Conditions Affecting the Endocrine System
Subtopic:
Cushing's Syndrome
Table of Contents
Learning Objectives
Explain the pathophysiology of Cushing’s Syndrome, including cortisol overproduction and its hormonal regulation.
Identify common causes, such as pituitary tumors, adrenal hyperplasia, and prolonged corticosteroid use.
Recognize clinical manifestations, including moon face, truncal obesity, hypertension, and mood changes.
Describe diagnostic procedures, like dexamethasone suppression tests, ACTH assays, and imaging studies.
Outline treatment options, including surgical interventions, hormone replacement, and adrenal enzyme inhibitors.
Implement nursing care strategies, focusing on skin integrity, fluid balance, mental status, and patient education.
Cushing’s Syndrome
- Cushing’s syndrome arises when the body is exposed to an abnormally high level of cortisol for an extended period. This excess cortisol can be due to several factors. One common cause is the overproduction of adrenocorticotropic hormone (ACTH). This overproduction can stem from tumors in the pituitary gland or from non-cancerous growths (adenomas) or an abnormal increase in the size of the adrenal glands (nodular hyperplasia).
- Alternatively, Cushing’s syndrome can be defined as a hormonal disorder resulting from an overproduction of corticosteroids by the adrenal glands themselves or by the pituitary gland’s influence on the adrenal glands. Furthermore, prolonged use of corticosteroid medications can also lead to this syndrome.
Causes of Cushing’s Syndrome
Prolonged Use of Corticosteroid Medications: Taking corticosteroid medications, such as prednisone, for extended periods is a significant cause of Cushing’s syndrome. These medications are often prescribed to treat inflammatory conditions or suppress the immune system.
Hyperplasia of the Adrenal Gland: This refers to the enlargement of the adrenal glands, which can lead to the production of excess cortisol.
Tumor in the Pituitary Gland Enhancing Overproduction of ACTH: The pituitary gland, located at the base of the brain, produces ACTH, which signals the adrenal glands to release cortisol. A tumor in the pituitary can cause it to overproduce ACTH, leading to excessive cortisol production. This specific form of Cushing’s syndrome is often referred to as Cushing’s disease.
Tumor in One of the Adrenal Glands Above the Kidneys: A tumor in one of the adrenal glands can directly cause the gland to produce too much cortisol, independent of ACTH levels.
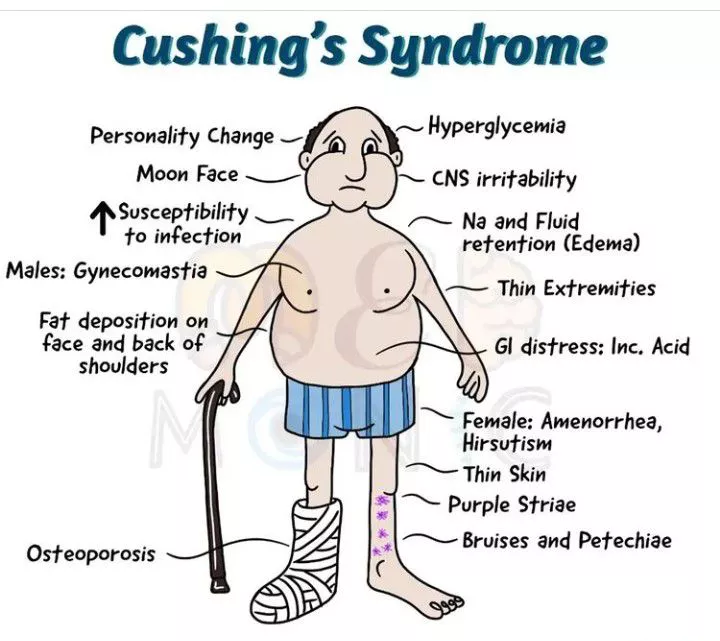
Clinical Presentation of Cushing’s Syndrome
The signs and symptoms of Cushing’s syndrome can vary from person to person but often include:
Hirsutism: Excessive hair growth in women in places where it typically doesn’t occur, such as the face, chest, and back.
Amenorrhea: The absence of menstruation in women of reproductive age.
Easy Bruising and Acne: The skin may become thinner and more fragile, leading to easy bruising. Acne is also a common skin manifestation.
Osteoporosis: The bones can become weakened and brittle due to the effects of excess cortisol, increasing the risk of fractures.
Cataracts and Glaucoma: Individuals with Cushing’s syndrome have an increased risk of developing these eye conditions.
Hypertension and Heart Failure: High blood pressure (hypertension) is common, and over time, the strain on the heart can lead to heart failure.
Truncal Obesity, Moon Face, Buffalo Hump: A characteristic pattern of weight gain occurs, with increased fat around the abdomen (truncal obesity), a rounded face (moon face), and a collection of fat on the upper back and base of the neck (buffalo hump).
Sodium Retention, Hypokalemia, Hyperglycemia: The body may retain excess sodium, leading to fluid retention. Low potassium levels (hypokalemia) and high blood sugar levels (hyperglycemia) are also frequently observed.
