Neurological Disorders in Children
Subtopic:
Hypoxic Ischemic Encephalopathy
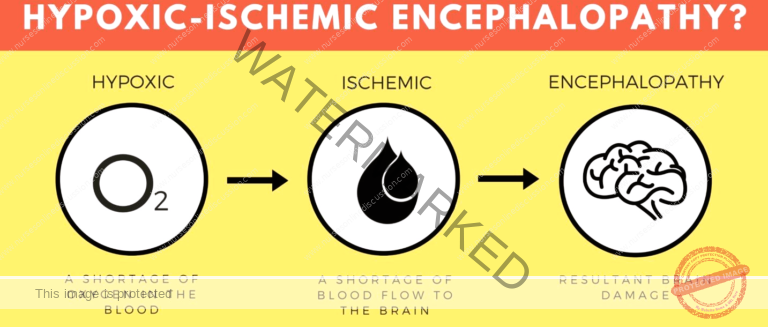
Hypoxic Ischemic Encephalopathy (HIE) describes a form of brain injury in newborns that occurs when the brain experiences a shortage of oxygen and reduced blood supply.
Hypoxic Ischemic Encephalopathy develops when the brain doesn’t receive sufficient oxygen, potentially leading to permanent damage. Hypoxic Ischemic Encephalopathy is considered a type of birth injury, a broad term encompassing any injury a baby sustains around the time of delivery. Other terms sometimes used to refer to HIE include birth asphyxia, perinatal asphyxia, and neonatal encephalopathy.
Hypoxic Ischemic Encephalopathy is a specific type within the broader category of “Encephalopathy“.
Encephalopathy
Encephalopathy is a general medical term indicating damage or dysfunction affecting the brain. It has various underlying causes, such as infections, liver problems, and exposure to toxic substances.
Some significant types of encephalopathy include:
Chronic Traumatic Encephalopathy: This condition results from direct trauma to the brain, which causes damage to nerve tissue. It’s frequently observed in individuals involved in contact sports.
Hepatic Encephalopathy: This often develops as a consequence of liver cirrhosis. When the liver cannot effectively filter waste products, toxins accumulate in the bloodstream and affect the brain.
Glycine Encephalopathy: This is a genetic form of encephalopathy where symptoms typically appear shortly after birth.
Toxic Metabolic Encephalopathy: This type arises from exposure to toxins, infections, or organ failure. Imbalances in the body’s chemical composition can disrupt normal brain function.
Hypoxic-Ischemic Encephalopathy: This occurs when the brain is deprived of adequate oxygen, potentially resulting in lasting brain damage.
Hypertensive Encephalopathy: Prolonged and untreated high blood pressure can cause the brain to swell, leading to neurological impairment.
Uremic Encephalopathy: This develops when the kidneys are not functioning correctly and are unable to remove harmful substances from the body. The accumulation of uremic toxins can cause confusion and other neurological symptoms.
Etiology of Hypoxic Ischemic Encephalopathy
From a pathological standpoint, any factors that disrupt the exchange of substances between maternal and fetal blood can contribute to HIE. These factors can be categorized as maternal, related to delivery, or fetal.
Maternal factor:
Hypoxia: Low oxygen levels in the mother.
Anemia: A deficiency of red blood cells in the mother.
Diabetes: Maternal diabetes can impact fetal oxygenation.
Hypertension: High blood pressure in the mother.
Smoking: Maternal smoking can reduce oxygen supply to the fetus.
Nephritis: Inflammation of the kidneys in the mother.
Heart disease: Maternal heart conditions can affect blood flow to the placenta.
Advanced or young maternal age: Being older or younger can increase risk.
Delivery condition:
Abruption of placenta: Premature separation of the placenta from the uterine wall.
Placenta previa: When the placenta covers the cervix.
Prolapsed cord: When the umbilical cord descends into the birth canal before the baby.
Premature rupture of membranes: When the amniotic sac breaks before labor begins.
Fetal factor:
Multiple birth: Twins or triplets can increase the risk.
Congenital or malformed fetus: Existing fetal conditions can contribute.
High Risk Factors
Mismanagement of a high-risk pregnancy: Conditions like preeclampsia and gestational diabetes necessitate intensive monitoring and care.
Umbilical cord complications: The umbilical cord is vital for oxygen and nutrient transport to the baby and waste removal. Any compression or impairment of the cord’s function puts the baby at risk of HIE.
