Medical Nursing (III)
Subtopic:
Arthritis
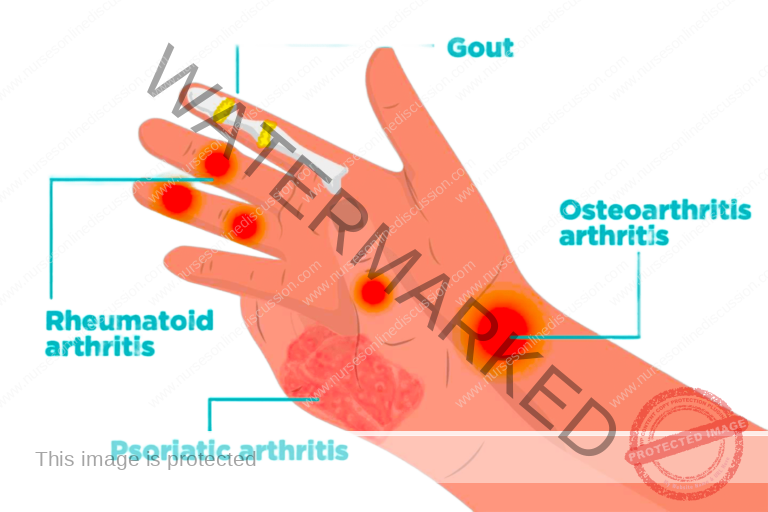
Arthritis refers to the experience of swelling and tenderness within one or multiple joints of the body.
Within the broad spectrum of arthritis, inflammatory arthritis encompasses numerous conditions where the primary characteristic is inflammation of the synovium, the lining of the joints. This category includes conditions arising after viral infections, rheumatoid arthritis, forms of arthritis associated with negative serological tests (seronegative spondyloarthropathy), and arthritis related to Lyme disease.
Conditions manifesting as inflammation in a single joint (inflammatory monoarthritis) can include arthritis caused by crystal deposits, such as gout and pseudogout, as well as septic arthritis (arthritis due to infection) and arthritis resulting from tumors located near joints.
Conversely, conditions characterized by inflammation in multiple joints (inflammatory polyarthritis) include rheumatoid arthritis, reactive arthritis, and seronegative arthritis that occurs in conjunction with psoriasis.
Categorization of Arthritis:
Rheumatoid Arthritis
Osteoarthritis
Gouty Arthritis
Arthritis Following Trauma
Arthritis Due to Infection
Arthritis Associated with Hemophilia
Arthritis Caused by Gonorrhea
Arthritis Related to Syphilis
Arthritis Caused by Tuberculosis
Underlying Causes of Arthritis:
Physical Injury or Trauma
Infectious Agents, such as staphylococcal and streptococcal bacteria
Tuberculosis Affecting Areas Outside the Lungs
Late-Stage Syphilis Infection
Deposition of Urate Crystals in Disorders of Uric Acid Metabolism (Gout)
Reactions Following Certain Infections
Breakdown or Deterioration of Joint Components, Particularly Cartilage
Autoimmune Reactions, as seen in Rheumatic Fever
Bleeding into the Joint Space
Factors That May Increase Susceptibility:
Sex: Women prior to menopause experience a higher incidence compared to men.
Family History: A positive family history of arthritis.
Genetic Predisposition: Inherited genetic factors.
Advancing Age: Increased risk with older age.
Kidney Dysfunction: Presence of renal failure.
Rheumatoid Arthritis: A Closer Look
Rheumatoid arthritis is an autoimmune disorder characterized by inflammation, with an unknown origin, that primarily affects the synovial membrane lining the joints.
It is a long-lasting inflammatory condition affecting the joints, distinguished by persistent, symmetrical involvement of smaller joints on both sides of the body. This process leads to the destruction of cartilage and erosion of bone, eventually causing joint deformities.
The impact of this disease extends beyond the joints, affecting various articular and non-articular structures throughout the body.
Rheumatoid arthritis is classified as seropositive in the majority of cases (around 80%) due to the presence of rheumatoid factor in the blood.
The field of rheumatology focuses on a diverse group of disorders affecting the joints, bones, and connective tissues.
Rheumatic conditions can affect individuals of all genders, ethnicities, and ages. The likelihood of experiencing these conditions increases with age, with a significant proportion of individuals over 50 reporting rheumatic complaints.
The Progression of Rheumatoid Arthritis:
Rheumatoid arthritis arises from an autoimmune response where the body’s defense system mistakenly attacks its own tissues. The precise trigger remains unidentified. The disease process primarily targets the synovium, leading to two key pathological changes: inflammation and the abnormal growth of tissue.
The joints become intensely inflamed due to these inflammatory changes within the synovial membrane. The synovium thickens, develops increased blood vessel presence, and becomes infiltrated with immune cells. This can lead to fluid accumulation within the joint, manifesting as a swollen, tender, and painful joint with restricted movement. Outside the joint, this process can lead to the formation of rheumatoid nodules, which are lumps under the skin.
