Obstetric Anatomy and Physiology
The Menstrual Cycle
Table of Contents
Definition and Controlling Factors
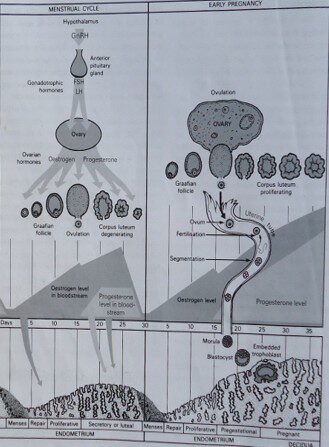
The menstrual cycle is a series of changes that take place in the uterine endometrium (reproductive lining). These changes are governed indirectly by the gonadotrophic hormones (from the pituitary gland) and directly by the ovarian hormones (Oestrogen and Progesterone).
Factors which play a part in the Menstrual Cycle:
The Anterior Pituitary Gland (A.P.G): Secretes Gonadotrophic hormones (FSH and LH).
The Ovaries: Produce the ovum and the ovarian hormones (Oestrogen and Progesterone).
The Fallopian Tube: Propels the ovum.
The Uterus: Sheds and regenerates the Endometrium.
The Vagina: Serves as the outlet for the discharged contents.
The cycle starts at the age of puberty (12-16 years) and continues until menopause (45-50 years). An average cycle lasts for about 28-30 days, but variations between 35-42 days may occur.
PHASES OF THE MENSTRUAL CYCLE
The menstrual cycle consists of four distinct phases:
Menstruation
Proliferative or Regenerative Phase
Secretory Phase
Degenerative Phase
1. Menstruation
This is a normal physiological discharge of blood from the uterine Endometrium when fertilization has not taken place. The discharge consists of torturous blood vessels, endometrial tissue, blood, mucus, and the unfertilized ovum.
The Endometrium sheds down to the basal layer, leaving the basal layer with the endometrial glands intact.
This phase lasts for 4-5 days, and the total amount of blood loss should not exceed $100\text{m}\ell\text{s}$.
Hormonal Status: The Anterior Pituitary Gland is inactive, and the ovaries release no hormones.
2. Proliferative Phase (Regenerative Phase)
This period of healing and regeneration begins soon after menstruation and lasts for about 10 days until ovulation.
The Anterior Pituitary Gland secretes F.S.H (Follicle Stimulating Hormone).
F.S.H stimulates the Graafian follicles to mature.
The ovaries are stimulated to produce Oestrogen, which helps in building and growing the Endometrium, leading to its regeneration.
A mature Graafian follicle ripens and ruptures, discharging an ovum (ovulation) prior to day 14 of the next period.
Soon after ovulation, FSH is withdrawn and the Oestrogen level drops.
3. Secretory Phase
This phase of secretion begins soon after ovulation and lasts for about 10 days.
The Anterior Pituitary Gland secretes Luteinizing Hormone (L.H.).
L.H. causes the ruptured follicle to develop into the Corpus Luteum (a yellow body) in the ovary, which prevents other mature ova from ripening.
The Corpus Luteum produces Progesterone (along with Oestrogen).
Progesterone and Oestrogen make the Endometrium become thicker, soft, spongy, and highly secretory, rich in nutrients in preparation for a fertilized ovum.
In cycles longer than 28 days, it is usually the Proliferative Phase that is extended, not the Secretory Phase.
Towards the end of this phase, L.H. levels decline, and Progesterone and Oestrogen levels begin to drop.
4. Degenerative Phase
This phase occurs about 4 days before menstruation when fertilization does not occur.
The Luteinizing Hormone is withdrawn.
The Corpus Luteum degenerates, becoming the Corpus Albicans.
The ovaries cease producing Oestrogen and Progesterone.
The Endometrium shrinks, secretion stops, and the torturous blood vessels shrink and become kinked.
The Endometrium becomes old and degenerates. This period is then followed by menstruation again.
DISORDERS OF MENSTRUATION
A. Amenorrhoea (Absence of Menstruation)
This is the absence of menstruation and is graded by type.
