Medical Nursing (III)
Subtopic:
Anatomy and Physiology of the Musculo-skeletal System

The musculoskeletal system is fundamentally responsible for enabling movement (locomotion), providing structural support to the body, and establishing the body’s framework. It is a complex and integrated system.
This system comprises three primary components: skeletal muscles, bones, and joints.
The Skeletal Muscle
Skeletal muscle is composed of numerous bundles of individual muscle cells, known as myocytes. Within these myocytes are the protein filaments actin and myosin. The organized interaction of these actin and myosin molecules forms structures called myofibrils, which are the fundamental units responsible for muscle contraction, similar to the mechanism in heart muscle.
Each individual myocyte, also termed a muscle fiber or sarcomere, is an elongated cell. Its outer boundary is the cell membrane, referred to as the sarcolemma. The nuclei of the cell are located just beneath this membrane. Myocytes also contain myoglobin, a specialized protein that binds and stores oxygen, providing a readily available oxygen supply for muscle activity.
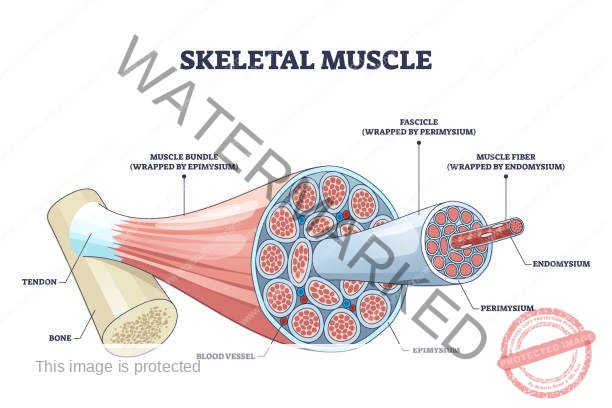
Surrounding each individual myocyte is a layer of connective tissue called the endomysium. Groups of these muscle fibers are bundled together into structures called fascicles, and each fascicle is enclosed by another connective tissue layer known as the perimysium. Finally, the entire muscle itself is encased in a further connective tissue sheath called the epimysium.
These three connective tissue layers (endomysium, perimysium, and epimysium) converge and extend beyond the muscle fibers to form a tendon. The tendon is a strong, fibrous cord that attaches the muscle to the surface of a bone at a specific point called the enthesis. Surrounding the epimysium and tendon is a layer of fibrous tissue known as the muscle fascia, providing further support and organization.
Physiology of a Skeletal Muscle
The sarcomere is considered the fundamental functional unit of muscle contraction. Muscle contraction occurs through a process where the light (actin) filaments and the dark (myosin) filaments within the sarcomere slide past each other, effectively bringing them closer together. This interaction shortens the overall length of the muscle cell.
The myosin filaments have numerous knob-like projections, often called heads, that can form temporary connections, known as cross-bridges, with the actin filaments. The formation of these cross-bridges triggers the contraction process. The cross-bridges then move, pulling the actin filaments past the myosin filaments.
Once a cross-bridge has moved as far as it can, it detaches from the actin, returns to its original position, and can then attach to a new binding site on the actin filament. This cycle of attachment, pulling, and detachment continues as long as the muscle is stimulated to contract.
The energy for this entire process is provided by adenosine triphosphate (ATP). If ATP is depleted or absent, the muscle is unable to release the cross-bridges, resulting in a sustained contraction known as muscle fatigue, which can ultimately lead to muscle cramps.
Control of Muscle Contraction
Skeletal muscle contraction is under the control of the central nervous system (CNS). Each muscle fiber is connected to a motor neuron, a specialized nerve cell that transmits signals from the CNS. When an impulse travels down the motor neuron, it triggers muscle contraction.
The point where a motor neuron comes into contact with a muscle fiber is called the neuromuscular junction. At the axon terminal of the motor neuron, vesicles contain a neurotransmitter called acetylcholine.
