Conditions Affecting the Endocrine System
Subtopic:
Addison’s disease
Table of Contents
Learning Objectives
Explain the pathophysiology of Addison’s Disease, including cortisol and mineralocorticoid deficiencies.
Identify primary and secondary causes, such as autoimmune reactions, infections, tumors, and pituitary dysfunction.
Recognize clinical manifestations, including hyperpigmentation, hypotension, electrolyte imbalance, and fatigue.
Describe diagnostic procedures, including cortisol and ACTH testing, stimulation tests, and adrenal antibody assays.
Outline medical management strategies, such as hormone replacement, fluid resuscitation, and infection control.
Implement nursing care interventions, focusing on cardiovascular monitoring, skin assessment, and fluid balance.
Addison’s disease
Addison’s disease is a clinical condition resulting from adrenocortical hormone deficiency due to primary disease of the adrenal glands or secondary to a pituitary gland disorder.
The primary causes are often unknown (idiopathic) or autoimmune, but it can also be triggered by tuberculosis infection of the adrenal glands, obstruction by an adrenal tumor, metastasis, or hemorrhage.
Pathophysiology
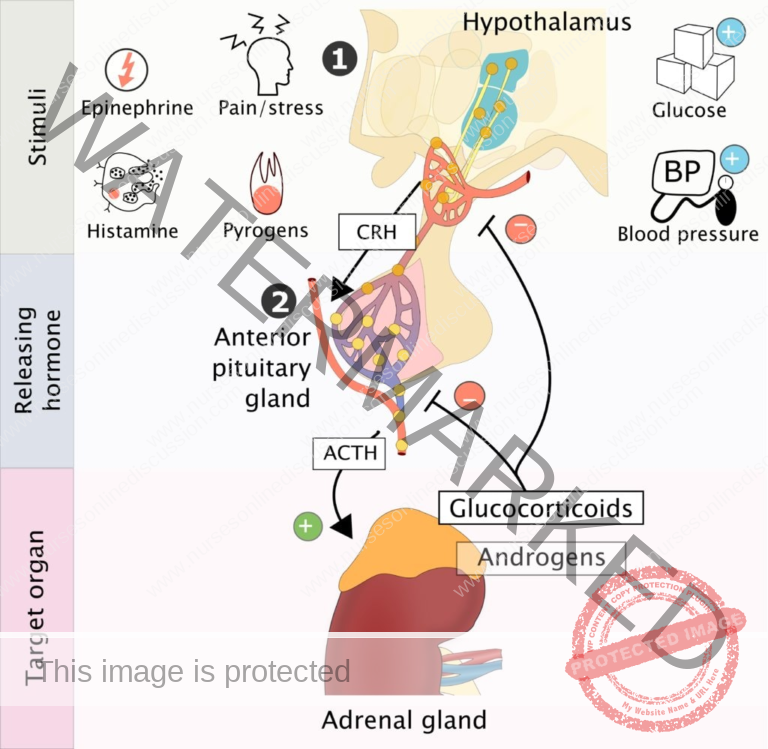
In Addison’s disease, the adrenal glands are unable to produce adequate amounts of cortisol and other steroid hormones. This is distinct from acute primary adrenocortical insufficiency, such as that seen in Waterhouse-Friderichsen syndrome.
Mineralocorticoid Deficiency: Mineralocorticoids regulate sodium reabsorption and potassium excretion. Their deficiency leads to increased sodium loss and decreased potassium excretion, primarily in urine, but also in sweat, saliva, and the gastrointestinal tract. This results in low serum sodium (hyponatremia) and high serum potassium (hyperkalemia). The resulting loss of salt and water leads to severe dehydration, increased concentration of solutes in the plasma (hypertonicity), acidosis, reduced blood volume, low blood pressure (hypotension), and potentially circulatory collapse. It’s important to note that in secondary adrenal insufficiency, where the problem lies in inadequate adrenocorticotropic hormone (ACTH) production by the pituitary, electrolyte imbalances may be less pronounced or even normal, and circulatory issues tend to be less severe.
