Conditions of the eye
Subtopic:
Foreign body in the eye

A foreign object in the eye is defined as any material that originates from an external source and enters the eye.
A foreign body in the eye describes the presence of any external object or substance that has entered and become lodged within the eye’s structures. This presence can lead to sensations of unease, discomfort, or even tissue damage.
These foreign bodies can vary greatly and encompass anything that is not naturally present within the eye. Common examples include minute particles like dust, fragments of wood, slivers of metal, small pieces of vegetation, insects, or shards of glass.
The majority of these foreign bodies tend to lodge themselves beneath the eyelids or rest on the surface of the eye itself. Upon entering the eye, a foreign object is most likely to impact either the cornea, the transparent front part of the eye, or the conjunctiva, the thin membrane lining the inner surface of the eyelids and the white part of the eye.
Foreign bodies can be classified based on their location within the eye:
It can be EXTRA OCCULAR: This refers to locations outside the inner structures of the eyeball, such as the eyelid itself, the sclera (the white of the eye), the conjunctiva, or the cornea.
It can be INTRAOCCULAR: This indicates the foreign body is located inside the eyeball itself, potentially in areas like the angle of the anterior chamber (the space between the cornea and the iris), the iris (the colored part of the eye), the lens (which focuses light), the vitreous (the gel-like substance filling the eye), or the retina (the light-sensitive layer at the back of the eye).
MORBID ANATOMY:
The cornea is a transparent, dome-shaped structure forming the anterior surface of the eye. Think of it as a protective shield for the front of the eye. Its primary function is to allow light to pass through into the eye. Additionally, the cornea plays a significant role in focusing light onto the retina, located at the back of the eye, which is crucial for clear vision.
The conjunctiva is a delicate, thin mucous membrane that overlays the sclera, commonly known as the white of the eye. It extends to the edge of the cornea. The conjunctiva also lines the inner surface of the eyelids, creating a moist environment.
A foreign object landing on the anterior part of the eye cannot migrate behind the eyeball due to the eye’s anatomy. However, these objects can cause abrasions or scratches on the cornea’s delicate surface. While most of these injuries are superficial and heal without issue, certain types of foreign materials can introduce infection or cause more significant damage that may potentially impair vision.
Causes of Foreign Bodies in the eye.
Foreign bodies commonly enter the eye due to routine daily activities, environmental elements, or unforeseen accidents. While most instances involve superficial objects that are easily removed, objects traveling at high velocity are particularly dangerous because of their capacity to penetrate deeper ocular tissues.
Foreign Objects at High Speed: Particles such as metal or glass are often propelled with force into the eye during events like explosions, the use of drills, or hammering activities. The combination of speed and sharp edges makes these objects a significant threat for serious injury.
Natural Causes:
Eyelashes: These can frequently detach and fall onto the eye’s surface, leading to irritation.
Dried Mucus: Small, hardened pieces of dried mucus can sometimes adhere to the eye’s surface, causing discomfort.
Environmental Debris:
Dirt and Sand: These fine particles are commonly swept into the eyes by wind or falling material, particularly in outdoor environments.
Sawdust: Small wood particles frequently enter the eyes during activities like woodworking or construction.
Sharp Particles:
Metal Fragments: This is a frequent risk in occupations involving welding, machining, or the use of power tools, where tiny metal pieces can become airborne.
Glass Fragments: These can result from incidents like car accidents, the breaking of glass objects, or explosions.
Cosmetics: Products like mascara, eyeliner, or powdered makeup can inadvertently enter the eye, particularly during the application process.
Chemicals: Cleaning solutions, industrial chemicals, or various sprays can cause irritation or damage to the cornea upon contact with the eye’s surface.
Contact Lenses: If lenses are damaged or handled improperly, small particles can be introduced into the eye, leading to discomfort or injury.
Signs and Symptoms of foreign bodies in the eye.
The presence of foreign bodies in the eyes can manifest through a range of symptoms and signs. These vary based on the object’s location, size, and nature.
A. Corneal Foreign Body
Pain: The cornea has a high density of nerve endings, meaning even minute foreign objects can cause intense pain.
Foreign Body Sensation: Individuals often describe a persistent feeling that something is lodged in their eye, even if the object is not immediately visible.
Photophobia (Light Sensitivity): Irritation of the cornea triggers sensitivity to light, as the resulting inflammation impacts the pupillary light reflex.
