Conditions Affecting the Endocrine System
Subtopic:
Hyperaldosteronism
Table of Contents
Learning Objectives
Explain the role of aldosterone in regulating sodium, water balance, and blood pressure.
Differentiate between primary and secondary hyperaldosteronism based on pathophysiology and causes.
Identify clinical manifestations of hyperaldosteronism, including hypertension and hypokalemia.
Describe diagnostic tests used to confirm hyperaldosteronism, such as aldosterone and renin levels.
Outline treatment options for primary hyperaldosteronism, including surgical and pharmacological approaches.
Formulate nursing diagnoses and interventions for patients with hyperaldosteronism, focusing on cardiac output and electrolyte balance.
Hyperaldosteronism
Hyperaldosteronism indicates a condition characterized by overly high amounts of aldosterone in the body.
Aldosterone
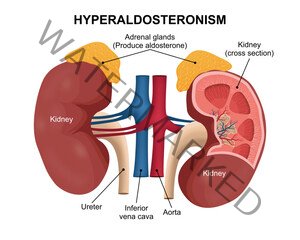
Aldosterone is a crucial mineralocorticoid hormone. This hormone is synthesized by the adrenal gland, specifically within the zona glomerulosa, which constitutes the outermost region of the adrenal cortex. Aldosterone’s primary function involves controlling the levels of sodium and water in the body. By regulating these components, aldosterone exerts a significant influence on maintaining blood pressure.
It is a type under ALDOSTERONISM, so therefore, lets start from the very beginning.
ALDOSTERONISM/ CONN’S SYNDROME
Disorders affecting the secretion of aldosterone can be broadly categorized into two main types:
Primary Hyperaldosteronism
Secondary Hyperaldosteronism
Primary Hyperaldosteronism
This condition arises due to the excessive and autonomous production of aldosterone. This surplus of aldosterone leads to increased sodium retention within the body and a corresponding loss of potassium. This imbalance results in a combination of low potassium levels (hypokalemia) and elevated blood pressure (hypertension).
Causes of hyperaldosteronism
A common cause is the presence of benign tumors on the adrenal gland called adrenal adenomas (Conn’s syndrome). These adenomas are responsible for approximately 60% of primary hyperaldosteronism cases.
Clinical presentation
Hypertension: Elevated blood pressure is a hallmark symptom.
Hypokalemia (<3.5mmol/l): Lower than normal potassium levels in the blood.
Muscle weakness: Low potassium can interfere with normal muscle function.
Nocturia: Frequent urination during the night.
Tetany (involuntary muscle contractions): Muscle spasms or cramps due to electrolyte imbalances.
Diagnosis
High sodium: Sodium levels in the blood may be elevated due to increased retention.
Low potassium level: Confirming hypokalemia through blood tests.
High serum aldosterone level: Measuring the level of aldosterone in the blood.
Low renin level: Renin, an enzyme involved in blood pressure regulation, is typically suppressed in primary hyperaldosteronism.
Aldosterone excretion rate after salt loading is diagnostic for primary aldosteronism: This test assesses how the body handles aldosterone after an increase in salt intake.
Renin-aldosterone stimulation test: This test evaluates the relationship between renin and aldosterone levels under specific conditions.
Treatment and management of primary hyperaldosteronism.
Removal of adenoma surgically (adrenalectomy): Surgical removal of the adrenal tumor is the primary treatment for adenoma-caused hyperaldosteronism.
Those with hypokaleamia should be treated by aldosterone antagonists e.g. spironolactone (100–400mg) daily: Medications like spironolactone block the action of aldosterone and help manage low potassium.
Pair with aldosterone receptor antagonist e.g. eplerenone is a useful alternative: Eplerenone works similarly to spironolactone by blocking aldosterone receptors.
Calcium channel blockers like Nefidipine are also useful moderately: These medications can help manage hypertension.
Correct hypokalemia: Restoring normal potassium levels is crucial.
Usual postoperative care with abdominal surgery: Standard post-surgical care is necessary after adrenalectomy.
Administer steroids like: Steroids may be needed temporarily after surgery to support adrenal function.
Hydrocortisone–Cortisol
Cortisone–Cortate
Prednisone–Deltasone
Prednisolone-Prelone
Triamcinolone–Kenalog
Betamethasone–Celestone
Fludrocortisone (contains both mineralocorticoid and Florinef glucocorticoid): This steroid has both mineralocorticoid and glucocorticoid properties.
Fluids: Maintaining proper hydration is important.
Monitoring of blood sugar: Steroid use can affect blood sugar levels.
Control of hypertension with spironolactone: Spironolactone helps manage high blood pressure.