1. Apparent Amenorrhoea (Cryptomenorrhoea): This occurs when the period contents are produced but not expelled due to an obstruction, such as an imperforated hymen.
2. Primary Amenorrhoea: Menstruation has never occurred. A gynecological consultation is advised if periods have not started by age 17.
Causes:
Congenital Abnormalities: Malformation of the uterus, vagina, or ovaries.
Hormonal Imbalance/Dysfunction: Mal-developed or dysfunctional Anterior Pituitary Gland (Hypopituitarism) or issues with the thyroid/adrenal glands.
Serious Illness.
Note: Primary amenorrhoea is often due to a permanent defect of the ovaries.
3. Secondary Amenorrhoea: Menstruation ceases after it had been established for months or years.
Causes:
Pregnancy: The most common cause if fertilization has occurred.
Emotional/Psychological: Excitement, worry, fear, or change of environment.
Glandular Dysfunction: May be associated with over-secretion of the thyroid gland or Adrenaline.
Hormonal/Medication: Contraceptive pills (use of Progesterone and Oestrogen).
Lactation: If it is full-time breastfeeding.
Infection/Systemic Illness: Pulmonary tuberculosis, severe Inflammatory diseases of the pelvis, severe Anemia, HIV infection, or malnutrition.
Menopause.
B. Dysmenorrhoea (Painful Periods)
Painful menstruation, usually of uterine origin, which can be severe enough to require bed rest. The pain is often colicky due to uterine muscle contractions, lasting for the first 12 hours of menses. It can sometimes be accompanied by nausea, vomiting, or diarrhea.
1. Primary Dysmenorrhoea (Spasmodic): Pain is directly due to the mechanism of menstruation itself.
Causes:
Obstruction: Narrow cervical os or malposition of the uterus.
Vaso-constriction: Vaso-constriction of terminal arteries leading to Ischemia, causing spasms and uterine pain.
Hypomenorrhoea: Associated with clots in the cervical os that must be expelled.
2. Secondary Dysmenorrhoea (Congestive): Pain develops after menstruation has been established for many years (usually after age 30) and is often associated with inflammation or other pelvic conditions.
Causes: Pelvic congestion brought about by infections, inflammation of the pelvic organs, retroversion of the uterus, fibroids, or cancer. Psychological factors like anxiety, emotional upset, or domestic problems may also contribute.
3. Membranous Dysmenorrhoea: The whole part of the Endometrium is shed in one piece, which is very painful to expel.
Causes: Due to dysfunction of the Anterior Pituitary Gland (A.P.G).
Management: Management should start with non-pharmacological methods:
Placing warm compress on the lower abdomen.
Waist massage.
Keeping busy and taking warm water.
If this fails, pharmacological therapy with NSAIDS can be initiated (e.g., Ibuprofen $400\text{m}g$ or Mefenamic acid $500\text{m}g$ every 8 hours for 3 days). In rare cases, cervical dilation may provide a permanent cure.
C. Other Frequency and Volume Disorders
1. Scanty Frequent Menstruation (Hypomenorrhoea): Common and often clears up after treatment.
Causes: Before menopausal age, causes include emotional upset, illness, and hormonal imbalance.
2. Menorrhagia (Too Frequent/Excessive Bleeding): Too frequent bleeding, excessive bleeding at the time of the period, or both. This is a symptom, not a disease.
Causes:
Uterine/Cervical Issues: Fibroids, Endometritis, Endometrium/cervical polyps, Cervical erosions, or Carcinoma.
Hormonal/Glandular: Disturbances due to emotional upset, hormonal imbalance (usually excessive Oestrogen), Ovarian bleeding, or Thyroid dysfunction (e.g., Myxoedema).
Systemic: Anemia, Blood disorders.
3. Oligomenorrhoea (Infrequent Periods): Low intervals between periods, which occur only 2 or 3 times a year.
4. Metrorrhagia (Intra-Menstrual Bleeding): Bleeding that occurs between periods.
Causes: Cervical erosion, Fibroids, Polyps, Carcinoma, or Ovarian issues.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