Glucocorticoid Deficiency: A lack of glucocorticoids contributes to hypotension and causes increased sensitivity to insulin, disrupting the metabolism of carbohydrates, fats, and proteins. Without sufficient cortisol, the body’s ability to produce glucose from protein is impaired, leading to low blood sugar (hypoglycemia) and decreased liver glycogen stores. This results in weakness, partly due to impaired nerve and muscle function. The body’s ability to withstand stress from infection, trauma, and other stressors is also reduced. Weakened heart muscle and dehydration decrease cardiac output, potentially leading to circulatory failure.
The decreased cortisol levels stimulate increased production of ACTH by the pituitary gland and an increase in beta-lipotropin in the blood. Beta-lipotropin has melanocyte-stimulating activity and, along with ACTH, causes the characteristic hyperpigmentation of the skin and mucous membranes seen in Addison’s disease. Therefore, hyperpigmentation is typically absent in adrenal insufficiency caused by pituitary failure (secondary adrenal insufficiency).
Causes of Addison’s Disease (Can be Predisposing Factors Too)
Autoimmune Reaction: Addison’s Disease can develop when the body’s defense mechanism mistakenly attacks and damages the adrenal glands. This is an autoimmune response where the immune system identifies adrenal tissue as foreign, initiating an assault that diminishes hormone production. Antibodies targeting adrenal enzymes may be involved in this process.
Idiopathic Atrophy of the Adrenal Glands: In some instances, the adrenal glands might undergo atrophy, meaning they diminish in size and lose functionality without a definitively known cause. This condition is termed idiopathic adrenal atrophy. The underlying mechanism for this is often unclear.
Surgical Removal of Both Adrenal Glands: Addison’s Disease can result from the bilateral surgical removal of the adrenal glands. This procedure is generally considered as a treatment for conditions such as Cushing’s syndrome or growths affecting both adrenals. Following this, ongoing hormone replacement is essential for survival.
Adrenal Carcinoma: Adrenal carcinoma, a less frequent form of malignancy, originates within the adrenal glands. The cancerous growth can disrupt the typical functioning of these glands, causing adrenal insufficiency and Addison’s Disease. The tumor can physically replace functional adrenal tissue.
Infections such as TB: Certain infections, most notably tuberculosis (TB), can infiltrate and harm the adrenal glands. Damage resulting from TB can compromise the glands’ ability to synthesize hormones, leading to Addison’s Disease. Fungal infections and cytomegalovirus (CMV) can also be causative agents.
Abnormal/Malfunction of the Pituitary Gland: The pituitary gland is critical in regulating adrenal function by secreting adrenocorticotropic hormone (ACTH). If the pituitary gland doesn’t operate correctly and fails to produce adequate ACTH, the adrenal glands won’t receive the necessary signals for hormone synthesis, resulting in Addison’s Disease. This is frequently classified as secondary adrenal insufficiency.
Prolonged Use of Steroid Medication: Extended use of corticosteroid drugs, frequently prescribed for autoimmune conditions or inflammatory states, can suppress the pituitary gland’s secretion of ACTH. This can contribute to the shrinking of the adrenal glands and potentially trigger Addison’s Disease upon abrupt cessation.
Additional causes include:
Genetic Factors: While the majority of Addison’s Disease cases are not inherited, a rare genetic form exists, known as familial glucocorticoid deficiency (FGD). In FGD, specific gene mutations can lead to insufficient adrenal hormone production. Conditions like autoimmune polyglandular syndrome type 1 and 2 have genetic components that increase risk.
Hemorrhage into the Adrenal Glands: Significant bleeding into the adrenal glands, often due to injury or other medical issues like sepsis-related Waterhouse-Friderichsen syndrome, can injure the glands and impair their hormone production. Anticoagulant therapy can also be a contributing factor in some instances.
Amyloidosis: Amyloidosis is an uncommon condition where abnormal proteins (amyloids) deposit in various organs, including the adrenal glands. This accumulation can disrupt adrenal function and induce Addison’s Disease.