Tearing: Excessive tear production is a natural protective response by the eye to flush away the irritating substance.
Blurred Vision: This can occur if the foreign body affects the central area of the cornea, thus interfering with the passage of light.
Ciliary Injection: Redness that is most prominent around the limbus (the border between the cornea and sclera) indicates inflammation or irritation of the cornea.
Hypopyon: The presence of pus accumulation in the anterior chamber suggests a severe infection or inflammatory response.
B. Conjunctival Foreign Body
Mild Discomfort: Compared to corneal foreign bodies, these are generally less painful due to the lower concentration of nerve endings in the conjunctiva.
Gritty Sensation: Individuals often describe a feeling similar to having sand in the eye.
Visible Foreign Body: Upon examination, the object is frequently visible on the surface of the conjunctiva.
Redness and Swelling: The irritation may be accompanied by redness of the conjunctiva (conjunctival injection) and mild swelling (edema).
Localized Irritation: The discomfort is usually confined to the specific area where the foreign body is in contact with the conjunctiva.
C. Intraocular Foreign Body (Penetrating)
Severe Pain and Vision Loss: These are indicators of significant damage to the inner structures of the eye.
Photophobia and Tearing: These are reflex actions aimed at protecting the injured eye.
Hyphema: The presence of blood in the anterior chamber suggests significant trauma to the iris or the ciliary body.
Retinal Damage or Detachment: This may manifest as the perception of flashing lights, new floaters, or a sudden loss of peripheral vision.
Nausea and Vomiting: These symptoms can accompany severe trauma, possibly due to the stimulation of the vagus nerve.
D. Chemical Foreign Bodies
Burning Pain: This is often severe, with the intensity depending on the nature of the chemical. Alkali burns tend to cause deeper and more significant damage than acidic burns.
Tearing and Redness: These are immediate reactions as the eye attempts to flush out the irritating substance.
Corneal Opacification: In severe cases, the cornea may become cloudy or opaque, affecting vision.
Conjunctival Injection: Intense redness indicates irritation or damage to the conjunctiva.
Additional Clinical Signs
Lid Edema: Significant irritation or trauma can lead to swelling of the eyelids.
Subconjunctival Hemorrhage: Bleeding beneath the conjunctiva can be a sign of minor trauma or chemical irritation.
Anterior Chamber Reaction: The presence of inflammatory cells or blood in the anterior chamber suggests deeper penetration or severe irritation.
A Feeling of Pressure or Discomfort: The physical presence of the object can create a persistent sensation of heaviness or pressure within the eye.
Sensation of a Foreign Body: Even if the object is not visible, individuals may have a persistent feeling that something is stuck in their eye.
Rubbing of Eyes: The instinctive reaction to rub the eyes in an attempt to dislodge the object can actually worsen abrasions or push the object deeper.
Eye Pain: The intensity of the pain varies depending on the location and type of foreign body. Corneal foreign bodies are particularly painful due to the cornea’s high nerve density.
Extreme Tearing: Reflexive tearing is the eye’s natural attempt to wash away the irritant.
Photophobia (Pain When Looking at Light): Inflammation and irritation make the eye sensitive to light, causing additional discomfort.
Excessive Blinking: Increased blinking is a natural protective mechanism of the eye.
Redness or Bloodshot Appearance: The dilation of blood vessels in the conjunctiva results in visible redness.
Discharge of Fluid or Blood: This is a sign of structural damage or rupture and is more commonly seen in penetrating injuries.