When a nerve impulse reaches the neuromuscular junction, it causes the release of acetylcholine into the synaptic cleft (the small gap between the neuron and muscle fiber). Acetylcholine binds to receptors on the muscle fiber membrane, triggering a series of events that lead to the release of calcium ions within the muscle cell. These calcium ions interact with regulatory proteins associated with the actin and myosin filaments, allowing them to bind and form cross-bridges. The muscle cell will remain in a state of contraction as long as acetylcholine continues to be produced and stimulate the muscle fiber.
To terminate the contraction, an enzyme called acetylcholinesterase is produced at the neuromuscular junction. This enzyme breaks down acetylcholine, preventing further stimulation of the muscle fiber. This allows for the re-absorption of calcium ions back into the muscle cell, causing the cross-bridges to detach and the muscle to relax.
The intensity of a muscle contraction depends on the specific task being performed. The frontal lobe of the cerebrum, the part of the brain responsible for motor control, determines which muscle cells need to contract and the number of cells required to achieve the desired movement or action.
Bones
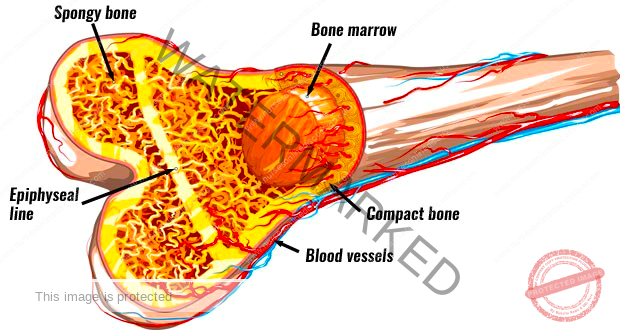
Bones constitute the body’s framework, defining its shape and providing structural form. They serve as attachment points for muscles and ligaments, crucial for movement and stability. Beyond structural support, bones play vital roles in protecting delicate internal organs from injury. They act as a reservoir for calcium, storing and releasing this essential mineral as needed by the body. Furthermore, bones are the site of hematopoiesis, the process of forming blood cells. Working in conjunction with muscles and joints, bones enable the movement of the body as a whole.
The fundamental functional unit of bone tissue is the osteocyte, a mature bone cell embedded within the bone matrix. Osteoblasts are specialized cells responsible for producing the bony matrix, a complex substance composed of collagen, minerals (primarily calcium and phosphate), carbohydrates, and proteins. The maintenance of healthy bone tissue is a tightly regulated process influenced by various hormones, including thyroid hormones, growth hormones, calcitonin, parathyroid hormone, and adrenal hormones.
Joints
A joint, also known as an articulation, is the site where two or more bones meet. These junctions are essential for providing flexibility and enabling movement of the skeletal system.
Types of Joints
Joints are classified structurally and functionally. One major structural classification is based on the material connecting the bones.