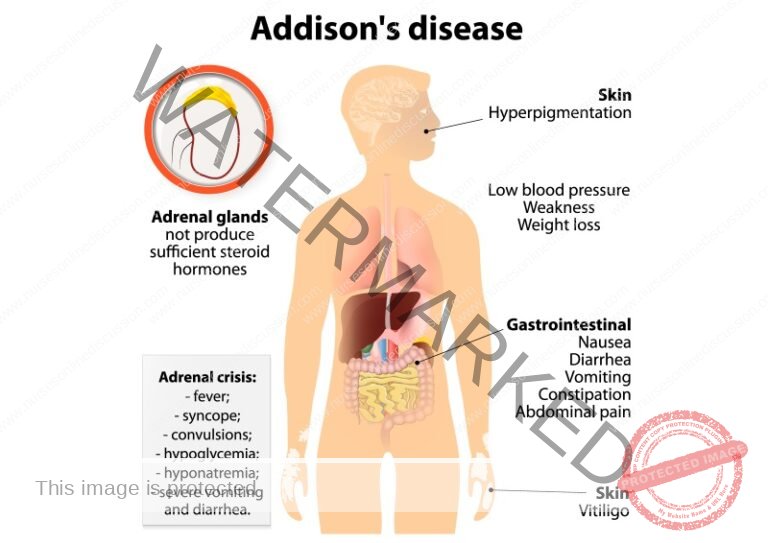
Clinical Presentation of Addison’s Disease
Clinical Presentation of Addison’s Disease:
Due to Cortisol Deficiency:
Addison’s Disease primarily results in a lack of cortisol, a fundamental hormone for numerous bodily functions. Common manifestations related to insufficient cortisol include:
Weakness: Individuals with Addison’s Disease commonly experience pronounced muscle weakness, making routine activities challenging.
Weight Loss: Unexplained reduction in body mass can occur due to alterations in metabolism.
Fatigue: Significant tiredness and exhaustion are characteristic, even with adequate sleep.
Nausea and Vomiting: Persistent feelings of sickness and throwing up may be present.
Diarrhea: Ongoing loose bowel movements can develop due to gastrointestinal disturbances. Abdominal discomfort or pain can also be experienced.
Due to Increased ACTH Production (If the Cause Is in the Adrenal Gland):
When Addison’s Disease originates from issues within the adrenal glands, it can stimulate increased secretion of adrenocorticotropic hormone (ACTH) as the body attempts to stimulate the failing glands.
Manifestations linked to elevated ACTH include:
Hyperpigmentation of Skin and Mucous Membranes: A distinctive sign is the darkening of the skin and mucous membranes, appearing as tan or bronze patches. This darkening is often more noticeable in skin folds, recent scars, and the lining of the mouth.
Due to Mineralocorticoid Deficiency:
Addison’s Disease can also lead to a deficiency of mineralocorticoids, particularly aldosterone, which is crucial for regulating electrolyte balance and maintaining blood pressure.
Manifestations associated with mineralocorticoid deficiency include:
Very Low Blood Pressure (Hypotension): The absence of sufficient aldosterone can cause notably low blood pressure, leading to dizziness, lightheadedness upon standing, and fainting episodes.
Electrolyte Imbalances: This presents as elevated potassium serum levels (hyperkalemia) and diminished levels of sodium (hyponatremia) and chloride in the bloodstream. Intense salt cravings may also be reported.
Due to Androgen Deficiency:
In some instances, Addison’s Disease can also cause a deficiency in androgens, which may lead to specific symptoms:
Sparse Hair in Females: Women with Addison’s Disease might notice thinning or loss of body hair, particularly in the pubic and axillary regions.
General Weakness: Physical exertion, exposure to cold temperatures, or acute infections can exacerbate the overall weakness and fatigue felt by individuals with Addison’s Disease. Muscle and joint aches may also be present.
Diagnosis of Addison’s Disease:
Hormone Levels Testing:
To diagnose Addison’s Disease, healthcare providers typically initiate assessment with hormone level measurement. The primary hormones assessed are cortisol and ACTH (Adrenocorticotropic hormone).