The proliferating synovial tissue, known as pannus, spreads over the articular cartilage, gradually causing its erosion.
Systemic inflammation can impact various organs, potentially leading to inflammation of the sac around the heart (pericarditis), the lining of the lungs (pleuritis), inflammation of blood vessels in the intestines (bowel vasculitis), as well as general feelings of illness and anemia.
In children under 16, the condition is known as juvenile rheumatoid arthritis or Still’s disease. It can present with arthritis affecting multiple joints, causing the child to assume a flexed posture, reluctance to be active, swollen lymph nodes, enlarged liver and spleen, and inflammation of the heart and lung linings.
Pathophysiology Summarized:
The progression of rheumatoid arthritis can be succinctly described as follows:
Autoimmune Response: The primary event in RA is an autoimmune reaction focused on the synovial tissue.
Enzyme Release: Immune cell activity releases enzymes within the joint.
Collagen Breakdown: These enzymes degrade collagen, leading to swelling, proliferation of the synovial lining, and the eventual formation of pannus.
Structural Damage: The pannus invades and destroys cartilage and erodes the underlying bone.
Functional Consequences: This destruction results in the loss of joint surfaces and impaired joint motion.
Muscle and Tissue Changes: Muscle fibers undergo degenerative changes, and the elasticity and contractile strength of tendons and ligaments diminish.
Recognizing the Signs and Symptoms:
Joint Pain: A hallmark symptom, characterized by difficulty in moving affected joints.
Swelling: Leads to limitations in joint function.
Warmth: Increased temperature is felt in the affected joint, which may feel spongy upon palpation.
Redness: Erythema over the affected area indicates inflammation.
Functional Limitations: Pain restricts the ability to use the affected area.
Joint Deformities: Misalignment due to swelling can result in deformities of the hands and feet.
Rheumatoid Nodules: Non-tender, movable lumps under the skin may appear in more advanced cases.
Gradual Onset of Pain and Morning Stiffness: Pain and stiffness that are worse in the morning.
Appetite and Weight Changes: Loss of appetite and subsequent weight loss.
Progressive Loss of Joint Function: Worsening swelling and reduced ability to use the joints.
Mild Fever and Fatigue: Low-grade fever and persistent tiredness.
Initial Vague Symptoms: Early, non-specific symptoms like loss of appetite, weakness, and joint aches that can persist for weeks or months before more specific symptoms arise.
Inflammation in Multiple Joints: Typically affecting three or more joints, including the smaller joints.
Symmetrical Arthritis: Bilateral involvement of joints, such as ankles, knees, wrists, elbows, shoulders, spine, and jaw joints.
Pain Exacerbated by Movement: Joint pain increases with movement and can disrupt sleep.
Subcutaneous Nodules: Lumps under the skin.
Extra-Articular Manifestations: Involvement of other organs, including enlarged spleen, swollen lymph nodes, inflammation around the heart, carpal tunnel syndrome, nerve damage, ulcers, decreased blood cell counts, and kidney issues.
Red, Spongy Joints: Inflamed joints that feel soft upon palpation.
Triggers: The condition can be triggered by stress, emotional factors, infections, and physical overexertion.
Relapsing and Remitting Course: Characterized by periods of symptom flare-ups (relapses) and periods of improvement (remissions).
Hemorrhagic Changes: Small areas of bleeding in the nails and fingertips.
Eye Inflammation: Inflammation and ulceration of the sclera (white part of the eye).
Cervical Spine Involvement: Inflammation in the upper spine potentially leading to compression of the spinal cord.
Assessment and Diagnostic Procedures:
Physical Examination: A thorough evaluation by a healthcare provider.
Medical History Review: Gathering information about the patient’s symptoms and medical background.
X-rays of Affected Joints: Can reveal swelling in soft tissues, erosion of joint surfaces, and thinning of bone near the joint in early stages, progressing to cyst formation in the bone.
Rheumatoid Factor (RF) Test: Positive in a significant majority of cases (often assessed using the Rose-Waaler test).
Synovial Membrane Biopsy: Microscopic examination of the joint lining to identify inflammatory changes and the presence of pannus.
Synovial Fluid Analysis: Examination of fluid aspirated from the joint, which may show an increased volume, and appear opaque, cloudy, or yellow due to inflammation, bleeding, and cellular debris.
Erythrocyte Sedimentation Rate (ESR): Typically significantly elevated, indicating inflammation. May return to normal as symptoms improve.
Complete Blood Count (CBC): Often reveals a moderate decrease in red blood cells (anemia). White blood cell count may be elevated during active inflammation.
Immunoglobulin (Ig) Levels (IgM and IgG): Elevated levels strongly suggest an autoimmune process as the cause of rheumatoid arthritis.
Direct Arthroscopy: Visual examination of the joint using a small camera to identify bone irregularities and joint degeneration.
