Skin Conditions
Subtopic:
Acne vulgaris

Acne vulgaris is a common inflammatory skin condition arising from alterations in the pilosebaceous units, the skin’s structures encompassing a hair follicle and its associated oil (sebaceous) gland.
The term “acne” originates from the Greek word “acme,” denoting a skin breakout or eruption.
This condition represents the most prevalent skin issue affecting teenagers and young adults. Individuals experiencing acne may suffer notable psychological distress, and in infrequent instances, mortality due to suicide has been reported.
The emotional impact of shame and worry can interfere with the social interactions and professional opportunities of those affected. Resulting scars can be permanent and disfiguring.
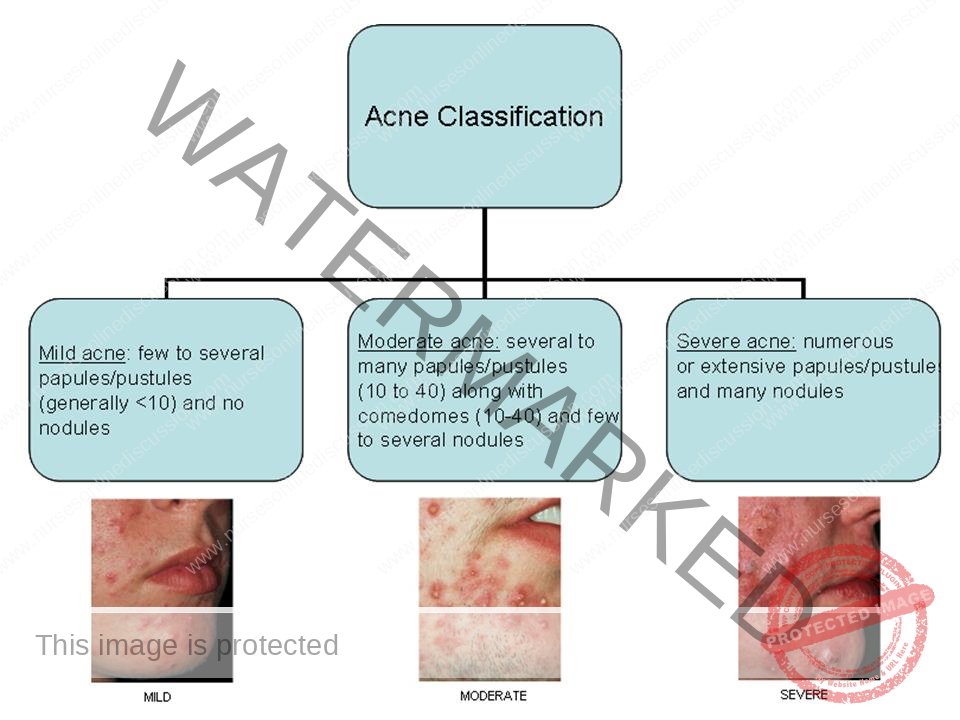
Classification of Acne
Acne vulgaris is categorized into mild, moderate, and severe forms.
Mild Acne: Characterized by non-inflamed lesions (comedones), a limited number of inflamed lesions (papules and pustules), or a combination of both.
Moderate Acne: Involves a greater number of inflamed lesions, occasional deeper, larger lesions (nodules), or both, and may present with mild scarring.
Severe Acne: Distinguished by extensive inflamed lesions, nodules, or both, accompanied by scarring. It can also refer to moderate acne unresponsive to six months of treatment or acne of any severity that significantly impacts psychological well-being.
Causes of Acne Vulgaris
Acne development is linked to an increased sensitivity of the sebaceous glands to normal levels of androgens (hormones), which is further exacerbated by the bacteria Cutibacterium acnes (P. acnes) and inflammation.
Contributing factors to acne include:
Infection with bacteria such as Cutibacterium acnes and Staphylococcus epidermidis.
Certain medications like lithium, corticosteroids, and anti-seizure drugs.
Excessive exposure to ultraviolet (UV) radiation from the sun.
The use of occlusive items like shoulder pads, headbands, backpacks, and tight undergarments.
Hormonal imbalances related to conditions such as polycystic ovary syndrome (PCOS) and pregnancy.
The buildup of dead skin cells within pores.
Medications containing halogens (like iodides, chlorides, bromides), lithium, barbiturates, or androgenic hormones.
Underlying medical conditions such as congenital adrenal hyperplasia, Cushing’s syndrome, and polycystic ovary syndrome.
Hormonal changes during puberty.
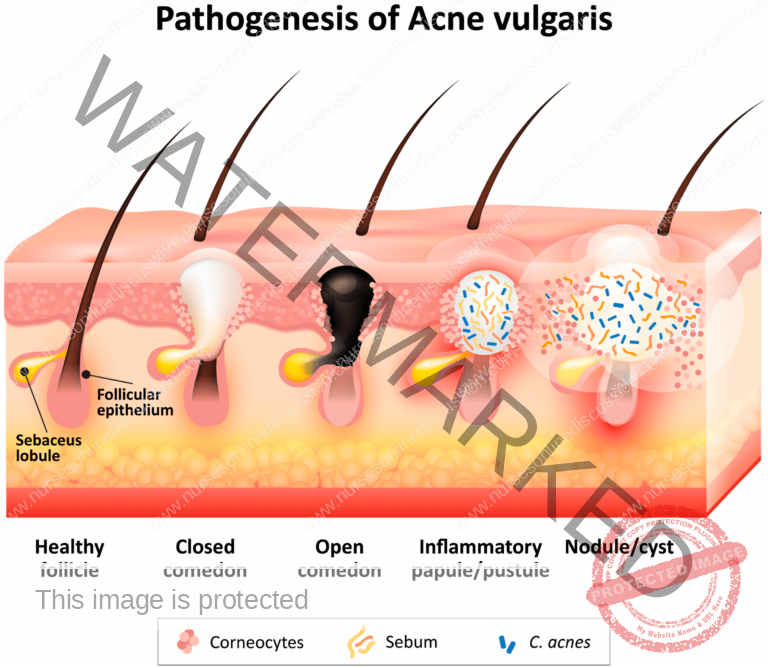
Pathophysiology of Acne
The development of acne involves four key factors:
Follicular hyperkeratinization: An excess buildup of keratin within the hair follicle, leading to pore blockage.