Morning and Evening Cortisol Levels: Blood samples are obtained in the early morning and later in the day to measure cortisol levels. In individuals with Addison’s Disease, both morning and evening cortisol levels are generally depressed. Salivary cortisol assays can also be utilized.
Plasma ACTH Level: Concurrently, the concentration of ACTH in the blood plasma is determined. The findings aid in differentiating between primary and secondary adrenal insufficiency.
Differentiating Primary and Secondary Adrenal Insufficiency:
In cases of primary adrenal insufficiency (due to issues intrinsic to the adrenal glands), ACTH levels are typically elevated, while cortisol levels are below the normal range.
In secondary adrenal insufficiency (arising from problems with the pituitary gland), both cortisol and ACTH levels are low or inappropriately normal.
ACTH Stimulation Test:
In some cases, an ACTH stimulation test might be performed for confirmation. During this test, a synthetic form of ACTH (cosyntropin) is administered, and blood cortisol levels are measured at baseline and at specific intervals after the injection.
A normal response to administered ACTH involves a significant increase in blood cortisol levels.
Individuals with Addison’s Disease often exhibit a diminished or absent rise in cortisol levels following ACTH administration. A prolonged ACTH stimulation test over several days may be indicated in certain situations.
Additional Blood Tests:
Blood glucose concentrations and electrolyte values are also evaluated. Addison’s Disease can lead to imbalances in blood electrolytes, such as decreased sodium and elevated potassium, which can contribute to symptoms like weakness and reduced blood pressure. Adrenal antibody testing may be performed to identify autoimmune etiology.
Complications of Addison’s Disease:
Renal Failure:
One potential complication of Addison’s Disease is renal failure, which signifies a loss of kidney function.
Addison’s Disease can disrupt the body’s electrolyte balance, particularly causing increased serum potassium concentrations. This imbalance can have detrimental effects on the kidneys.
Elevated potassium levels can induce abnormal heart rhythms (arrhythmias) and, in severe instances, compromise kidney function. Dehydration resulting from fluid losses can further contribute to renal issues.
Adrenal Hemorrhage:
Adrenal hemorrhage, although infrequent, is another complication that can arise in individuals with Addison’s Disease.
It involves bleeding within the adrenal glands, typically secondary to an adrenal crisis or significant physiological stress. This can manifest as sudden and severe abdominal or back pain.
Adrenal hemorrhage necessitates prompt medical intervention as it can be life-threatening.
Addisonian Crisis:
An Addisonian crisis, also termed acute adrenal insufficiency, is a critical and potentially fatal complication of Addison’s Disease.
It occurs when the adrenal glands fail to produce sufficient cortisol to meet the body’s demands, frequently precipitated by stressors such as infection, trauma, surgical procedures, or the sudden cessation of corticosteroid therapy.
Symptoms of an Addisonian crisis can encompass profound weakness, confusion, significant hypotension, rapid heartbeat, intense abdominal pain, severe nausea and vomiting, and potentially loss of consciousness.
Immediate emergency medical management is vital to stabilize the patient, typically involving intravenous administration of hydrocortisone and intravenous fluids.
4. Depression:
Chronic illnesses like Addison’s Disease can lead to emotional and psychological challenges, including depression.
Coping with the demands of managing a chronic condition, along with the physical symptoms and potential complications, can take a toll on a person’s mental health. It is essential for individuals with Addison’s Disease to receive comprehensive care that includes addressing emotional well-being and providing support for mental health issues such as depression.
