lesions >4 cm in size
Stage II: Cancer extends beyond the cervix but not to pelvic wall or lower third of vagina
IIA: No parametrial involvement
IIA1: Tumor <4 cm, involves upper two-thirds of vagina
IIA2: Tumor >4 cm, involves upper two-thirds of vagina
IIB: Obvious parametrial involvement
Stage III: Tumor extends to pelvic wall and/or lower third of vagina
IIIA: No extension to pelvic walls but involves lower third of vagina
IIIB: Extension to pelvic walls or causes hydronephrosis/nonfunctioning kidneys
Stage IV: Tumor extends beyond true pelvis or involves bladder/rectum
IVA: Growth to adjacent pelvic organs
IVB: Spread to distant organs (liver, lungs)
Treatment of Cervical Cancer
| Stage | Recommended Treatment |
|---|---|
| Stage 0 (Carcinoma in situ / CIN) | Cryotherapy, LEEP (Loop Electrosurgical Excision Procedure), or Simple Total Hysterectomy |
| Stage IA1 | Total hysterectomy or radical hysterectomy |
| Stage IA2, IB, IIA | Combined radiotherapy and radical hysterectomy with bilateral pelvic lymphadenectomy |
| Stage IIB, III, IVA | Cisplatin-based chemotherapy combined with radiotherapy |
| Stage IVB & Recurrent Cancer | Palliative radiotherapy or chemotherapy |
Prevention of Cervical Cancer
1. Sexual Behavior Change
Abstinence
Avoiding early sexual debut
Avoiding multiple sexual partners
Consistent condom use
2. Vaccination
HPV vaccine (Gardasil) — quadrivalent, active against HPV types 6, 11, 16, and 18.
Administered as two IM injections (0 and 6 months) before sexual debut.
Target group: girls aged 10–14 years.
3. Cervical Cancer Screening
Methods:
Visual Inspection with Acetic Acid (VIA)
Visual Inspection with Lugol’s Iodine (VILI)
PAP smear
HPV DNA testing
Colposcopy and Cervical Biopsy
4. Early Treatment of Premalignant Lesions
Cryotherapy
LEEP
Thermocoagulation
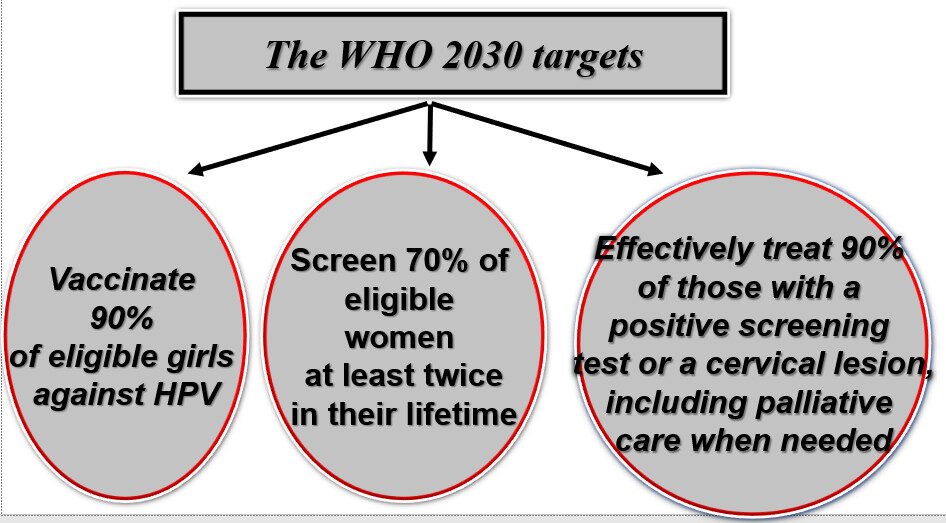
WHO 2030 Targets
- 90% of eligible girls vaccinated against HPV
- 70% of eligible women screened at least twice in their lifetime
- 90% of women with positive screening tests or lesions effectively treated (including palliative care)
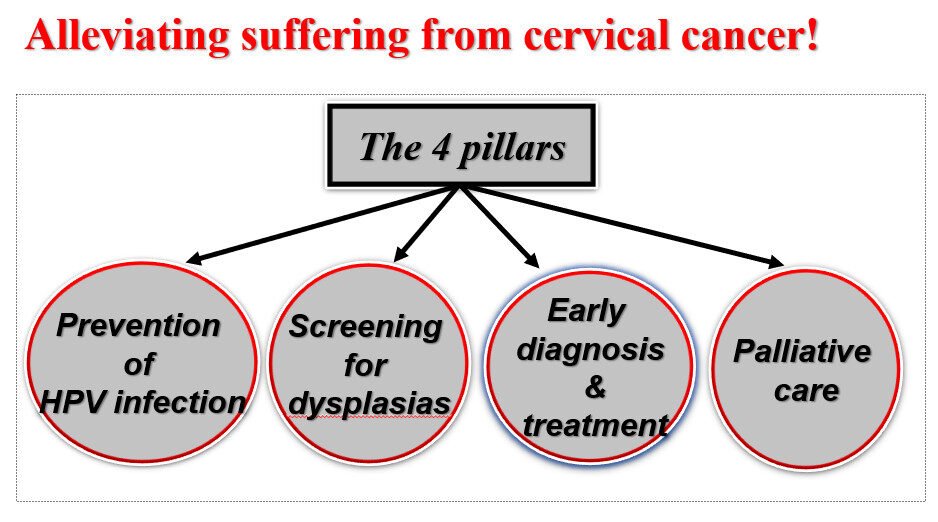
The Four Pillars of Cervical Cancer Control
- Prevention of HPV infection
- Screening for dysplasias
- Early diagnosis and treatment
- Palliative care
Cervical Cancer Screening Methods
Early detection of cervical cancer through screening in women aged 25 years and above, followed by treatment of precancerous lesions, can prevent the majority of cases.
