Mental Health
Acute Conversional Dissociative Disorders
Table of Contents
Definition
Conversion disorder is characterized by the presence of one or more physical symptoms suggesting a neurological or medical condition that cannot be explained by any known physiological disorder. Instead, psychological factors like stress and conflicts are strongly associated with the onset or exacerbation of the symptoms. Patients are genuinely unaware of the psychological basis and are thus unable to consciously control their symptoms. This disorder was formerly referred to as ‘hysteria.’
Etiology
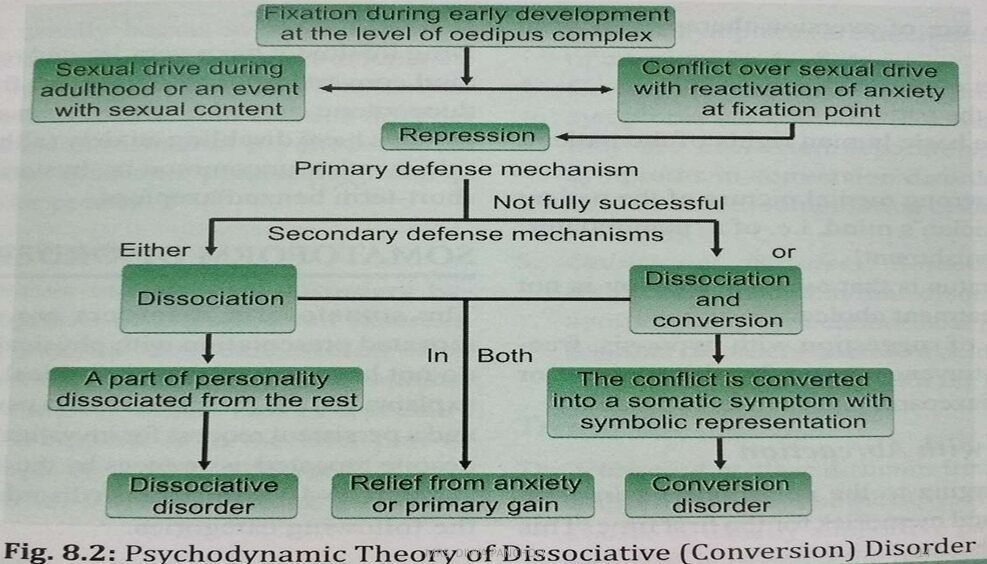
Psychodynamic Theory
According to this theory, the ego defense mechanisms involved are repression and conversion. Conversion symptoms allow a forbidden wish or urge to be partly expressed while sufficiently disguised, preventing the individual from consciously facing the unacceptable internal conflict. The symptoms are often symbolically related to the underlying conflict.
Behavioral Theory
This theory suggests that the symptoms are learned behaviors from the surrounding environment. These symptoms bring about psychological relief by allowing the individual to avoid stress. Conversion disorder is more common in people with histrionic personality traits.
Clinical Features
Primary Gain: The symptoms reduce the patient’s anxiety by keeping the psychological conflict out of conscious awareness.
Secondary Gain: The symptoms provide an advantage to the patient, such as escaping an unpleasant duty (e.g., psychogenic paralysis escaping a responsibility).
La Belle Indifference: The patient often shows surprisingly little distress or a lack of concern about the severity of their physical symptoms.
Intentionality: The patient does not intentionally produce the symptoms.
Medical Findings: Physical examination and investigations do not reveal any medical or neurological abnormalities consistent with the symptoms.
Types of Conversion Disorder
Dissociative Motor Disorders
These are characterized by motor disturbances such as paralysis (monoplegia, paraplegia, or quadriplegia) or abnormal movements (tremors, choreiform, or gait disturbances) which often increase when attention is directed toward them. Examination reveals normal tone and reflexes.
Dissociative Convulsions (Pseudo-seizures or Hysterical Fits)
Characterized by convulsive movements and partial loss of consciousness. Differential diagnosis with true epileptic seizures is crucial (see table below).
Dissociative Sensory Loss and Anaesthesia
This involves sensory disturbances like hemianesthesia, blindness, deafness, and glove and stocking anesthesia (absence of sensations at wrists and ankles). The disturbance is usually based on the patient’s non-medical knowledge of the illness they are manifesting, and detailed examination shows no abnormalities.
