Gynaecologhy
UTERINE CANCER
Table of Contents
Introduction
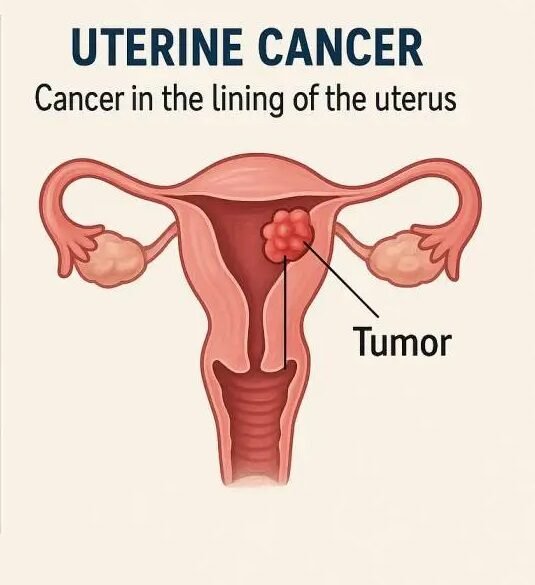
Uterine cancer refers to tumors that arise from the uterine corpus (the body of the uterus).
The most common form is endometrial cancer, which originates from the lining of the uterine cavity known as the endometrium.
Endometrial cancer usually arises from the glandular component of the endometrium.
Classification of Endometrial Tumors
Endometrial cancers are classified into two main types depending on their histological subtype:
Type 1 Tumors
Endometrioid adenocarcinomas
Estrogen-driven
Arise from a background of endometrial hyperplasia
Account for 75–80% of all endometrial tumors
Generally low-grade and have a good prognosis
Type 2 Tumors
Include high-grade serous and clear cell histological subtypes
Arise from an atrophic endometrium
More aggressive and associated with a worse prognosis
Sarcomas of the Uterus
Uterine sarcomas are derived from the stromal cells and may be endometrial or myometrial in origin.
These are rare tumors, accounting for approximately 5% of all uterine cancers.
The most common types are:
Leiomyosarcomas
Carcinosarcomas
Classification
Pure sarcomas
Mixed epithelial sarcomas
Heterologous sarcomas
Pure Sarcomas
This group includes:
Endometrial stromal sarcomas
Leiomyosarcomas
Endometrial stromal sarcomas occur mainly in perimenopausal women, presenting with irregular bleeding and a soft, enlarged uterus.
The majority of these tumors are low grade.
Leiomyosarcomas are rare tumors of the myometrium.
They are rarely (0.75%) associated with malignant transformation of benign fibroids and often present with:
Rapidly growing pelvic mass
Pelvic pain
Other symptoms include:
Postmenopausal bleeding
Vaginal discharge
Pelvic pain or pressure symptoms
Preoperative diagnosis is difficult but may be aided by MRI, which can delineate areas of necrosis within a fibroid suggestive of malignant transformation.
Treatment:
Surgery is the mainstay.
Adjuvant therapy may be considered if the mitotic count is high (>10 mitoses per high-powered field).
Metastatic spread is usually vascular, involving distant sites such as the lungs and brain.
Mixed Epithelial Sarcomas (Carcinosarcomas)
This group, formerly known as malignant mixed Müllerian tumors, contains both carcinomatous and sarcomatous elements.
The carcinomatous component is usually glandular.
The sarcomatous component can be:
Homologous: composed of tissues normally found in the uterus (endometrial, stromal, and/or smooth muscle).
Heterologous: composed of tissues not normally found in the uterus (bone, cartilage, skeletal muscle).
Presentation of Mixed Epithelial Sarcomas
Most cases occur after menopause.
Sometimes associated with previous pelvic irradiation.
Typical presentation includes:
Postmenopausal bleeding (PMB)
A fleshy mass protruding from the cervix
An enlarged, soft uterus
Treatment
Surgery is the main treatment.
Followed by postoperative radiotherapy.
Prognosis:
5-year survival: 73% if confined to uterus
5-year survival: 25% if tumor spreads beyond the uterus
Heterologous Sarcomas
These rare tumors consist of sarcomatous tissue not normally found in the uterus, such as:
Striated muscle
Bone
Cartilage
The most common is rhabdomyosarcoma, which may occur in children, presenting as:
A grape-like mass protruding from the cervix
Watery vaginal discharge
Histology: reveals primitive rhabdomyoblasts.