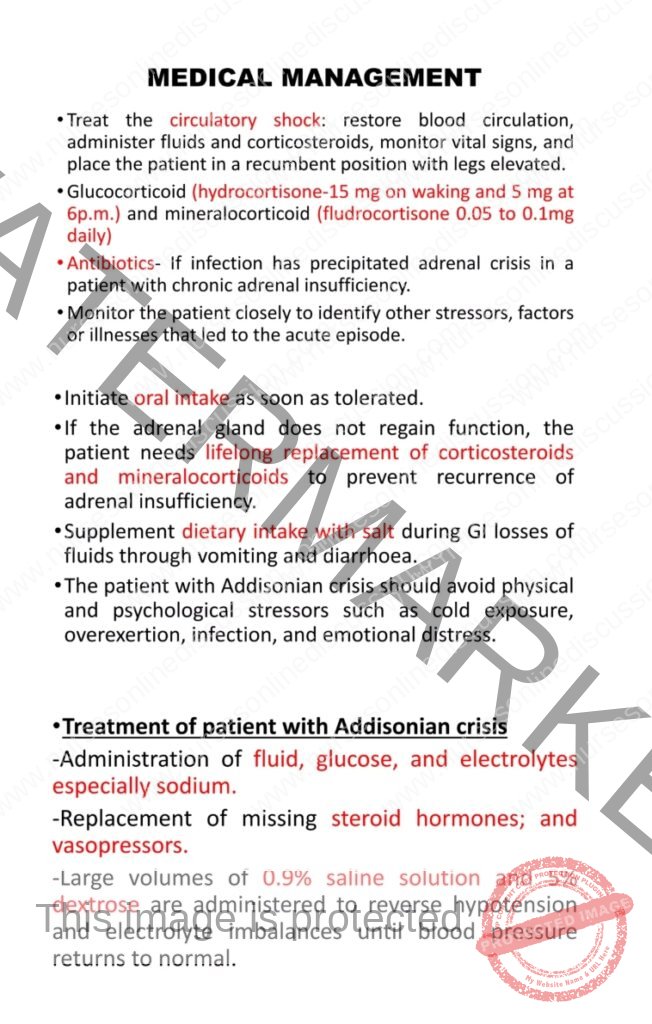
Medical Management
Restore Blood Circulation: Intravenous fluid administration with isotonic saline (NS) and dextrose solutions is initiated to address hypovolemia and hypoglycemia.
Mineralocorticoid Support: Fludrocortisone is typically prescribed in small daily doses, ranging from 0.05 to 0.1 mg, to help regulate blood pressure and electrolyte balance, particularly sodium and potassium.
Glucocorticoid Replacement: Daily hormone replacement therapy with a glucocorticoid, such as prednisolone, is crucial. A common regimen involves divided doses, for example, 15-25mg in the morning and 5-10mg in the evening to mimic the natural diurnal rhythm of cortisol secretion. Hydrocortisone can also be used, typically given in 2-3 divided doses daily.
Support for Hypotension: If low blood pressure persists despite fluid resuscitation and mineralocorticoid therapy, vasopressor agents like norepinephrine or dopamine may be necessary.
Address Precipitating Factors: If an infection is identified as the trigger for the adrenal crisis, appropriate antibiotic therapy should be administered promptly.
Long-Term Hormone Therapy: Lifelong replacement of both glucocorticoids and mineralocorticoids is required to manage adrenal insufficiency. Regular monitoring and dose adjustments may be necessary.
Sodium Supplementation: Oral rehydration solutions (ORS) can be used for sodium replenishment. Patients may also need to increase their dietary salt intake, especially during periods of increased sweating or activity.
Treat Underlying Etiology: The underlying cause of Addison’s disease needs to be addressed, such as initiating anti-tubercular treatment for TB-induced adrenal insufficiency.
