Pediatric Conditions of the Respiratory System
Subtopic:
Meconium Aspiration Syndrome
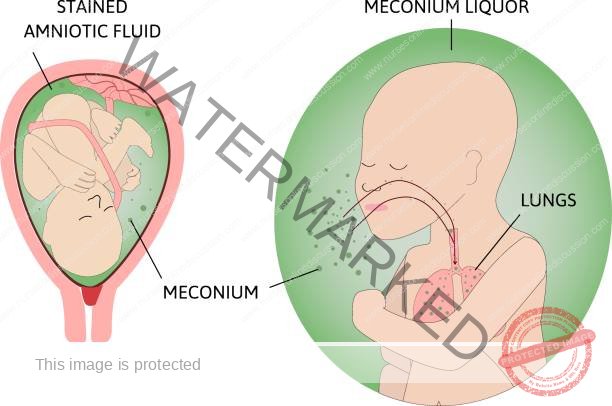
Meconium aspiration syndrome refers to breathing difficulties, specifically respiratory distress, observed in a newborn infant. This condition arises when the baby inhales (aspirates) meconium, a dark green, sterile fecal substance, into their lungs either before or around the time they are born.
Meconium represents a newborn’s earliest stool. In some instances, infants may pass meconium while still in the womb during labor or delivery. This results in what is known as meconium-stained amniotic fluid (MSAF). Meconium is the initial intestinal discharge of newborns, characterized as a thick, dark-green material. Its composition includes cells shed from the intestinal lining, fine fetal hair (lanugo), mucus, and secretions produced by the intestines, such as bile.
Meconium aspiration syndrome (MAS) occurs when the infant inhales amniotic fluid that is contaminated with meconium. This aspiration event can take place before birth, during the birthing process, or immediately after the baby is born.
Causes of Meconium Aspiration Syndrome
Placental Insufficiency: This occurs when the placenta doesn’t provide sufficient blood flow to the developing baby. This inadequate blood supply can lead to fetal distress, a condition that may trigger the premature release of meconium.
Preeclampsia: This pregnancy complication involves high blood pressure and can restrict blood flow to the placenta. When the placenta doesn’t deliver enough oxygen and nutrients to the fetus due to this reduced blood flow (maternal underperfusion), it can lead to fetal distress and subsequent meconium passage. Pathological changes in the placenta and maternal blood vessels are associated with this condition.
Maternal Infection/Chorioamnionitis: This involves an infection of the amniotic fluid and placental membranes following their rupture. The placenta exhibits signs of acute chorioamnionitis (representing the mother’s inflammatory response) and funisitis (indicating the fetus’s inflammatory response).
Fetal Hypoxia: When the fetus experiences oxygen deprivation, it can stimulate the nervous system, leading to the passage of meconium due to the maturing gastrointestinal system’s response.
Clinical Features
Severe Respiratory Distress: Significant breathing difficulty may be present, indicated by symptoms such as a bluish discoloration of the skin (cyanosis), grunting noises at the end of exhalations, widening of the nostrils with each breath (nasal flaring), visible sinking of the chest between the ribs during inhalation (intercostal retractions), rapid breathing (tachypnea), and a rounded chest appearance (barrel chest) due to trapped air. In some cases, abnormal lung sounds like crackling (rales) and coarse rattling (rhonchi) can be heard with a stethoscope.
Staining of the Fingernails: A yellowish-green discoloration of the fingernails, as well as the umbilical cord and skin, may be observed due to the presence of meconium.
Green Urine: In newborns with MAS, green-tinged urine may be noticeable within the first 24 hours after birth. This occurs because meconium pigments absorbed by the lungs can be filtered and excreted in the urine.
Meconium Staining: The amniotic fluid will have a meconium or dark green appearance.
Tachypnea: An abnormally fast respiratory rate.
Nasal Flaring: Widening of the nostrils during breathing, indicating increased effort.
Retractions: Pulling in of the skin between the ribs or above the collarbone during breathing, signifying respiratory distress.