Negative Nitrogen Balance and Altered Calcium Metabolism: The body may break down more protein than it builds (negative nitrogen balance). Calcium metabolism is also affected, which contributes to bone weakening.
Decreased Inflammatory Responses, Impaired Wound Healing, Increased Susceptibility to Infections: Cortisol can suppress the immune system, leading to a reduced ability to fight off infections and slower wound healing.
Peptic Ulcers and Pancreatitis: There is an increased risk of developing ulcers in the stomach or duodenum (peptic ulcers) and inflammation of the pancreas (pancreatitis).
Thinning of Skin, Striae, Acne: The skin can become thin and fragile, leading to the formation of purple or pink stretch marks (striae), particularly on the abdomen, thighs, and arms. Acne is also a common skin problem.
Mood Alterations: Individuals with Cushing’s syndrome may experience a range of mood changes, including irritability, anxiety, and emotional lability.
Depression: Depression is a significant psychological symptom associated with Cushing’s syndrome.
Diagnosis
Diagnosing Cushing’s syndrome involves several tests:
Overnight Dexamethasone Suppression Test: This is a frequently used screening test. Dexamethasone, a synthetic corticosteroid, is administered, typically around 11 pm. The next morning, around 8 am, the level of cortisol in the blood is measured. In individuals with normal adrenal function, dexamethasone should suppress cortisol production.
Suppression of Cortisol: If the cortisol level is suppressed to less than 5 micrograms per deciliter (mcg/dL), it generally indicates normal functioning of the adrenal glands.
Measurement of Plasma ACTH (Radioimmunoassay) in Conjunction with Dexamethasone Suppression Test: Measuring ACTH levels alongside the dexamethasone suppression test helps to determine the underlying cause of Cushing’s syndrome. It can differentiate between a pituitary source (Cushing’s disease) where ACTH levels might be elevated or inappropriately normal, and other causes like adrenal tumors or ectopic ACTH production, where ACTH levels might be low or very high, respectively.
MRI, CT, and CT Scans: Imaging techniques such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are used to visualize the pituitary and adrenal glands to detect the presence of tumors or other abnormalities.
Management
The treatment strategy for Cushing’s syndrome depends on the underlying cause:
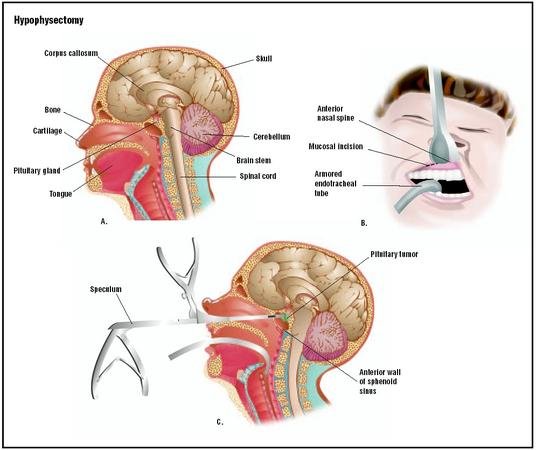
If Pituitary Source: For Cushing’s disease caused by a pituitary tumor, the primary treatment is often transsphenoidal hypophysectomy. This is a surgical procedure performed to remove the pituitary tumor, typically through the nasal passages.
Radiation of Pituitary: Radiation therapy to the pituitary gland may be considered if surgery is not feasible or if the tumor recurs after surgery.
Adrenalectomy: In cases where Cushing’s syndrome is caused by a tumor or hyperplasia of one or both adrenal glands, adrenalectomy, the surgical removal of one or both adrenal glands, may be necessary.
Temporary Replacement Therapy with Hydrocortisone or Florinef: Following surgery, particularly after bilateral adrenalectomy or hypophysectomy, the body may not produce enough cortisol. Therefore, temporary hormone replacement therapy with medications like hydrocortisone (a synthetic cortisol) or Florinef (fludrocortisone, a synthetic mineralocorticoid) may be needed to replace the hormones the body is no longer producing.
Adrenal Enzyme Reducers: If the source of excess cortisol is ectopic (meaning it’s produced by a tumor outside of the pituitary or adrenal glands) and inoperable, medications that reduce the production of cortisol by the adrenal glands may be used. Examples of these adrenal enzyme inhibitors include ketoconazole, mitotane, and metyrapone.
If Cause is Related to Excessive Steroid Therapy: If Cushing’s syndrome is due to the long-term use of corticosteroid medications, the appropriate management involves gradually tapering the dosage of the steroid down to the minimum effective dose necessary to manage the underlying condition. Abruptly stopping steroid medication can be dangerous.
Hypophysectomy
This surgical procedure involves the removal of the pituitary gland. Nurses play a crucial role in the care of patients undergoing this procedure.
Nursing Care
Assess the patient’s current activity level and their ability to perform daily routines and personal care tasks. This helps establish a baseline and identify areas where assistance may be needed.
Closely observe the patient’s skin for any signs of injury, infection, breakdown, bruising, or swelling (edema). Post-operative patients can be vulnerable to skin issues.
Note any changes in the patient’s appearance and their emotional response to these changes. Family members can provide valuable insights into the patient’s pre-operative emotional state and any noticeable shifts.