Screening is a public health intervention aimed at asymptomatic populations to identify individuals at increased probability of having disease or precancerous lesions.
Screening Methods:
VIA (Visual Inspection with Acetic Acid)
VILI (Visual Inspection with Lugol’s Iodine)
PAP smear
HPV DNA testing
Note: Cervical biopsy and colposcopy are diagnostic, not screening tools.
Visual Inspection with Acetic Acid (VIA)
Uses 3–5% acetic acid, which causes reversible protein coagulation in tissues with high DNA concentration—appearing white (“acetowhite”).
Physiologic conditions with high nuclear activity that may transiently turn white: mature metaplasia and columnar epithelium.
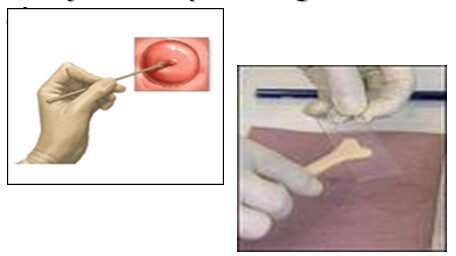
Procedure:
Place patient in lithotomy position.
Insert and adjust speculum.
Remove discharge using dry or saline-soaked cotton swab.
Apply acetic acid to cervix and wait one minute.
Indications:
Used in women below 50 years (with visible squamocolumnar junction).
For postmenopausal women (SCJ recedes), use PAP smear instead.
Visual Inspection with Lugol’s Iodine (VILI)
Uses 5% Lugol’s iodine, a glycophilic solution staining glycogen-rich tissues dark brown.
Normal mature squamous epithelium → dark brown
Columnar epithelium → pinkish (no glycogen)
Precancerous/glycogen-poor tissues → yellow
Physiologic glycogen-poor states (iodine negative):
Columnar epithelium (pinkish)
Postmenopausal/hypo-estrogenic states (yellow)
A VILI positive area may indicate benign lesion, precancerous lesion, or cancer.
PAP Smear
Sample from vagina and cervix applied to slide for cytopathological analysis.
HPV DNA Testing
Detects presence of HPV in the cervix.
More expensive than other methods.
Colposcopy
Uses a colposcope (magnifying device).
Indications:
Abnormal cytology
Grossly abnormal cervical lesions (even if cytology negative)
Postcoital bleeding (even if smear negative)
Re-screening Intervals
HIV-positive women: every 1 year
HIV-negative women: every 3 years
Post-treatment follow-up (LEEP or cryotherapy for CIN2/CIN3): after 1 year
Treatment of Precancerous Lesions
Cryotherapy

Uses cryoprobes, cryogun, pressure gauge, and stopwatch.
Metal probe cooled by CO₂ or N₂O gas freezes abnormal ectocervical tissue (destructive therapy).
No anesthesia needed.
Procedure:
Two successive freeze–thaw cycles:
3-minute freeze → 5-minute thaw → repeat
Indications:
CIN 2–3 lesions not suspicious of cancer
Lesions fully covered by cryoprobe
No >2 mm endocervical canal extension
Not used in pregnancy
Side effects: mild pelvic pain, watery discharge, light bleeding up to 2 weeks, rarely infection or cervical stenosis.
Loop Electrosurgical Excision Procedure (LEEP)
Uses fine stainless steel or tungsten wire loop electrodes (0.2 mm) to excise the transformation zone containing lesions.
Indicated for:
Early-stage suspicious lesions
Lesions ineligible for cryotherapy/thermocoagulation
Lesions with >2 mm endocervical extension
Not used in pregnancy
Side effects: similar to cryotherapy and thermocoagulation. Rarely, may cause:
Spontaneous miscarriage (due to cervical incompetence)
Prolonged labor (due to cervical stenosis)
Thermocoagulation
Uses a probe heated to 100°C to destroy ectocervical abnormal tissue (destructive therapy).
Performed without anesthesia.
Procedure:
Single application lasting 60 seconds.
Indications:
CIN 2–3 lesions not suspicious of cancer
Lesions ≤2 mm endocervical extension
Not used in pregnancy
Side effects: mild pelvic pain, watery discharge, spotting or light bleeding for 2 weeks, rarely infection or cervical stenosis.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