Cyanosis or Desaturation: A bluish tint to the skin or a lower than normal oxygen saturation level in the blood.
Rales: Crackling or bubbling sounds heard in the lungs.
Rhonchi: Coarse, snorting, or rattling sounds heard in the lungs.
Greenish Yellow Staining: The umbilical cord, nail beds, or skin may exhibit a greenish-yellow discoloration from the meconium. Meconium staining may be visible in the back of the throat (oropharynx) and, if the baby requires a breathing tube, in the voice box (larynx) and windpipe (trachea).
Barrel-shaped Chest: Newborns with trapped air in their lungs may develop a rounded or barrel-shaped chest.
Fetal Distress: Signs indicating the baby is not tolerating labor well before birth.
Signs of Neonatal Asphyxia: Indications that the newborn has suffered from a lack of oxygen around the time of birth.
Pathophysiology
In Utero Meconium Passage: Before birth, the passage of meconium is usually a result of the developing gastrointestinal (GI) tract being stimulated by the nervous system, often due to the fetus experiencing a lack of oxygen (hypoxic stress).
GI Tract Maturation: As the fetus nears full term, the GI system matures. Stimulation of the vagus nerve (which can occur from head or spinal cord compression) can trigger bowel movements and the relaxation of the rectal sphincter, leading to meconium release.
Amniotic Fluid Alteration: Meconium changes the nature of the amniotic fluid, reducing its ability to fight bacteria, which consequently elevates the risk of bacterial infection around the time of birth.
Skin Irritation: Meconium can irritate the fetal skin, increasing the likelihood of a common newborn rash called erythema toxicum.
Meconium Aspiration: The most serious problem arising from meconium passage before birth is the inhalation (aspiration) of the meconium-stained amniotic fluid by the baby before, during, or immediately after delivery – this is meconium aspiration syndrome (MAS).
Aspiration Mechanism: If the fetus is under stress, it may exhibit a gasping breathing pattern, which can lead to the aspiration of meconium-stained amniotic fluid.
Pulmonary Effects: The aspiration of meconium causes oxygen deprivation (hypoxia) through four main effects on the lungs: blocking the airways, disrupting the function of surfactant (a substance that helps keep the air sacs in the lungs open), causing chemical inflammation of the lungs (pneumonitis), and leading to high blood pressure in the lungs (pulmonary hypertension).
Diagnosis
Acid-Base Status: Measuring the levels of acidity (pH), carbon dioxide (pCO2), and oxygen (pO2) in arterial blood, as well as continuously monitoring oxygen levels using a pulse oximeter, are essential for proper care. Calculating the oxygenation index (OI) can be useful when considering more advanced treatments like ECMO.
Serum Electrolytes: Measuring the levels of sodium, potassium, and calcium in the blood is recommended about 24 hours after birth in infants with MAS. This is because complications like SIADH (a condition causing fluid imbalance) and acute kidney failure can occur due to the stress around birth.
Complete Blood Cell Count: Measuring hemoglobin and hematocrit levels ensures there are enough red blood cells to carry oxygen. Low platelet counts (thrombocytopenia) increase the risk of bleeding in newborns. Elevated or decreased white blood cell counts with immature forms (neutropenia or neutrophilia with left shift) may indicate a bacterial infection around birth.
Chest Radiography: A chest X-ray is crucial to confirm the diagnosis of MAS, assess the extent of lung involvement, identify collapsed lung areas (atelectasis) and air leaks, and verify the correct placement of breathing tubes and catheters in the umbilical cord. The diagnosis is supported by X-ray findings of overinflated lungs with patchy areas of collapse and a flattened diaphragm.
Echocardiography: An ultrasound of the heart is necessary to check the heart’s structure and function, as well as to determine the severity of pulmonary hypertension and any abnormal blood flow patterns (right-to-left shunting).
Meconium Passage and Respiratory Distress: Observing the passage of meconium and the presence of breathing difficulties are key indicators.