Distinguishing Epileptic Seizures and Dissociative Convulsions
Clinical Point | Epileptic Seizures | Dissociative Convulsions |
|---|---|---|
Aura (Warning) | Usual | Unusual |
Attack Pattern | Stereotyped, known clinical pattern | Purposive body movements; absence of any established clinical pattern |
Tongue Bite | Present | Absent |
Incontinence | Can occur | Very rare |
Injury | Can occur | Very rare |
Duration | Usually about $30-70$ seconds | $20-800$ seconds (prolonged) |
Amnesia | Complete | Partial |
Time of Day | Anytime, can occur during sleep | Never occurs during sleep |
Place of Occurrence | Anywhere | Usually indoors or in a safe place |
Post-ictal Confusion | Present | Absent |
Neurological Signs | Present | Absent |
Dissociative Disorders
Definition
Dissociation is the separation of thoughts, feelings, or experiences from the normal stream of consciousness and memory. Dissociative disorders involve a disturbance in the organization of identity, memory, perception, or consciousness, often existing on a continuum experienced by individuals exposed to trauma.
Etiology
Trauma and Development
Dissociative disorders usually develop as a mechanism for coping with severe trauma. They most often form in children subjected to chronic physical, sexual, or emotional abuse, or an otherwise frightening and unpredictable home environment. Since personal identity is still forming during childhood, dissociation allows the child to step outside themselves and observe trauma as though it’s happening to a different person.
Types of Dissociative Disorder
1. Dissociative Amnesia
This is a sudden inability to recall important personal information, particularly concerning a traumatic or stressful life event. The memory loss is too great to be explained by ordinary forgetfulness.
Localized Amnesia: No memory of specific events that took place within a specific window of time (e.g., no memory of a car wreck itself).
Selective Amnesia: Recall of only small parts of events that took place in a defined period of time (e.g., recalling only some parts of an abusive series of events).
Generalized Amnesia: Patients cannot remember anything in their entire lifetime, including their own identity.
Continuous Amnesia: Patients have no memory of events up to and including the present time.
Systematized Amnesia: Loss of memory for a specific category of information (e.g., missing all memories about one specific family member).
2. Dissociative Fugue (Psychogenic Fugue)
This involves a sudden, unexpected travel away from home or the workplace, often with the assumption of a new identity and an inability to recall the past. The onset is sudden, often in the presence of severe stress. Following recovery, the patient has no recollection of the events that took place during the fugue. The course is typically brief (hours to days), but can last for months.
3. Dissociative Stupor
A rare condition in which patients are motionless and mute and do not respond to stimulation, yet they remain fully aware of their surroundings.
4. Ganser’s Syndrome
A rare condition characterized by four main features:
Giving ‘approximate answers’ to simple questions (e.g., answering $3 + 3 = 7$).
Psychogenic physical symptoms.
Hallucinations (usually visual and elaborate).
Apparent clouding of consciousness.
5. Dissociative Identity Disorder (DID) (Multiple Personality Disorder)
The person is dominated by two or more distinct personalities (called “alters”), of which only one is manifest at a time. Typically, one personality is not aware of the existence of the others. The transition from one personality to another is sudden, and the new behavior usually contrasts strikingly with the patient’s normal state.
6. Trance and Possession Disorders
This is common in various cultures and is characterized by a temporary loss of both the sense of personal identity and full awareness of the surroundings. When induced by religious rituals, the person may feel taken over by a deity or spirit.
Management and Interventions
Treatment Modalities
Treatment typically involves various forms of psychotherapy, as the role of drugs is limited unless managing comorbid anxiety or mood symptoms.
Psychotherapy:
Free Association
Hypnosis (to access repressed memories)
Abreaction Therapy (to relive and express intense emotions tied to a trauma)
Supportive Psychotherapy
Behavior Therapy (e.g., aversion therapy, operant conditioning)
Drug Therapy: Drugs have a limited role but may be used short-term (e.g., benzodiazepines) for anxiety.
Nursing Interventions
Rule Out Organic Pathology: Monitor physician’s assessments and lab reports to ensure there is no underlying medical condition.
Manage Disability Focus: Do not focus on the physical disability. Encourage the patient to perform self-care activities as independently as possible and only intervene when assistance is necessary.
Discourage Manipulation: Do not allow the patient to use the disability as a manipulative tool to avoid participating in therapeutic activities. Withdraw attention if the patient continues to overly focus on physical limitations.
Encourage Verbalization: Encourage the patient to verbalize fears and anxieties related to their conflicts.
Positive Reinforcement: Provide positive reinforcement for the patient when they identify or demonstrate alternative, adaptive coping strategies.
Goal Setting: Identify unresolved specific conflicts and assist the patient in setting realistic goals and identifying possible solutions for the future.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