Increased sebum production: Elevated production of skin oil (sebum) by the sebaceous glands.
Presence of Cutibacterium acnes (P. acnes) in the follicle: This anaerobic bacterium, a normal inhabitant of the skin, contributes to inflammation.
Inflammation: The body’s response to the other factors, resulting in redness, swelling, and pain.
During puberty, hormonal changes, particularly an increase in androgens, stimulate sebum production. The enzyme 5-alpha reductase converts testosterone into dihydrotestosterone (DHT), a more potent androgen, which binds to receptors in sebaceous glands, further increasing sebum output. This, in turn, promotes the excessive growth of cells lining the hair follicle, leading to sebum retention.
When distended follicles rupture, they release pro-inflammatory substances into the surrounding skin (dermis), triggering inflammation. Cutibacterium acnes, Staphylococcus epidermidis, and the yeast Malassezia furfur can contribute to inflammation and further stimulate follicular cell proliferation.
Risk Factors
Hormonal Influence: Androgens stimulate the growth and secretory function of sebaceous glands.
External Factors:
Certain soaps and oil-based cosmetics.
Facial massage.
Certain detergents.
Repetitive friction or pressure can worsen acne by rupturing comedones, leading to inflammatory lesions. Patients should avoid touching or picking at their skin.
Occlusive clothing or gear like turtlenecks, bra straps, shoulder pads, orthopedic casts, and sports helmets can cause “acne mechanica” by blocking hair follicles.
Diet: Components in cow’s milk may potentially exacerbate acne in some individuals.
Family History: Having close relatives with acne increases the risk of developing the condition. The risk is more than threefold in individuals with affected first-degree relatives.
Stress: Psychological stress can worsen acne. Sebaceous glands contain receptors for corticotrophin-releasing hormone (CRH), a stress hormone. Severe anxiety and anger may aggravate acne due to the release of stress hormones.
Body Mass Index (BMI): A correlation exists between increasing BMI and a higher risk of acne in females.
Premenstrual Period: Acne flare-ups before menstruation are common in women, possibly due to fluid retention around the hair follicles, occurring in approximately 70% of female acne patients.
Signs and Symptoms of Acne
Acne vulgaris commonly affects areas with numerous, hormone-sensitive sebaceous glands, such as the face, neck, chest, upper back, and upper arms.
Typical acne lesions include:
Open comedones (blackheads)
Closed comedones (whiteheads)
Inflammatory lesions (papules, pustules, nodules, cysts)
Scarring can occur as a result of inflammatory lesions.
Post-inflammatory hyperpigmentation, dark marks on the skin, is common in individuals with darker skin tones and may persist for months without treatment.
Adult women may experience acne on the lower face and neck, often associated with premenstrual flare-ups.
Management of Acne Vulgaris
Aims of Treatment:
Reduce the population of acne-causing bacteria.
Decrease sebaceous gland activity and prevent pore blockage.
Reduce inflammation and treat any secondary infections.
Minimize scarring and identify/eliminate factors that worsen acne.
Medical Management:
Topical Pharmacologic Therapy:
Benzoyl peroxide (5%) applied twice daily.
Topical antibiotics, such as clindamycin (1% gel).
Systemic Pharmacologic Therapy:
Oral antibiotics, such as doxycycline (100 mg twice daily).
Oral retinoids (e.g., isotretinoin).
Hormone therapy, including oral contraceptives, may be beneficial for women by reducing androgen levels and subsequently decreasing sebum production.
Surgical Treatment:
Extraction of comedones.
Drainage of pustules and cysts.
Excision of sinus tracts and cysts.
Intralesional corticosteroid injections to reduce inflammation.
Cryotherapy (freezing) for certain lesions.
Dermabrasion to improve the appearance of scars.
Laser resurfacing for scar treatment.
Nursing Diagnoses
Impaired Skin Integrity
Deficient Knowledge
Disturbed Body Image
Nursing Management
Administer prescribed medications, which may include topical benzoyl peroxide (inform patients that initial redness and scaling are common but usually resolve), topical retinoids (vitamin A derivatives), and oral antibiotics like tetracycline.
Provide client and family education:
Advise that heat, humidity, and perspiration can worsen acne. Clarify that poor hygiene, diet, menstrual cycles, and other common myths are not direct causes of acne.
Explain that noticeable results from treatment typically take 4 to 6 weeks of consistent adherence to the prescribed regimen.
Instruct on gentle face washing (avoid scrubbing) with a mild cleanser twice daily.
Advise against squeezing blackheads, touching or rubbing the face, and emphasize the importance of daily hair washing and keeping hair off the face. Recommend cautious use of cosmetics, as some products can exacerbate acne.
Instruct female patients to inform their healthcare provider if they suspect they might be pregnant. Certain medications, such as systemic retinoids, can cause birth defects, necessitating pregnancy testing before starting treatment and the use of strict birth control measures during treatment.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