Classification of Foreign Bodies in the Eye
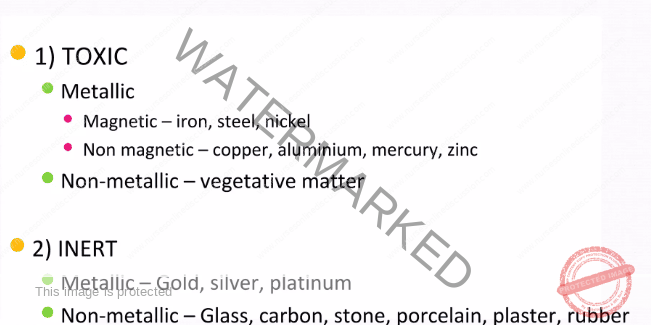
Classification Based on Toxicity
| Type | Description | Examples | Clinical Relevance |
| Toxic | Foreign bodies composed of substances capable of causing chemical burns, systemic poisoning, or significant tissue damage. | – Metallic: Iron, nickel, copper, mercury. <br> – Non-Metallic: Organic (plant, wood) or inorganic (plastic, glass). | – Can induce severe inflammation or infection, especially with organic matter that may harbor bacteria. <br> – Certain metals like copper and mercury can be absorbed systemically, leading to broader health issues. |
| Inert | Foreign bodies made of materials that are generally non-toxic, primarily causing irritation or mechanical injury rather than chemical damage. | – Metallic: Gold, silver, platinum. <br> – Non-Metallic: Glass, carbon, rubber. | – Often well-tolerated by the eye’s tissues, such as gold. <br> – May still cause irritation or abrasions if embedded within the ocular structures. |
Classification Based on Material Properties
| Type | Examples | Clinical Relevance |
| Metallic | ||
| Magnetic | Iron, steel, nickel. | – Readily extracted using a magnet. <br> – Iron and steel can rust within the eye, forming toxic corneal rust rings that require specialized removal, often using an Alger brush. |
| Non-Magnetic | Copper, aluminum, mercury, zinc. | – Copper: Can lead to chalcosis, a condition characterized by significant inflammation and deposition of copper in ocular tissues. <br> – Mercury: Highly toxic and poses a risk of systemic absorption, affecting various bodily functions. <br> – Zinc: Can cause localized tissue irritation and inflammation within the eye. |
| Non-Metallic | ||
| Organic | Wood, thorns, plant material, insect parts. | – Carry a high risk of infection due to the potential introduction of bacteria or fungi into the eye. |
| Inorganic | Glass, plastic, stone, porcelain, rubber. | – Generally less chemically reactive with ocular tissues. <br> – Can still cause substantial mechanical damage to the eye depending on their size, shape (especially sharpness), and the force of impact. |
Classification Based on Location
| Location | Description | Examples | Clinical Relevance |
| Superficial | Foreign body situated on the outermost layer of the cornea or the conjunctiva. | Dust, sand, small metal shavings. | – Usually easily accessible and can be removed with relative ease. <br> – May result in corneal abrasions if not addressed promptly, potentially causing discomfort and infection risk. |
| Embedded | Foreign body partially or completely lodged within the cornea, sclera, or conjunctiva. | Plant thorns, glass shards, metallic particles. | – Can lead to scarring of the ocular tissues, increase the risk of localized infection, and cause tissue damage if not carefully and properly removed by a healthcare professional. |
| Intraocular | Foreign body that has penetrated the eyeball, potentially reaching deeper internal structures. | High-velocity metal fragments, sharp objects. | – Represents a medical emergency requiring prompt intervention. <br> – Can cause serious complications such as hyphema (bleeding in the eye), retinal detachment, and permanent vision loss if left untreated. |
Classification Based on Mechanism of Entry
| Type | Description | Examples | Clinical Relevance |
| Blunt Trauma | Impact to the eye without penetration of the globe; the foreign body may remain on the surface or cause abrasions. | Dirt, dust, small particles. | Can result in significant irritation and tearing. Superficial corneal injuries such as abrasions are common. |
| Sharp Trauma | Injuries involving penetration of the eye by sharp objects, potentially embedding foreign bodies deeply. | Needles, plant thorns, glass shards. | Carries an increased risk of intraocular infection due to the breach of the eye’s protective barrier. Retinal damage and serious structural complications, including perforation of the globe, are possible. |
| High Velocity | Objects propelled into the eye at high speeds, often associated with industrial or accidental incidents. | Metal fragments (e.g., during welding), explosions. | Presents a high risk of the foreign body penetrating deep into the eye (intraocular penetration). Severe complications like hyphema (bleeding inside the eye) and globe rupture are significant concerns. Requires immediate and specialized medical intervention. |
Management of Foreign Body in the Eye
The management of foreign bodies in the eyes encompasses immediate first aid, care provided in a medical facility, and steps taken to prevent such incidents.
A. Emergency Management (Pre-Hospital)
Wash Hands: It is crucial to ensure hands are thoroughly clean before touching the affected eye area. This simple step significantly reduces the risk of introducing bacteria and causing a secondary infection.
Inspect the Eye in Bright Light: Utilize a flashlight or another source of intense light to carefully examine the eye. This enhanced illumination helps in better visualizing the foreign object and assessing the extent of any visible injury.
Avoid Eye Pressure: It is imperative not to press on or rub the injured eye. Applying pressure can force the foreign body deeper into the tissues, exacerbating the injury and potentially causing further damage.
