Obstetric Anatomy and Physiology
Fetal Circulation
Table of Contents
Definition of Fetal Circulation
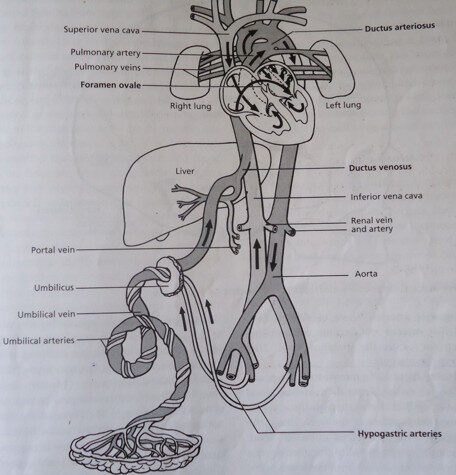
It is the circulation developed by the fetus in the utero. During intrauterine life, the lungs of the fetus are inactive, and the interchange of oxygen and carbon dioxide takes place in the placenta. Extra structures are therefore present in the fetal circulating system which become useless once the extrauterine function of respiration is established.
Before the fetal circulation can be fully understood, the general structure and principles of the adult circulation must be brought to mind.
Factors Needed in Establishment of Respiration
Baby should be born at 38 weeks of gestation, having matured lungs, alveoli, and a matured medulla oblongata (respiratory centers).
Accumulation of carbon dioxide is beneficial to set the lungs ready for respiration.
The extra coldness and handling of the baby stimulate it to gasp and cry, which widens the lungs.
The Adult Circulation System
Venous return from the lower limbs is returned to the right auricle of the heart by the inferior vena cava, and venous blood from the upper extremities is returned to the right auricle by the superior vena cava.
From the right auricle, blood passes through the tricuspid valve to the right ventricle and is then pumped to the lungs for replacement of oxygen by the pulmonary artery.
Four pulmonary veins take the newly oxygenated blood from the lungs to the left auricle of the heart, where it passes through the mitral valve into the left ventricle.
From the left ventricle, the Aorta sends blood into two streams: the ascending branch supplies the head and the upper limbs; the descending branch supplies parts of the body below the level of the diaphragm.
Following its circulation to the upper and lower extremities, the blood is returned again to the heart by the superior and inferior vena cava.
The Fetal Circulatory System
Blood which has circulated and been refreshed is carried by two umbilical arteries in the umbilical cord to the placenta, where an interchange takes place between fetal and maternal blood by a process of osmosis (this is from low concentration to high concentration) and diffusion (from high concentration to low concentration), as well as by the selective action of the cytotrophoblast and the syncytiotrophoblast.
The four layers that separate fetal from maternal blood are:
Syncytiotrophoblast
Cytotrophoblast
Mesoderm
Capillary wall.
Carbon dioxide and other excretory products are given off into the maternal blood. Nutritional substances and oxygen are picked up. It’s important to realize that blood which circulates within the fetal umbilical and placental vessels is fetal in origin.
Umbilical Vein
Carries blood rich in oxygen from the placenta to the undersurface of the liver. The hepatic vein leaves the liver and returns blood to the inferior vena cava.
The Inferior Vena Cava
Already transmitting blood which has circulated in the fetal lower limbs and trunk, it is thus joined by blood from the hepatic vein and Ductus Venosus and takes it to the right auricle of the heart.
Ductus Venosus
Branches from the umbilical vein and transmits the greater amount of the oxygenated blood into the inferior vena cava.
The Foramen Ovale
Allows the greater part of oxygenated blood in the right auricle to pass to the left auricle, where it is then passed through the mitral valve to the left ventricle and then through the aorta into the ascending branch to supply the head and upper extremities. It can be seen, therefore, that the liver, heart, and the brain receive the best supply of the newly oxygenated blood.
Superior Vena Cava
Returns the blood from the head and upper extremities to the right auricle. This, with the remainder of the stream brought in by the inferior vena cava, passes through the tricuspid valve and into the pulmonary auricle.
Pulmonary Arteries
Shunts some of the supply of mixed blood to the non-functioning lungs, which fortunately require only little nourishment (25%).
Ductus Arteriosus
Shunts the greater amount of blood from the left ventricle directly into the descending aorta to supply the abdomen, pelvis, and lower extremities.
Hypogastric Arteries
These are the extensions of the internal iliac arteries carrying blood back to the placenta, where more oxygen and nutrients are supplied from the maternal blood.
Additional Structures in Fetal Circulation
The cord has two umbilical arteries that return deoxygenated blood and fetal waste to the placenta. One umbilical vein brings oxygenated blood and nutrients to the fetus.