Placental or uterine complications: The placenta and uterus are essential for providing oxygenated blood to the baby. Examples of issues include:
Placental abruption: The placenta detaches from the uterus prematurely.
Placenta previa: The placenta is positioned too close to the cervix, potentially causing bleeding and oxygen deprivation during delivery.
Placental insufficiency: The placenta cannot adequately supply blood to the baby.
Uterine rupture: A tear in the wall of the uterus, either partial or complete.
Infections: Infections in the mother can spread to the baby during labor and delivery, particularly if proper precautions aren’t taken, such as screening and administering necessary antibiotics.
Improper fetal heart monitoring: If a baby shows signs of distress on the monitor, prompt intervention can restore oxygen supply, potentially including an emergency C-section. Failure to monitor adequately can lead to missed critical warning signs.
Failure to prevent a premature birth: Premature infants have a higher susceptibility to HIE due to underdeveloped lungs. Measures to prevent premature birth, like cervical cerclage or progesterone treatment, are important.
Allowing prolonged labor to continue: Labor is stressful for babies due to contractions compressing the placenta and umbilical cord. If labor isn’t progressing, and interventions like an emergency C-section aren’t offered, it can be considered negligent. Prolonged labor is more likely with larger babies or smaller maternal pelvic size.
Medication problems: Medications like Pitocin and Cytotec, used to induce or augment labor, can sometimes cause excessively strong and frequent contractions, leading to dangerous oxygen deprivation for the baby.
Mismanagement of a neonatal condition: HIE can arise from complications in the newborn period (the first month of life). Issues like respiratory distress, jaundice, and neonatal hypoglycemia can contribute to an HIE diagnosis if not properly managed.
Clinical Features of Hypoxic Ischemic Encephalopathy
Breathing problems
Feeding problems
Missing reflexes (e.g., absence of response to loud noises)
Seizures
Low Apgar scores (a measure of a newborn’s health immediately after birth)
Low or high muscle tone
Altered level of consciousness (e.g., not being alert)
Classification of Hypoxic Ischemic Encephalopathy
Clinical Classification
Mild (stage I): Baby is overly alert, irritable, has normal muscle tone and reflexes, no seizures, and a normal EEG (electroencephalogram).
Moderate (stage II): Baby is lethargic, has reduced muscle tone (hypotonia), weak sucking and Moro reflex, often experiences seizures, and an abnormal EEG.
Severe (stage III): Baby is in a coma, has absent muscle tone and reflexes, persistent seizures, and a significantly abnormal EEG.
Levene Classification
| Feature | Mild | Moderate | Severe |
| CONSCIOUSNESS | Irritable | Lethargy | Comatose |
| TONE | Hypotonia | Marked | Severe |
| SEIZURE | No | Yes | Prolonged |
| SUCKING/ RESPIRATION | Poor Suck | Unable to Suck | Unable to maintain spontaneous respiration |
Sarnat Staging Classification
(Commonly used)
Sarnat staging, combined with EEG findings, helps determine the infant’s prognosis.
| Grade I Mild | Grade II Moderate | Grade III Severe | |
| Alertness | Hyperalert | Lethargy | Coma |
| Muscle tone | Normal or increased | Hypotonic | Flaccid |
| Seizures | None | Frequent | Uncommon |
| Pupils | Dilated, reactive | Small, reactive | Variable, fixed |
| Respiration | Regular | Periodic | Apnoea |
| Duration | < 24 Hours | 2 – 14 Days | Weeks |

Management of Hypoxic Ischemic Encephalopathy
This situation requires immediate pediatric medical attention; it’s a pediatric emergency.
HIE is primarily managed using therapeutic hypothermia. This treatment involves cooling the baby’s brain or body to a temperature slightly below normal. This cooling process helps to slow down the damaging effects of oxygen deprivation on brain cells. By reducing the metabolic rate, it gives the brain a better chance to recover and can lessen the long-term disability the child might experience. Current medical guidelines stipulate that this treatment should ideally commence within six hours of birth and generally not be initiated after 24 hours.
The general treatment of encephalopathy varies significantly depending on the specific underlying cause of the condition.
Generalized treatment:
Ventilation: Respiratory support may be necessary.
CPAP (continuous positive airway pressure): Provides constant air pressure to keep airways open.
CMV (continuous mandatory ventilation): A machine-driven method of breathing.
HFOV (High-frequency oscillatory ventilation): Uses very fast, small breaths to oxygenate the blood.