Do Not Use Tools: Refrain from attempting to remove the foreign body with implements like tweezers or cotton swabs directly on the eye’s surface. Such actions can easily push the object further into the eye or scratch the delicate corneal surface.
Restrict Eye Movement: Minimize movement of the injured eye. Instruct the patient to try and keep both eyes as still as possible. This helps prevent further irritation or potential dislodgement of an embedded object.
Do Not Remove Contact Lenses: Unless there is visible swelling of the eye or suspicion of a chemical injury, it is generally advisable to leave contact lenses in place. Attempting to remove them can cause additional trauma to the already irritated eye.
Bandage the Eye: Gently cover the injured eye with a clean cloth or sterile gauze pad. This provides a protective barrier against further contamination and accidental rubbing.
Cover the Uninjured Eye: Covering the unaffected eye can help to minimize sympathetic movement of the injured eye. Since both eyes tend to move together, limiting the movement of the good eye helps to keep the injured eye still.
Refer to Hospital: It is essential to ensure the patient receives prompt professional medical evaluation and treatment in a hospital setting. Emergency management is primarily for stabilization and preventing further harm before expert care is available.
B. Hospital Management
Topical Anesthesia:
Proparacaine or Tetracaine: These topical anesthetic eye drops are administered to temporarily numb the surface of the eye. This is done to allow for a painless and more comfortable examination and removal of the foreign body.
Fluorescein Staining:
A harmless fluorescent dye is applied to the surface of the eye. When viewed under a cobalt blue light, this dye will highlight any areas where the corneal epithelium has been disrupted, such as corneal abrasions, or reveal the presence of a foreign object.
Inspection and Removal:
A magnifying device or a slit lamp (a microscope with a bright light) is used to carefully locate the foreign object. The high magnification and illumination allow for precise identification and removal.
Moistened Cotton Swab: For foreign bodies located superficially on the conjunctiva, a gentle swipe with a sterile, moistened cotton swab is often sufficient for removal.
Irrigation: Sterile saline solution can be used to flush out loose, non-embedded debris from the surface of the eye.
Special Instruments: For objects that are embedded or more difficult to remove, specialized ophthalmic instruments such as an Alger brush (for removing rust rings) or fine forceps are used with precision under magnification.
Management of Corneal Abrasions:
Antibiotic Ointments: To prevent bacterial infection of the abrasion, antibiotic ointments such as Ciprofloxacin or Moxifloxacin are typically prescribed.
Cycloplegics: Eye drops like cyclopentolate or homatropine are used to temporarily paralyze the muscles that control focusing and pupil constriction. This helps to dilate the pupil and reduce painful muscle spasms that can occur with corneal abrasions.
Pain Management:
Over-the-counter pain relievers such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended to manage pain associated with larger abrasions or persistent discomfort following foreign body removal.
Advanced Imaging:
CT Scan: In cases where an intraocular foreign body is suspected or there is concern about fractures of the orbital bones surrounding the eye, a CT scan can provide detailed imaging to guide further management.
Treatment of Complications:
Corneal Rust Rings: If a metallic foreign body containing iron has been present for some time, a rust ring may form on the cornea. This is carefully removed using a specialized tool called an Alger brush under high magnification.
Hyphema Management: If bleeding into the anterior chamber of the eye (hyphema) occurs, management typically includes elevating the patient’s head to help the blood settle, applying cold compresses to the eye, and referral to an ophthalmologist for specialized care and monitoring.
C. Prevention
Protective Eyewear: Wearing appropriate eye protection is paramount in preventing foreign bodies from entering the eye. This includes using:
Goggles or safety glasses specifically designed for impact resistance when working with tools such as saws, grinders, or hammers that can project particles.
Specialized eyewear designed to protect against chemical splashes when handling chemicals or engaging in activities like welding that produce fumes and sparks.
Hygiene and Awareness:
Avoid touching your eyes, especially with dirty hands. This simple practice minimizes the introduction of foreign materials and potential pathogens.
Be particularly aware of your surroundings in environments where there is a higher risk of airborne debris, such as construction sites, windy areas, or during gardening, and take necessary precautions
Complications of Foreign Bodies in the Eye
If foreign bodies in the eye are not treated promptly or are managed incorrectly, a variety of complications can arise. The nature and severity of these complications are influenced by the characteristics of the foreign body itself—such as its type, size, and location—as well as the speed and mechanism of its entry into the eye.