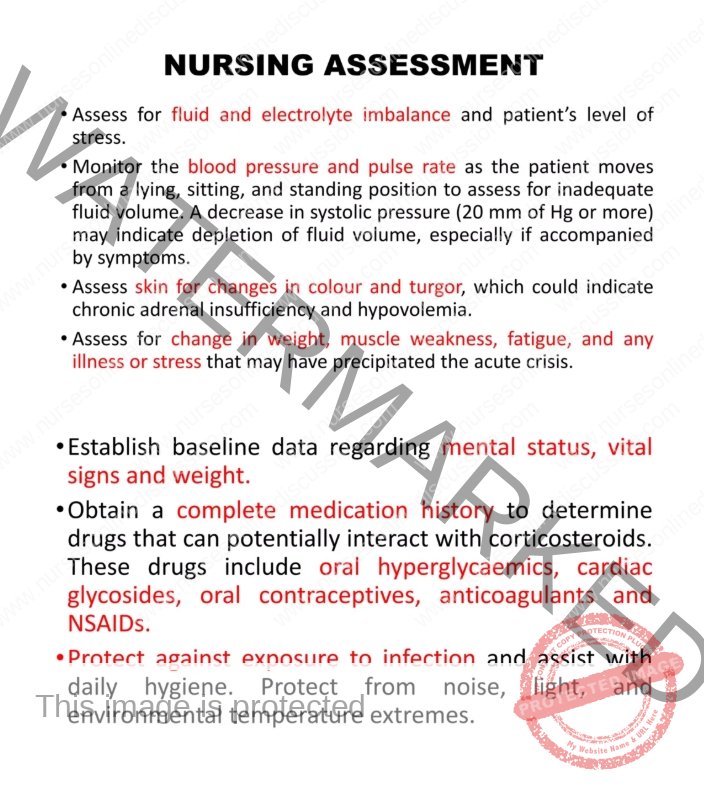
Nursing Care
Cardiovascular Monitoring: Closely monitor blood pressure and pulse rate, particularly when the patient changes position (lying, sitting, standing), to detect orthostatic hypotension indicative of inadequate fluid volume.
Skin Assessment: Regularly assess skin color for hyperpigmentation and evaluate skin turgor to determine hydration status. Note any areas of vitiligo that may be associated with autoimmune Addison’s.
History and Symptom Review: Obtain a detailed history of weight fluctuations, reports of muscle weakness, and experienced fatigue levels.
Identify Triggers: Inquire with the patient and their family about the onset of current symptoms or recent increases in physical or emotional stress that may have contributed to the adrenal crisis. Document any recent illnesses or injuries.
Nursing Diagnosis
Electrolyte Imbalance: Characterized by laboratory findings of hyponatremia, along with subjective reports of salt cravings and objective findings of vomiting and diarrhea.
Ineffective Tissue Perfusion: Related to alterations in skin pigmentation, specifically hyperpigmentation observed as skin tanning or bronzing. Assess for pallor, cyanosis, and delayed capillary refill as well.
Risk for Deficient Fluid Volume: Potentially related to excessive fluid loss through vomiting and diarrhea. Monitor for signs of dehydration such as dry mucous membranes, decreased urine output, and increased heart rate.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Medical Conditions Affecting the Endocrine System
- Applied Anatomy and Physiology of the Endocrine System
- Acromegaly/Gigantism (Hyperpituitarism)
- Dwarfism (Panhypopituitarism)
- Addison’s Disease (Adrenal Insufficiency)
- Pheochromocytoma
- Cushing’s Syndrome
- Hyperaldosteronism
- Thyrotoxicosis
- Diabetes Mellitus
Conditions Affecting the Nervous System
- Applied Anatomy and Physiology of the Nervous System
- Trigeminal Neuralgia
- Bell’s Palsy
- Parkinson’s Disease
- Spinal Cord Compression
- Transverse Myelitis
Medical Diseases Affecting the Renal System
- Anatomy and Physiology of the Renal System
- Renal Disorders
- Urinary Tract Infections (UTIs)
- Cystitis
- Renal Failure (Acute and Chronic)Nephrotic Syndrome
- Polycystic Kidney Disease (PKD)
- Kidney Stones (Nephrolithiasis)
Conditions of the Lymphatic System
- Anatomy and Physiology of the Lymphatic System
- Lymphedema
- Lymphangitis and Lymphadenitis
- Hodgkin’s Disease
Conditions of the Musculo-Skeletal System
- Anatomy and Physiology of the Musculo-Skeletal System
- Tendonitis
- Rheumatoid Arthritis
- Osteoarthritis
- Gout
- Bursitis
- Ankylosing Spondylitis
- Osteoporosis
- Paget’s Disease
Skin Conditions (Dermatology)
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