Goals of Rheumatoid Arthritis Management:
Pain Control
Prevention of Joint Damage
Management of Systemic Symptoms
Achieving Disease Remission (Stopping Inflammation)
Enhancement of Physical Function and Overall Well-being
Reduction of Long-Term Complications
Symptom Relief
It is important to note that there is currently no definitive cure for rheumatoid arthritis.
Nursing Interventions:
Ensure adequate rest for painful, swollen joints, especially during acute flare-ups. Employ a bed cradle to keep bedding off affected joints.
Utilize firm back support during the day.
Maintain legs in a straight position, avoiding pillow placement behind the knees to prevent flexion contractures.
Encourage active exercises under the guidance of a physical therapist.
Provide a diet rich in protein, including ample milk and eggs.
Administer iron supplements to address the common issue of anemia.
Consider Vitamin D and calcium supplements to help mitigate osteoporosis risk.
Support and immobilize affected joints using light plastic splints or even plaster casts.
Alleviate pain and discomfort through comfort measures like heat or cold application, massage, and proper positioning with supportive pillows.
Encourage patients to express their pain. Administer prescribed anti-inflammatory and analgesic medications.
Facilitating Self-Care: Assist the patient in identifying areas where they experience difficulties with self-care. Develop a care plan based on their perceptions and priorities.
Improving Body Image and Coping Skills: Discuss how the disease impacts their life and address their concerns. Create a strategy for managing symptoms and build a support network with family and friends to promote daily function.
Increasing Mobility: Assess the need for consultations with occupational or physical therapists. Encourage independent movement while providing assistance as needed.
Reducing Fatigue: Promote adherence to treatment plans. Encourage proper nutrition and teach energy conservation techniques such as delegation and prioritizing tasks.
Promoting Home and Community-Based Care: Focus on educating the patient about their condition, potential disease-related changes, prescribed medications and their side effects, and strategies for maintaining independence and safety at home.
Medical Treatment Strategies:
While a definitive cure remains elusive, recent advances suggest that achieving remission is more likely with early and aggressive treatment using disease-modifying antirheumatic drugs (DMARDs). The specific medications prescribed will depend on the severity of symptoms and the duration of the condition.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These medications can reduce pain and inflammation. Over-the-counter options include ibuprofen and naproxen sodium. Prescription-strength NSAIDs are also available. Common NSAIDs used include aspirin, indomethacin, naproxen, diclofenac, and piroxicam. Side effects can include tinnitus, stomach irritation, cardiovascular issues, and potential liver and kidney damage.
Corticosteroids (Steroids): Medications like prednisone effectively reduce inflammation and pain and can slow joint damage. However, long-term use can lead to side effects such as bone thinning, weight gain, and diabetes. They are often used for short-term relief of acute symptoms with a plan for gradual dose reduction.
Disease-Modifying Antirheumatic Drugs (DMARDs): These drugs can slow the progression of rheumatoid arthritis and protect joints and other tissues from permanent damage. Common DMARDs include methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine. Side effects vary but may include liver damage, bone marrow suppression, and serious lung infections.
Biologic Agents (Biologic Response Modifiers): This newer class of DMARDs targets specific parts of the immune system that trigger inflammation. Examples include abatacept, adalimumab, anakinra, certolizumab, etanercept, golimumab, infliximab, rituximab, tocilizumab, and tofacitinib. While effective, they can increase the risk of infections. Biologic DMARDs are often used in combination with non-biologic DMARDs like methotrexate for enhanced effectiveness.
Surgical Interventions:
If medication is insufficient to prevent or slow joint damage, surgery may be considered to repair affected joints, improve function, reduce pain, and correct deformities. Surgical options include:
Synovectomy: Removal of the inflamed synovial lining of the joint, applicable to knees, elbows, wrists, fingers, and hips.
Tendon Repair: Addressing loosened or ruptured tendons around the joint due to inflammation and damage.
Joint Fusion (Arthrodesis): Surgically joining bones to stabilize or realign a joint and alleviate pain when joint replacement isn’t feasible.
Total Joint Replacement (Arthroplasty): Replacing damaged parts of the joint with a prosthesis made of metal and plastic.
Osteotomy: Cutting and reshaping bone to relieve pressure or improve alignment.
Tenorrhaphy: Surgically suturing a tendon.
Conservative Management Strategies:
Weight Reduction
Joint Rest
Avoiding Overuse of Affected Joints
Utilizing Orthotic Devices (Braces and Splints) to Support Inflamed Joints
Performing Isometric, Postural, and Aerobic Exercises
Seeking Occupational and Physical Therapy
Common Nursing Diagnoses:
Acute and Chronic Pain related to inflammation and increased disease activity, tissue damage, fatigue, or lowered pain tolerance.
Fatigue related to increased disease activity, pain, inadequate sleep/rest, insufficient nutrition, and emotional stress/depression.
Impaired Physical Mobility related to decreased range of motion, muscle weakness, pain on movement, limited endurance, and the lack of or improper use of assistive devices.
Self-Care Deficit related to contractures, fatigue, or loss of motion.
Disturbed Body Image related to physical and psychological changes and the dependency imposed by a chronic illness.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