Fibrous joints
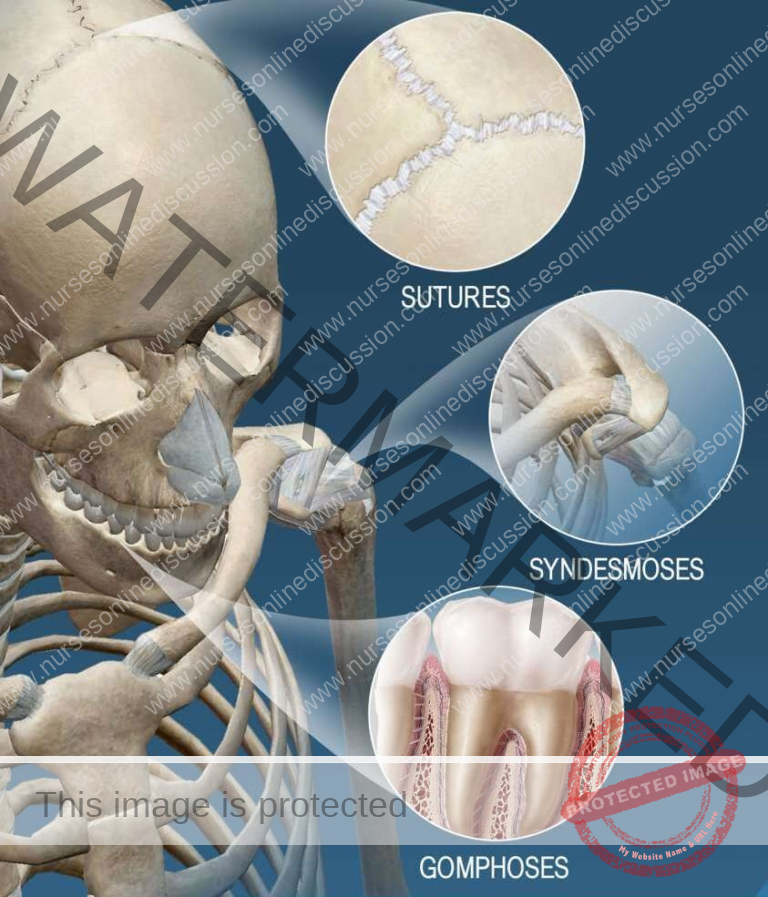
Fibrous joints are characterized by the direct connection of the articulating surfaces of bones through fibrous connective tissue. This type of joint generally allows for very limited or no movement. Examples of fibrous joints include the sutures in the skull, the middle radioulnar joint in the forearm, and the connections between teeth and the jawbones.
There are three main types of fibrous joints:
(1) Sutures: These are immovable joints (synarthroses) specifically found connecting the bones of the skull. The bones at these joints have interlocking, often serrated or irregular edges. These edges are bound together by short, dense fibers of connective tissue. This rigid connection provides significant protection for the brain.
(2) Gomphoses: These are also immovable joints. The term gomphosis refers to the peg-in-socket fibrous joint that exists between a tooth and its bony socket (alveolus) in the mandible or maxilla. The tooth is held firmly in place by the strong periodontal ligaments, which are specialized fibrous connective tissues.
(3) Syndesmoses: These are slightly movable joints (amphiarthroses) where two bones are connected by a ligament. The ligament, a band of fibrous connective tissue, allows for a greater range of movement compared to sutures or gomphoses, but still restricts movement significantly. A good example is the distal tibiofibular joint, located between the tibia and fibula at the ankle. The interosseous membrane between the radius and ulna in the forearm is another example, allowing for pronation and supination of the hand.
Cartilaginous joints

In cartilaginous joints, the ends of the bones involved in the articulation are joined together by cartilage. This type of joint allows for more movement than fibrous joints but less movement than synovial joints. Examples of cartilaginous joints include the intervertebral discs between the vertebrae of the spine, the pubic symphysis in the pelvis, and the costochondral joints connecting the ribs to the costal cartilage.
There are two primary types of cartilaginous joints:
(1) Synchondroses: These are immovable cartilaginous joints (synarthroses) where the connecting material is hyaline cartilage. The epiphyseal plate (growth plate) in growing bones is a temporary synchondrosis. Once bone growth is complete, this cartilage is replaced by bone, resulting in a synostosis (bony fusion). A permanent example is the joint between the first rib and the sternum, where the costal cartilage directly fuses with the sternum.
(2) Symphyses: These are slightly movable cartilaginous joints (amphiarthroses) where the bones are connected by a broad, flattened disc of fibrocartilage. This fibrocartilaginous pad is compressible, allowing for limited movement and acting as a shock absorber. The pubic symphysis, connecting the left and right pubic bones of the pelvis, is one example. Another prominent example is the intervertebral discs located between the vertebrae of the spinal column, which provide cushioning and flexibility to the spine.