Differential Diagnosis
Aspiration Syndromes (other causes of inhaling fluids or substances into the lungs)
Congenital Heart Disease with Pulmonary Hypertension (heart defects causing high lung pressure)
Pediatric Congenital Diaphragmatic Hernia (a birth defect where organs move into the chest)
Pediatric Idiopathic Pulmonary Artery Hypertension (high blood pressure in the lung arteries with no known cause)
Pediatric Pneumonia (lung infection)
Pediatric Sepsis (blood infection)
Persistent Pulmonary Hypertension of the Newborn (PPHN) (continued high lung pressure after birth)
Surfactant Deficiency (lack of the substance that helps keep air sacs open)
Transient Tachypnea of the Newborn (rapid breathing in newborns that usually resolves quickly)
Transposition of the Great Arteries (a serious heart defect)
Management of Meconium Aspiration Syndrome
Routine Neonatal Care and Monitoring: Infants with MAS should receive standard newborn care while being closely watched for any signs of breathing problems, following established neonatal resuscitation guidelines.
Suctioning: Clearing the airway with suctioning to remove any blockages.
Avoid Routine Endotracheal Suctioning: Current guidelines generally advise against routinely suctioning the windpipe of non-vigorous infants with MAS.
Chest Tube Insertion: In vigorous infants, a chest tube may be inserted with underwater seal drainage to address collapsed lung areas (atelectasis) or air leaks into the chest cavity (pneumothorax).
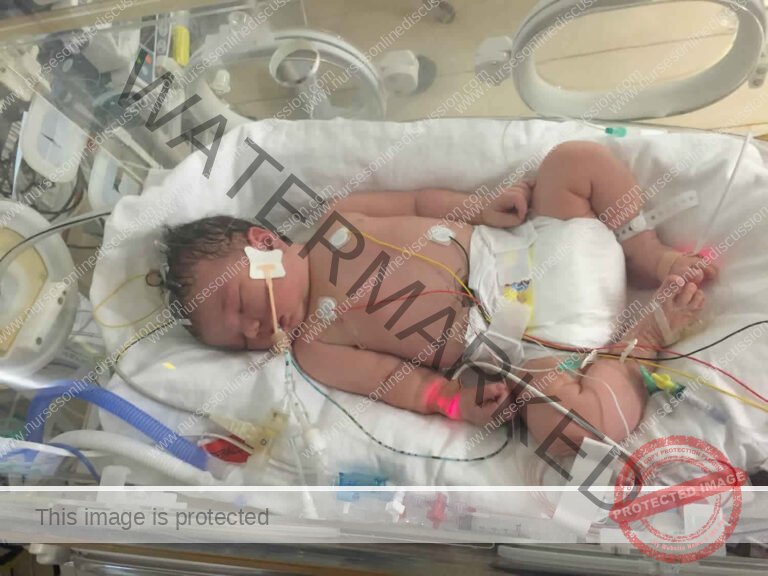
NICU Admission: Newborns may be admitted to the neonatal intensive care unit (NICU) for specialized care.
Oxygen Therapy: Providing extra oxygen is often necessary to maintain oxygen saturation above 90%, preventing tissue oxygen deprivation and improving overall oxygen levels.
Surfactant: While not a standard treatment for all cases, surfactant replacement may be considered as surfactant dysfunction plays a role in MAS. It can help to improve lung function.
Cardiac Exam: A thorough heart examination and echocardiogram are important to rule out congenital heart disease and persistent pulmonary hypertension of the newborn (PPHN).
Rooming-in (for vigorous infants): If the baby is breathing normally and has good muscle tone (vigorous), they can stay with the mother for initial newborn care. A bulb syringe can be used to gently clear secretions from the nose and mouth.
Radiant Warmer (for non-vigorous infants): If the baby has weak breathing or poor muscle tone (non-vigorous), they should be placed on a radiant warmer for resuscitation, including clearing secretions and providing warmth, support, and stimulation.