Aldosterone-blocking drugs – Medications that inhibit the effects of aldosterone are a key treatment, particularly for individuals unsuitable for surgery. This is also the preferred approach when hyperaldosteronism is due to overactivity of both adrenal glands. Surgery is not typically an option in such cases, as removing part of the glands might not resolve the issue, and complete removal necessitates lifelong corticosteroid therapy to prevent Addison’s disease. Therefore, medication blocking aldosterone’s action may be the only feasible treatment.
Secondary hyperaldosteronism
This condition mirrors the clinical presentation of primary hyperaldosteronism but stems from excessive stimulation of the zona glomerulosa by renin, leading to increased Angiotensin II production.
Common causes include accelerated hypertension and renal arterial stenosis (narrowing of the arteries supplying the kidneys).
Causes associated with normal blood pressure (normotension) include congestive cardiac failure and cirrhosis (scarring of the liver).
Treatment includes:
Angiotensin–converting enzyme inhibitors e.g. captopril, enalapril and angiotensin II antagonists e.g. losartan, are effective in managing heart failure symptoms and improving lifespan. Spironolactone has also demonstrated increased survival rates in heart failure patients.
Complications
Problems related to high blood pressure – Sustained high blood pressure can lead to:
Heart attack, heart failure, and other heart problems
Stroke
Kidney disease or kidney failure
Problems related to hypokalemia or low blood potassium level
Arrhythmias (irregular heartbeats)
Muscle cramps
Excessive thirst and urination
Hyperaldosteronism Nursing Diagnosis
Diagnosis 1: Decreased cardiac output related to increased vascular resistance due to hypertension, as evidenced by high blood pressure level of 170/89, shortness of breath, high aldosterone levels, fatigue and inability to do activities of daily living as normal.
Desired Outcome: The patient will be able to maintain adequate cardiac output.
Intervention: Assess the patient’s vital signs and characteristics of heart beat every 4 hours. Observe for signs of decreasing peripheral tissue perfusion such as slow capillary refill, facial pallor, cyanosis, and cool, clammy skin. Administer prescribed medications for hypertension and hyperaldosteronism.
Rational: Regular assessment aids in accurate diagnosis and monitors the effectiveness of treatment. Signs of reduced peripheral perfusion indicate a decline in the patient’s condition requiring immediate medical attention. The choice of medications depends on blood pressure readings, underlying conditions, and complications. This may involve vasodilators (direct or indirect), diuretics, and medications that reduce cardiac workload. Aldosterone-blocking drugs are also used to treat hyperaldosteronism caused by overactivity of both adrenal glands.
Diagnosis 2: Electrolyte Imbalance related to hypokalemia as evidenced by serum potassium level of 2.9 mmol/L, high aldosterone levels, polyuria, increased thirst, weakness, tachycardia, and fatigue.
Desired Outcome: Patient will be able to re-establish a normal electrolyte and fluid balance.
Intervention: Obtain a daily blood sample from the patient. Administer a slow intravenous potassium solution as prescribed.
Rationale: Blood tests are necessary to monitor serum potassium levels. Slow intravenous potassium administration helps to safely raise potassium levels. A slow infusion rate is essential to avoid irritation or burning at the infusion site.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Medical Conditions Affecting the Endocrine System
- Applied Anatomy and Physiology of the Endocrine System
- Acromegaly/Gigantism (Hyperpituitarism)
- Dwarfism (Panhypopituitarism)
- Addison’s Disease (Adrenal Insufficiency)
- Pheochromocytoma
- Cushing’s Syndrome
- Hyperaldosteronism
- Thyrotoxicosis
- Diabetes Mellitus
Conditions Affecting the Nervous System
- Applied Anatomy and Physiology of the Nervous System
- Trigeminal Neuralgia
- Bell’s Palsy
- Parkinson’s Disease
- Spinal Cord Compression
- Transverse Myelitis
Medical Diseases Affecting the Renal System
- Anatomy and Physiology of the Renal System
- Renal Disorders
- Urinary Tract Infections (UTIs)
- Cystitis
- Renal Failure (Acute and Chronic)Nephrotic Syndrome
- Polycystic Kidney Disease (PKD)
- Kidney Stones (Nephrolithiasis)
Conditions of the Lymphatic System
- Anatomy and Physiology of the Lymphatic System
- Lymphedema
- Lymphangitis and Lymphadenitis
- Hodgkin’s Disease
Conditions of the Musculo-Skeletal System
- Anatomy and Physiology of the Musculo-Skeletal System
- Tendonitis
- Rheumatoid Arthritis
- Osteoarthritis
- Gout
- Bursitis
- Ankylosing Spondylitis
- Osteoporosis
- Paget’s Disease
Skin Conditions (Dermatology)
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