Synovial joints

Synovial joints are distinguished by a space between the articulating bones called the synovial cavity. This cavity is enclosed by an articular capsule, the inner layer of which is the synovial membrane. The synovial membrane secretes synovial fluid, a viscous fluid that lubricates the joint, reduces friction between the bones during movement, and provides nutrients to the articular cartilage. This structural arrangement allows for a wide range of free movements. Examples of synovial joints include ball-and-socket joints like the hip and shoulder, and hinge joints such as those in the fingers (interphalangeal joints) and the knee.
A key characteristic of synovial joints is the presence of articular cartilage covering the bone surfaces where they come into contact. This smooth, specialized cartilage minimizes friction and absorbs shock, further facilitating smooth movement. Synovial joints are often reinforced and supported by ligaments, strong bands of connective tissue that connect bones and help to stabilize the joint, limiting excessive or unwanted movements that could cause injury.
There are six distinct types of synovial joints, each with a unique range of motion:
(1) Gliding joints (or plane joints): These joints allow bones to slide or glide past each other in a single plane. The movement is generally non-axial, meaning it doesn’t involve rotation around an axis. Examples include the intercarpal joints in the wrist and the intertarsal joints in the ankle, as well as the joints between the articular processes of vertebrae.
(2) Hinge joints: These joints permit movement along a single axis, primarily allowing for flexion (bending) and extension (straightening) movements. Major examples include the elbow joint, the interphalangeal joints of the fingers and toes, and the ankle joint.
(3) Pivot joints: These joints allow for rotational movement around a single longitudinal axis. A key example is the atlantoaxial joint, located between the first and second cervical vertebrae (atlas and axis), which enables the rotation of the head, such as when shaking your head “no.”
(4) Condyloid joints (or ellipsoidal joints): These joints allow for biaxial movement, meaning movement in two planes. This enables circular motion (circumduction), as well as flexion and extension, and abduction and adduction (movement away from and towards the midline of the body). The wrist joint, specifically the articulation between the radius and the carpal bones, is a classic example.
(5) Saddle joints: These unique joints are characterized by articulating surfaces that have both concave and convex areas, resembling a saddle. This allows for a wider range of movement than condyloid joints, including flexion, extension, abduction, adduction, and circumduction, but typically does not permit axial rotation. The carpometacarpal joint of the thumb, located between the trapezium carpal bone and the first metacarpal bone, is a prime example, enabling the opposable thumb.
(6) Ball-and-socket joints: These are the most freely moving synovial joints, allowing for multiaxial movement, including rotation around any axis. The spherical head of one bone fits into the cup-shaped socket of another. The hip joint and the shoulder joint are prominent examples of ball-and-socket joints, permitting a wide range of movements in multiple directions.
Hyaline cartilage
Hyaline cartilage is a specialized connective tissue that forms the articular surface within synovial joints. Unlike most connective tissues, hyaline cartilage is avascular, meaning it lacks a direct blood supply. Instead, it relies on the diffusion of nutrients from the synovial fluid within the joint capsule to maintain its health and function. Hyaline cartilage is primarily composed of a dense extracellular matrix rich in type II collagen fibers. These collagen fibers form a strong, interwoven meshwork that provides tensile strength. Embedded within this collagen network are large, complex molecules called proteoglycans, which attract and hold water, contributing to the cartilage’s resilience and ability to withstand compression forces.
DISEASES AFFECTING SKELETAL MUSCLES
MYASTHENIA GRAVIS
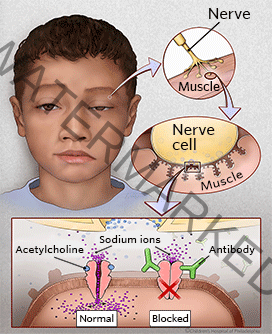
This autoimmune disorder disproportionately affects females and is characterized by abnormal muscle weakness and fatigability. The underlying cause is a reduction in the number of functional acetylcholine receptors at the neuromuscular junctions (also called myoneural junctions). Acetylcholine is a critical neurotransmitter required for muscle contraction, and a deficiency of its receptors impairs the transmission of nerve impulses to muscles.