Minimize Handling: It’s crucial to handle these infants gently and minimally, as they are easily agitated. Agitation can worsen pulmonary hypertension and abnormal blood flow, leading to further oxygen deprivation and acidosis. Sedation may be required to keep the baby calm.
Umbilical Artery Catheter: Inserting a catheter into an umbilical artery allows for frequent monitoring of blood pH and blood gas levels without repeatedly disturbing the infant.
Respiratory Care: Ongoing respiratory support includes oxygen therapy via a hood or positive pressure ventilation. Maintaining adequate oxygen levels in the blood is critical. Approximately 30% of infants with MAS require mechanical ventilation. Efforts are made to use the lowest possible airway pressure and shortest possible breath delivery time. Oxygen saturation should be kept between 90-95%.
Surfactant Therapy: Surfactant can be administered to replace missing or inactive surfactant and to help clear meconium from the airways. Although it may not change mortality rates, it can lessen the severity of the illness, reduce the need for ECMO, and shorten the hospital stay.
IV Fluids: Intravenous fluids are started with adequate dextrose (sugar) to prevent low blood sugar (hypoglycemia). Fluid rates are often slightly restricted (60-70 mL/kg/day).
Diet: Nutrition is gradually advanced by adding electrolytes, protein, fats, and vitamins to ensure proper nourishment and prevent deficiencies.
Antibiotics: Medications like Ampicillin and Gentamicin are given to prevent or treat potential infections.
Systemic Vasoconstrictors: These medications help to prevent abnormal blood flow in the heart by raising the systemic blood pressure above the lung pressure. Common examples include dopamine, dobutamine, and epinephrine, with dopamine being the most frequently used.
Pulmonary Vasodilator: Inhaled nitric oxide is used to widen the blood vessels in the lungs, helping with pulmonary hypertension and PPHN.
Neuromuscular Blocking Agents: These medications cause temporary muscle paralysis to optimize ventilation, improving oxygenation and ventilation. They also help to reduce lung injury from the ventilator and minimize the baby’s oxygen use.
Sedatives: These medications help to maximize the effectiveness of mechanical ventilation, reduce oxygen consumption, and manage discomfort from invasive procedures.
Nursing Diagnosis
Elevated Body Temperature (Hyperthermia): Secondary to the body’s inflammatory response and/or a hypermetabolic state. This is indicated by an elevated body temperature reading, skin that is warm to the touch, and tachycardia, which is an abnormally rapid heart rate.
Compromised Fluid Volume: Occurring because the body’s regulatory mechanisms are not effectively maintaining fluid balance.
Compromised Tissue Perfusion: Related to the reduced efficiency of oxygen movement across the alveolar and capillary membranes within the lung tissues.
Disruption in Breastfeeding: Associated with the newborn’s current illness, as evidenced by the necessary physical separation of the mother and infant for medical care.
Potential Risk for Impaired Parent-Newborn Emotional Bond: Due to the newborn’s physical health issues and the resulting need for hospitalization, which can limit normal bonding opportunities.
Nursing Care Planning and Goals
The newborn will maintain a stable core body temperature, evidenced by vital signs remaining within normal ranges and white blood cell (WBC) counts within expected levels.
The newborn will maintain appropriate fluid balance, as shown by adequate urine output with urine specific gravity within normal limits, stable vital signs, moist mucous membranes, good skin elasticity (turgor), rapid return of skin color after blanching (capillary refill), and the resolution of any swelling (edema).
The newborn will demonstrate improved tissue perfusion, indicated by skin that is warm and dry, strong peripheral pulses readily palpable, vital signs within normal parameters, adequate urine output, and the absence of swelling (edema).
The mother will verbalize understanding and effectively demonstrate methods to support breast milk production until direct breastfeeding can be safely and effectively initiated.
The mother will understand and demonstrate techniques for sustaining lactation and identify appropriate methods for providing expressed breast milk to her newborn during this period.