Perfusion/Circulation: Medications may be used to support blood pressure and circulation.
Dopamine/Dobutamine: Drugs that can help increase heart contractility and blood pressure.
Energy: Maintaining stable blood glucose levels is crucial for brain function.
Normal glucose level maintained (50-110mg/dl): Avoiding both low (hypoglycemia) and high (hyperglycemia) blood sugar is important.
Fluid: Fluid management is critical.
60-80ml/kg/d: Typical daily fluid requirement.
Restriction if SIADH (Syndrome of inappropriate antidiuretic hormone secretion): A condition where the body retains too much water, requiring fluid restriction.
Electrolytes: Monitoring and maintaining electrolyte balance is vital.
Sodium and Calcium should be monitored: These electrolytes play crucial roles in nerve and muscle function.
Avoid Polycythemia: High red blood cell count can impede blood flow.
If Hct>65-70, partial exchange transfusion is done to bring Hct level to 55: Removing some of the baby’s blood and replacing it with donor blood to reduce red blood cell concentration.
Control of seizures: Seizures associated with HIE can be difficult to manage.
Phenobarbital loading dose 15-20mg/kg, iv maintenance dose 3-5mg/kg, iv: An anticonvulsant medication.
Phenytoin loading dose 15-20mg/kg, iv maintenance dose 5mg/kg, iv: Another anticonvulsant medication.
Midazolam: 0.1-0.3mg/kg, iv: A fast-acting sedative and anticonvulsant.
Leveracetam, Topiramate: Other anticonvulsant medications that might be used.
EEG: Electroencephalography is used to monitor brain electrical activity.
Special Investigations
Continuous aEEG – Amplified EEG used for cerebral function monitoring: A specialized EEG technique to continuously assess brain function, especially in newborns.
Detects voltage pattern- burst, low voltage, isoelectric: Identifies different patterns of brain electrical activity.
Detects electrical seizure activity: Helps to identify seizures occurring in the brain.
CT scan: Computed tomography scan.
Only indicated in emergency: Usually performed if there is a need for immediate structural imaging of the brain.
Prognosis
The long-term outlook depends significantly on the extent of brain damage and the effectiveness of medical treatment.
Mild or moderate cases could be cured completely: Babies may recover fully with minimal or no lasting effects.
Severe cases represent poor prognosis with high mortality or cerebral complications such as mental retardation & cerebral palsy: Severe HIE often leads to significant long-term neurological disabilities.
Overall mortality – 20%: Approximately 20% of babies with HIE do not survive.
Overall incidence of sequele – 30%: About 30% of survivors experience long-term complications.
Mild: 100% good prognosis: Babies with mild HIE generally have a very favorable outcome.
Moderate: 80% normal: Around 80% of babies with moderate HIE will develop normally.
Severe: 50% death, 50% sequele: In severe cases, there is roughly a 50% chance of death and a 50% chance of surviving with long-term complications.
Presence of seizure increases chance of Cerebral palsy by 50-70 times: Seizures are a strong indicator of increased risk for cerebral palsy.
Prevention
Better Obstetric care: Ensuring high-quality care during pregnancy and delivery.
Skilled resuscitation teams and neonatal facilities: Having trained personnel and appropriate resources available to manage birth complications.
Nursing Diagnosis
Acute Confusion related to Hypoxia, Disturbance in cerebral metabolism, Accumulation of toxins in the brain, Structural changes in the brain as evidenced by Cognitive dysfunction, Altered psychomotor performance, Tremors, Fluctuation in the level of consciousness, Agitation, Misperception, Neurobehavioral manifestations, Difficulty initiating purposeful behavior.
Impaired Memory related to Neurological disturbances related to encephalopathy, Inadequate intellectual stimulation, Changes in brain structure and processes, Irreversible brain damage, Depressive symptoms as evidenced by Reports experiences of forgetfulness, Consistently forgets to schedule or keep appointments, Difficulty recalling events, Difficulty recalling familiar names, objects, and words, Inability to learn or retain new skills or information, Inability to perform a previously learned skill.
Disturbed Thought Processes related to Insufficient oxygen supply to the brain secondary to encephalopathy, Head trauma related to encephalopathy, Infections as evidenced by Incorrect perception of stimuli, Difficulty performing activities of daily living, Difficulty communicating verbally, Impaired interpretation of events, Impaired judgment, Impaired decision making, Inadequate emotional responses, Disorientation.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