Signs and Symptoms
The onset of myasthenia gravis is typically gradual.
Patients often experience excessive fatigue, particularly as the day progresses. A hallmark symptom is ptosis, or drooping of the eyelids, due to weakness of the eye muscles.
Frequent falls can occur due to muscle weakness.
Difficulties with chewing (mastication) and swallowing (dysphagia) are common as the muscles involved in these actions become weak.
If the respiratory muscles are affected, it can lead to serious complications, including respiratory failure, requiring ventilatory support.
A weakened cough reflex can impair the ability to clear secretions from the airways, increasing the risk of mucus buildup and respiratory infections.
Treatment and Management
Short-acting anticholinesterase drugs: Medications like edrophonium temporarily improve muscle strength by inhibiting the breakdown of acetylcholine in the neuromuscular junction, making more of the neurotransmitter available.
Long-acting anticholinesterase drugs: Drugs such as neostigmine or pyridostigmine have a more prolonged effect than short-acting agents, helping to manage the symptoms of muscle weakness over longer periods.
Thymectomy and steroids: Surgical removal of the thymus gland (thymectomy) can be beneficial in some patients, as the thymus is thought to play a role in the autoimmune response in myasthenia gravis. Corticosteroids (steroids) are immunosuppressant medications that can help reduce the autoimmune attack on acetylcholine receptors.
Exercises: Specific exercises, under the guidance of a physical therapist, can help maintain muscle strength and function, although overexertion should be avoided.
MYOSITIS (MYOPATHY)
Myositis or myopathy is a broad term referring to a group of diseases that primarily affect the muscles themselves, leading to muscle weakness. Myositis specifically indicates inflammation of the muscles and can have various underlying causes, including genetic factors and autoimmune processes.
Progressive muscular atrophy encompasses a group of hereditary disorders where there is a progressive degeneration of muscle tissue. This degeneration occurs without direct involvement of the bones or the nervous system’s sensory pathways.
The characteristic feature is symmetrical muscle wasting and weakness, meaning it affects both sides of the body relatively equally. Notably, there is no accompanying loss of sensation. Affected muscles may appear larger than normal (pseudohypertrophy) and feel firm to the touch, despite being weak.
Children with certain forms of progressive muscular atrophy may exhibit a distinctive gait, often described as a waddling gait, similar to that of a duck. Another classic sign is the Gowers’ sign (or tripod sign), observed when a child attempts to rise from a lying position on the floor. The child will typically roll onto their stomach (prone position) and then use their arms to “walk” their hands up their legs to push themselves into an upright position. In severe forms, involvement of the respiratory muscles often leads to a shortened lifespan, with death commonly occurring in the second decade of life.
Fibrositis – Rheumatism (Fibromyalgia)
Fibrositis, also known as fibromyalgia or muscular rheumatism, describes a condition characterized by chronic, widespread pain and stiffness in the muscles and soft tissues. The pain can be recurring and affect various parts of the body over time.
Unlike progressive muscular atrophy, fibrositis is not considered a progressive disease and does not cause muscle degeneration. The vague and subjective nature of the symptoms is often linked to factors such as emotional stress, sleep disturbances, and altered pain processing.
Treatment
Treatment for fibrositis is primarily aimed at managing symptoms.
Symptomatic relief: Focuses on alleviating pain and discomfort.
Heat and massages: Applying heat to affected areas and massage therapy can help to soothe muscles and reduce pain and stiffness.
Aspirin or NSAIDs: Non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin or ibuprofen can be prescribed to help reduce pain and inflammation, although their effectiveness varies among individuals with fibromyalgia. Other pain-relieving medications or therapies may also be used.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