Recurrence rates are high with frequent distant metastases.
Risk Factors for Endometrial Cancer
Obesity
Diabetes mellitus
Nulliparity
Late menopause (>52 years)
Unopposed estrogen therapy
Tamoxifen therapy
Family history of colorectal or endometrial cancer
Presentation of Endometrial Cancer
Most commonly occurs in postmenopausal women.
Usually presents early, often following postmenopausal bleeding (PMB).
Approximately 5–10% of women with PMB have an underlying gynecological malignancy.
→ This is a “red flag” symptom and should always be investigated.
In premenopausal women, it presents with:
Abnormal uterine bleeding (heavy, irregular, or intermenstrual bleeding).
Advanced disease may present with:
Abdominal pain
Urinary dysfunction
Bowel disturbances
Respiratory symptoms
Signs and Symptoms of Endometrial Cancer
Bleeding from the cervical os during speculum examination
Bulky uterus on bimanual pelvic examination
In many women, pelvic examination may be normal
Pain may indicate metastatic spread
Discharge may be present, often associated with pyometra
Diagnosis
Postmenopausal bleeding (PMB) is a critical symptom that must always be investigated.
Steps in assessment:
Inspection of external genitalia
Speculum examination – to exclude vulval, vaginal, and cervical cancers as potential causes.
Investigations
Transvaginal Ultrasound Scan (TVUSS)
Hysteroscopy
Endometrial biopsy
FIGO Staging of Carcinoma of the Uterus
| Stage | Description |
|---|---|
| I | Tumor confined to uterine body |
| IA | Less than 50% myometrial invasion |
| IB | More than 50% myometrial invasion |
| II | Tumor invading cervix |
| III | Local and/or regional spread |
| IIIA | Invades serosa of uterus |
| IIIB | Invades vagina and/or parametrium |
| IIIC | Metastases to pelvic and/or para-aortic nodes |
| IV | Tumor invades bladder and/or bowel or has distant metastases |
Management of Endometrial Cancer
Surgery
Surgery is the mainstay of treatment.
The extent of surgery depends on:
Tumor grade and stage
Patient’s comorbidities
Standard surgery:
Total hysterectomy with bilateral salpingo-oophorectomy (BSO) — removal of uterus, both fallopian tubes, and ovaries.
Can be performed:
Abdominally
Laparoscopically (total, vaginally assisted, or robotically)
If MRI suggests cervical involvement, a modified radical hysterectomy is performed, which includes:
Removal of a cuff of vagina
Paracervical and parametrial tissues
Ensures adequate excision margins
Advanced or High-Grade Disease
If the tumor is:
High grade (Grade 3) or
Type 2 histology,
many centers perform pelvic and para-aortic lymph node dissection, since nodal disease (pelvic or para-aortic) occurs in about one-third of patients.
However, the role of nodal dissection is contentious.
The ASTEC trial (large UK study) found no survival benefit from pelvic node dissection in endometrial cancer.
Adjuvant Treatment
Radiotherapy
Postoperative radiotherapy reduces local recurrence but does not improve overall survival.
Strategies:
Brachytherapy (localized vaginal vault radiotherapy) for early/local disease
External beam radiotherapy + brachytherapy for stage III or locally advanced disease
Chemotherapy
Used for advanced or metastatic disease.
Evidence supporting its efficacy remains limited.
Hormonal Therapy
High-dose progestins (oral or intrauterine) are effective in some women with:
Complex atypical hyperplasia
Low-grade stage IA endometrial carcinoma
However, relapse rates are high after hormonal treatment.
Differential Diagnosis for Pelvic Masses
From the Uterus
Fibroids (leiomyomas)
Uterine malformations
Blood accumulation (hematometra)
Pyometra
Uterine body neoplasms
From the Ovaries
Endometriosis
Functional or organic ovarian cysts
Benign and malignant ovarian tumors
From the Fallopian Tubes
Tubo-ovarian abscess
Pelvic inflammatory disease
Hydrosalpinx
Para-ovarian cysts
Ectopic pregnancy
Fallopian tube neoplasms
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