The mother will learn and demonstrate strategies to promote the newborn’s behavioral regulation and physiological organization.
Following hospital discharge, the parents will report and exhibit mutually satisfying interactions and a strong emotional bond with their newborn.
Nursing Interventions
Actively work to reduce body temperature: Implement tepid sponge baths (TSB) as a physical method to aid in temperature reduction. Strictly adhere to sterile techniques for all equipment utilized for the newborn, and diligently avoid sharing equipment between infants to minimize the potential for cross-infection. Administer fever-reducing medications (antipyretics) as prescribed by the physician.
Work to improve fluid volume status: Closely monitor and meticulously document vital signs at regular intervals, noting and reporting any significant variations or concerning trends. Provide meticulous oral care to maintain comfort and hydration by regularly moistening the lips. Ensure thorough skin care through daily baths to maintain skin integrity. Administer intravenous (IV) fluids as specifically ordered by the medical team to effectively compensate for identified or potential fluid losses.
Work to enhance tissue perfusion: Perform regular assessments of the peripheral pulses, noting their quality and strength to monitor circulatory status. Closely monitor respiratory rate, depth of respiration, and the overall effort of breathing. Assess the skin for any changes in color (pallor, cyanosis), temperature (coolness), and moisture (clamminess). Elevate any extremities exhibiting edema periodically to potentially aid in fluid redistribution and reduce tissue oxygen demand.
Facilitate and support breastfeeding efforts: Demonstrate the correct and efficient use of a manual piston-type breast pump to the mother. Thoroughly review and clearly explain appropriate techniques for the safe storage and proper utilization of expressed breast milk to maintain its nutritional and hygienic qualities. Provide a private, quiet, and calm environment for the mother when she is attempting to breastfeed or pump. Encourage frequent attempts at breastfeeding when possible or simulated sucking if breastfeeding is not yet feasible. Educate and encourage the mother to prioritize adequate rest for her own recovery, maintain sufficient fluid intake and nutritional balance, and establish a consistent breast pumping schedule, aiming for approximately every 3 hours while awake to stimulate and maintain milk supply.
Foster a positive parent-infant relationship: Provide parents with education regarding expected newborn growth patterns and developmental milestones to increase their understanding and address any parental concerns or misperceptions. Actively involve parents in the direct care of their newborn in ways that are manageable and promote their confidence, and provide consistent positive reinforcement and praise for nurturing and protective parenting behaviors observed.
Evaluation
Goals were successfully met, as evidenced by:
The newborn maintained a stable core body temperature, demonstrated by vital signs remaining within expected ranges and white blood cell (WBC) counts within normal limits.
The newborn successfully maintained appropriate fluid balance, evidenced by adequate urine output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor, prompt capillary refill, and resolution of edema.
The newborn demonstrated improved tissue perfusion, evidenced by warm and dry skin, strong peripheral pulses, normal vital signs, adequate urine output, and the absence of edema.
The mother understood and demonstrated techniques to sustain lactation until direct breastfeeding could be initiated safely.
The mother was able to understand and demonstrate techniques for sustaining lactation and identify ways to provide breast milk to her newborn effectively.
The mother understood and demonstrated techniques to enhance the newborn’s behavioral organization and self-regulation.
Following discharge from the hospital, the parents demonstrated positive and mutually satisfying interactions and bonding behaviors with their newborn.
Complications
Persistent high blood pressure in the pulmonary arteries and lungs (persistent pulmonary hypertension).
Pneumothorax: Collection of air within the pleural space surrounding the lungs, potentially causing lung collapse.
Aspiration pneumonia: Lung infection resulting from the inhalation of foreign materials, such as gastric contents.
Hypoxic brain injury: Damage to brain tissue due to an insufficient supply of oxygen to the brain.
Prolonged respiratory distress: Ongoing breathing difficulties that extend beyond the acute phase.
Atelectasis: Collapse of lung tissue in part or all of the lung.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