Rust Ring: When foreign bodies composed of iron or steel come into contact with the eye’s natural fluids, they can undergo oxidation, resulting in the deposition of a rust ring on the cornea. This rust deposit can cause ongoing irritation, hinder the healing process, and necessitates removal using specialized ophthalmic instruments, such as an Alger brush, to prevent further corneal damage.
Corneal Abrasions and Erosions: These involve superficial scratches on the cornea. They can be caused directly by the foreign body as it makes contact with the eye or during attempts to remove it. If not managed appropriately, these abrasions can develop into recurrent corneal erosions, leading to chronic pain and potential blurring of vision due to irregularities on the corneal surface.
Infectious Keratitis: This is an infection of the cornea, a serious complication frequently associated with organic foreign bodies like pieces of wood or plant material. These materials can introduce bacteria or fungi into the cornea, leading to inflammation and infection. If left unchecked, infectious keratitis can progress to form corneal ulcers or abscesses, which can severely impair vision and even cause permanent vision loss.
Endophthalmitis: This represents a severe infection within the eye itself. It typically arises from penetrating injuries that allow pathogens to enter the inner structures of the eyeball. Endophthalmitis is a sight-threatening emergency requiring immediate and aggressive treatment to prevent irreversible blindness or even the loss of the eye.
Hyphema: This refers to bleeding into the anterior chamber of the eye, the space between the cornea and the iris. It is usually a consequence of trauma caused by a penetrating or high-velocity foreign body. The presence of blood can lead to an increase in intraocular pressure, staining of the cornea, and potentially the development of secondary glaucoma.
Iritis or Anterior Uveitis: This involves inflammation of the iris (iritis) or the anterior portion of the uveal tract (anterior uveitis). It often occurs due to trauma or irritation caused by a foreign body. Symptoms include pain in the eye, increased sensitivity to light (photophobia), and redness. If not properly treated, it can lead to long-term complications, such as synechiae, which are adhesions between the iris and the lens.
Scleral or Corneal Scarring: Permanent scar tissue can form on the sclera (the white of the eye) or the cornea as a result of embedded foreign bodies or as a complication of abrasions and infections. Significant visual impairment can occur if the scar tissue is located in the central visual axis, obstructing the passage of light to the retina.
Globe Rupture: This is a severe injury involving the breach of the eye’s outer protective layers. It can be caused by penetrating foreign bodies or significant blunt force trauma to the eye. A globe rupture is a medical emergency that often requires surgical intervention to attempt to repair the eye, and it frequently results in partial or total loss of vision.
Retinal Detachment: High-velocity foreign bodies entering the eye can cause direct damage to the retina, leading to its separation from the underlying layer of tissue. Patients may experience symptoms like flashes of light, the sudden appearance of floaters in their vision, or a shadow or curtain-like loss of vision. Urgent surgical repair is necessary to reattach the retina and prevent permanent blindness.
Sympathetic Ophthalmia: This is a rare but serious immune response where trauma to one eye triggers inflammation in the other, uninjured eye. It is a complex reaction that can lead to vision loss in both eyes if not identified and treated aggressively in the early stages.
Increased Risk of Glaucoma: Secondary glaucoma can develop as a consequence of various complications from a foreign body. Chronic inflammation within the eye, the presence of blood in the anterior chamber (hyphema), or scarring of the structures involved in fluid drainage can all lead to an unhealthy elevation of intraocular pressure, which can progressively damage the optic nerve and result in gradual vision loss.
Subconjunctival Hemorrhage: This involves bleeding underneath the conjunctiva, the clear membrane covering the white part of the eye. It is often seen following blunt trauma. While it can appear alarming, it usually resolves spontaneously without specific treatment, but it is important to rule out more severe underlying injuries.
Persistent Foreign Body Sensation: Even after the foreign body has been removed, individuals may experience a continued feeling that something is still in their eye. This can be due to the incomplete removal of microscopic debris or the presence of secondary abrasions on the cornea. This persistent discomfort may necessitate further evaluation and management to alleviate the symptoms.
Anterior Chamber Foreign Bodies: Small foreign bodies can sometimes settle within the anterior chamber of the eye. Their presence can cause ongoing inflammation and increase the risk of secondary infection. Removal often requires specialized surgical techniques to access this area of the eye safely and effectively.