Umbilical Vein
Carries oxygenated blood and nutrients from the placenta to the fetus. When the vein enters the undersurface of the liver, it has a branch which joins the portal vein and supplies the liver. The hepatic vein leaves the liver and returns blood to the inferior vena cava. Blood is dispersed in this way: ½ of the blood enters the liver while the other half comes into the ductus venosus.
The Ductus Venosus
(From vein to vein) Connects the umbilical vein to the inferior vena cava. At this point, the blood mixes with deoxygenated blood returning from the lower parts of the body; thus, the blood throughout the body is at best partially oxygenated. Blood is shunted from the right atrium to the left atrium, skipping the lungs. More than one-third of blood takes this route, where it is then passed through the mitral valve to the left ventricle, through the aorta into its ascending branch to supply the head and the upper extremities.
The Superior Vena Cava
Returns blood from the head and upper extremities to the right atrium. This, with the remainder of the stream brought in by the inferior vena cava, passes through the tricuspid valve into the right ventricle.
The Pulmonary Artery
Shunts some of this supply of the mixed blood to the non-functioning lungs, which fortunately require little nourishment.
The Foramen Ovale
Is a temporary opening between the atria which allows the majority of blood entering from the inferior vena cava to pass across into the left atrium. The reason for this diversion is that the blood does not need to pass through the lungs since it is already oxygenated.
Ductus Arteriosus
(From an artery to an artery) Leads from the bifurcation of the pulmonary artery to the descending aorta, entering it just beyond the point where the subclavian and carotid arteries leave. (Shunts the amount part of the blood from the right ventricle directly into the descending aorta to supply the abdomen, pelvis, and lower extremities).
The Hypogastric Arteries
Branch off from the internal iliac arteries and become the umbilical arteries when they enter the umbilical cord. They return the blood to the placenta where more oxygen and nutrients are supplied from the maternal blood.
The blood takes about half a minute to circulate. From the placenta, blood passes along the umbilical vein (This is the only vessel in the fetus which carries unmixed blood).
Summary
Umbilical vein: Carries oxygenated blood from the placenta to the undersurface of the liver.
Ductus venosus: Leaves the umbilical vein before it reaches the liver and transmits the greater part of the newly oxygenated blood into the inferior vena cava.
Foramen ovale: Is an opening which allows the passage of blood from the right auricle into the left auricle.
Ductus Arteriosus: A bypass extending between the right ventricle and ends at the descending aorta.
Hypogastric arteries: Two vessels that return blood from the fetus to the placenta.
Adaptation (Changes at Birth) to Extrauterine Life
At birth, the baby takes a breath, and blood is drawn to the lungs through the pulmonary arteries. It is then collected and returned to the left atrium via the pulmonary veins, resulting in a sudden inflow of blood. The placental circulation ceases soon after birth, and so less blood returns to the right side of the heart. In this way, the pressure in the left side of the heart is greater, while that in the right side of the heart becomes less. This results in the closure of a flap over the foramen ovale, which separates the two sides of the heart and stops the blood flowing from right to left.
With the establishment of pulmonary respiration, the oxygen concentration in the blood stream rises. This causes the Ductus Arteriosus to constrict and close.
The cessation of the placental circulation results in the collapse of the umbilical vein, the Ductus Venosus, and the hypogastric arteries. These immediate changes are functional, and those related to the heart are reversible in certain circumstances; later, they become permanent and anatomical.
Changes at Birth
The umbilical vein becomes the Ligamentum teres.
The Ductus venosus becomes the Ligamentum venosum.
The Ductus Arteriosus becomes the Ligamentum Arteriosum.
The foramen ovale becomes the fossa Ovalis.
The hypogastric arteries are known as the obliterated hypogastric arteries, except for the first few centimeters which remain open as the superior vesicle arteries.
Congenital Anomalies
Ventricular Septal Defect
This is formed as a result of incomplete closure of the walls between the two ventricles. This leads to the mixing of oxygenated and deoxygenated blood.
Atrial Septal Defect
Incomplete closure of the walls between the two atria.
Patent Ductus Arteriosus
Failure of the Ductus Arteriosus to close at birth leads to a mixture of blood.
Fallot’s Tetralogy
Means transposition of the great vessels. This is the commonest cause of cyanotic lesions. Malformations that interfere with the blood flow from the left ventricle. These are:
Stenosis of the pulmonary artery
Ventricular septal defect
Aortic misplacement
Right ventricular hypertrophy.
Cyanosis occurs because blood bypasses the lungs and joins the systemic circulation without being oxygenated.
Acyanotic Heart Lesions
These include:
Ventricular septal defect
Patent Ductus Arteriosus
Pulmonary stenosis
Aortic stenosis
Atrial septal defect
Coarctation of the aorta
Presentation
Neonates with cyanotic or acyanotic heart defects will present with:
History of breathlessness
Failure to thrive
Signs of congestive cardiac failure
Management
Surgery to correct the defect.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