Regularly evaluate the patient’s mental status, paying attention to alertness, orientation, and cognitive abilities. This is important for detecting any neurological complications.
Nursing Diagnosis
Acute pain related to potential vertebral compression fractures, as indicated by reports of back pain. This pain can arise from the physiological effects of the underlying condition.
Self-care deficit linked to generalized weakness and fatigue, observed through signs like appearing tired and difficulty responding to questions. These symptoms can significantly impact a patient’s ability to care for themselves.
Risk for fluid overload due to the body’s potential to retain water and sodium because of elevated cortisol and mineralocorticoid levels. This hormonal imbalance disrupts normal fluid regulation.
Risk for injury associated with factors such as decreased bone density, generalized fatigue, fragile capillaries, and impaired wound healing. These physiological changes increase the susceptibility to physical harm.
Risk for infection connected to possible alterations in protein metabolism, elevated serum cortisol levels, or a compromised immune response. These factors can weaken the body’s defenses against pathogens.
Knowledge deficit regarding Cushing’s syndrome, evidenced by frequent hospital readmissions for related issues, repeated questions, or stated misunderstandings about the condition. This highlights the need for patient education.
Disturbed body image related to changes in fat distribution and fluid retention, resulting in characteristic features like a rounded face (moon face), fat accumulation on the upper back (buffalo hump), and increased abdominal fat, potentially leading to the patient using clothing to conceal these changes.
Disturbed thought processes linked to chemical imbalances in the brain caused by high cortisol levels, potentially manifesting as anxiety, irritability, or depression. These emotional and psychological changes are a direct consequence of the hormonal imbalance.
Evaluations
The patient will demonstrate a reduced risk of injury through preventive measures and interventions.
The patient will exhibit a decreased risk of infection by adhering to hygiene protocols and demonstrating no signs of infection.
The patient will actively participate in self-care activities to the best of their ability, showing improvement over time.
The patient will maintain or achieve intact skin without evidence of breakdown or injury.
The patient will express an improved perception of their body and demonstrate positive coping mechanisms.
The patient will exhibit improved mental clarity, appropriate affect, and coherent thought processes.
The patient will experience no significant complications related to their condition or treatment.
Nursing Interventions
Assess for indicators of circulatory overload, such as bluish discoloration of the skin (cyanosis), difficulty breathing (dyspnea), swelling (edema), distended neck veins, shortness of breath, and rapid breathing (tachypnea). Rationale: Prompt identification of circulatory overload allows for timely interventions to prevent further complications. Excess glucocorticoids and mineralocorticoids can lead to sodium and water retention, predisposing the patient to this condition.
Monitor vital signs regularly, with particular attention to blood pressure and heart rate. Rationale: Cushing’s disease can cause elevated blood pressure due to increased fluid volume from sodium and water retention. An elevated heart rate (tachycardia) can be a compensatory response to the increased fluid volume and the heart working harder.
Carefully monitor the patient’s serum sodium and potassium levels. Rationale: Elevated cortisol levels can cause the body to retain sodium and water while increasing the excretion of potassium. Excess mineralocorticoids further exacerbate sodium and water retention and lead to significant potassium loss (hypokalemia).
Instruct the patient to elevate their feet when seated. Rationale: Elevating the legs promotes venous return and helps to reduce fluid buildup in the lower extremities, alleviating edema.
Advise the patient to follow a diet that is low in sodium and high in potassium. Rationale: Limiting sodium intake helps to minimize fluid retention and associated weight gain. Increasing potassium intake helps to counteract the potassium loss often seen in this condition due to hormonal imbalances.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Medical Conditions Affecting the Endocrine System
- Applied Anatomy and Physiology of the Endocrine System
- Acromegaly/Gigantism (Hyperpituitarism)
- Dwarfism (Panhypopituitarism)
- Addison’s Disease (Adrenal Insufficiency)
- Pheochromocytoma
- Cushing’s Syndrome
- Hyperaldosteronism
- Thyrotoxicosis
- Diabetes Mellitus
Conditions Affecting the Nervous System
- Applied Anatomy and Physiology of the Nervous System
- Trigeminal Neuralgia
- Bell’s Palsy
- Parkinson’s Disease
- Spinal Cord Compression
- Transverse Myelitis
Medical Diseases Affecting the Renal System
- Anatomy and Physiology of the Renal System
- Renal Disorders
- Urinary Tract Infections (UTIs)
- Cystitis
- Renal Failure (Acute and Chronic)Nephrotic Syndrome
- Polycystic Kidney Disease (PKD)
- Kidney Stones (Nephrolithiasis)
Conditions of the Lymphatic System
- Anatomy and Physiology of the Lymphatic System
- Lymphedema
- Lymphangitis and Lymphadenitis
- Hodgkin’s Disease
Conditions of the Musculo-Skeletal System
- Anatomy and Physiology of the Musculo-Skeletal System
- Tendonitis
- Rheumatoid Arthritis
- Osteoarthritis
- Gout
- Bursitis
- Ankylosing Spondylitis
- Osteoporosis
- Paget’s Disease
Skin Conditions (Dermatology)
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