Cataract Formation: Penetrating injuries that damage the lens capsule, the outer covering of the eye’s natural lens, can lead to the development of traumatic cataracts. This clouding of the lens impairs vision and typically requires surgical intervention to remove the cataract and restore clear sight.
Nursing Interventions for a Child with a Foreign Body in the Eye
The primary goals of nursing interventions for a child with a foreign body in the eye are to minimize the child’s pain and anxiety, prevent potential complications, ensure timely and effective medical treatment, and educate caregivers on preventive measures.
Assess the Child’s Condition.
Intervention: Conduct a careful and thorough assessment of the child’s affected eye. Document any observable signs, including redness, excessive tearing, swelling of the eyelids, or the presence of a visible foreign body.
Rationale: An early and detailed assessment is crucial for determining the severity of the injury and guides the immediate course of care and necessary interventions.
Ensure Safety and Comfort.
Intervention: Approach the child calmly and reassuringly. Attempt to keep the child as still as possible to minimize further movement of the eye and potential exacerbation of the injury.
Rationale: Reducing the child’s anxiety and agitation is vital. It minimizes reflexive actions such as rubbing the eye or excessive blinking, which could worsen the injury.
Educate the Caregiver.
Intervention: Provide clear and concise instructions to the child’s caregiver, emphasizing the importance of not touching the eye or attempting to remove the foreign body themselves.
Rationale: Improper handling of the eye can worsen the existing condition or lead to secondary trauma, potentially embedding the object further or causing an abrasion.
Position the Child Properly.
Intervention: Position the child in an upright or seated position. Instruct them to avoid lying flat, particularly if there is a suspicion of a penetrating injury to the eye.
Rationale: Maintaining an upright position helps reduce intraocular pressure. In cases of potential penetration, it can minimize the risk of fluid leakage from the eye.
Restrict Eye Movement.
Intervention: Gently cover both of the child’s eyes with a sterile dressing or an eye shield. This is done even if only one eye is affected.
Rationale: Because the eyes move in tandem, covering both eyes helps to significantly restrict ocular movement in the injured eye, preventing further irritation or damage.
Perform Gentle Irrigation (If Appropriate).
Intervention: If the foreign body appears to be superficial and it is deemed safe to do so, gently irrigate the affected eye with sterile saline solution.
Rationale: Irrigation can effectively flush out loose debris from the surface of the eye without causing additional trauma. However, this should only be done if there is no suspicion of penetration.
Administer Prescribed Topical Anesthesia.
Intervention: Administer any prescribed topical anesthetic eye drops, such as proparacaine, as directed by the healthcare provider.
Rationale: Topical anesthetics help to numb the surface of the eye, reducing pain and discomfort. This makes it easier for medical personnel to examine the eye and remove the foreign body if necessary.
Monitor for Signs of Complications.
Intervention: Closely observe the child for any signs that might indicate the development of complications. This includes monitoring for signs of infection (increased redness, discharge), any changes in vision, or increased swelling and redness around the eye.
Rationale: Prompt detection of complications like an infection or hyphema ensures timely medical intervention, potentially preventing more serious outcomes.
Provide Pain Management.
Intervention: Administer prescribed pain relievers, such as acetaminophen or ibuprofen (if age-appropriate and ordered), to manage any discomfort the child is experiencing.
Rationale: Relieving pain not only improves the child’s comfort but also helps to keep them calm and more cooperative during examination and treatment procedures.
Facilitate Ophthalmology Referral.
Intervention: Ensure that an immediate referral to an ophthalmologist is arranged, especially in cases where the foreign body is suspected to be penetrating the eye or is embedded within the ocular tissues.
Rationale: Specialized care provided by an ophthalmologist is essential to prevent potentially serious complications such as corneal scarring or permanent vision loss.
Support Emotional Well-being.
Intervention: Use age-appropriate language and communication techniques to explain any procedures to the child. Involve caregivers in comforting and reassuring the child throughout the process.
Rationale: Addressing the child’s fear and anxiety is important for gaining their cooperation and building trust with the healthcare team.
Educate on Prevention.
Intervention: Provide comprehensive education to both the child (if age-appropriate) and their caregivers about the importance of using protective eyewear during activities that pose a risk to the eyes. This includes activities such as playing with sharp objects, using tools, participating in sports, or engaging in outdoor activities where airborne particles are present.
Rationale: Educating on preventive measures is crucial to reduce the risk of future eye injuries and foreign body incidents.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

