Pediatric Conditions of the Cardiovascular System
Subtopic:
Pericarditis
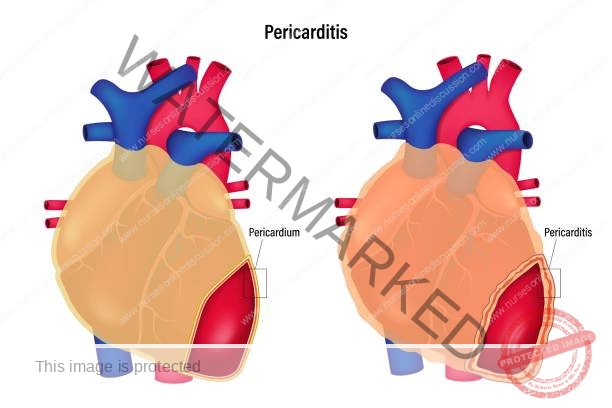
Pericarditis refers to the inflammation of the pericardium. This condition often presents acutely, meaning it develops rapidly, and its duration can extend for several months. In some instances, an excessive amount of fluid can accumulate within the pericardial sac, the space situated between the layers of the pericardium. This accumulation is known as a pericardial effusion.
The Pericardium
The pericardium is a delicate, sac-like structure that surrounds the heart. It consists of two layers and contains a small amount of fluid, typically around 50ml, between these layers. This fluid-filled space helps to reduce friction as the heart beats.
Functions of the Pericardium
It also prevents the heart from over-expanding when blood volume increases, thereby helping the heart maintain effective pumping action. This ensures the heart isn’t stretched beyond its capacity.
It protects the heart from infections or cancerous growths and physically confines the heart within the chest cavity. This provides a barrier and keeps the heart in its correct anatomical position.
Causes of Pericarditis
Infection
A) Viral infection: This is a major cause of pericarditis due to infection. Common culprits include coxsackie A and B viruses, particularly B3 and B5, as well as influenza and hepatitis viruses.
B) Bacterial infection: This can be caused by bacteria like tubercle bacilli (responsible for tuberculosis), Staphylococcus, Streptococcus, and Pneumococcus.
C) Fungal infection: Fungi such as Histoplasma and Candida species can lead to pericarditis. Also, infections like toxoplasmosis can be a cause.
D) Metabolic disorders:
Uraemia (build-up of waste products in the blood due to kidney failure) is a significant cause. Pericardial effusion, the accumulation of fluid around the heart, is a common presentation, especially after starting renal dialysis, and can sometimes worsen after dialysis treatment begins.
E) Connective tissue disorders: Conditions like systemic lupus erythematosus can trigger pericarditis due to autoimmune inflammation.
Other Causes:
Chest trauma / injury: Physical harm to the chest can inflame the pericardium.
Lung disease (Tuberculosis): Tuberculosis in the lungs can sometimes spread to the pericardium.
HIV (Human Immunodeficiency Virus): Weakened immune systems make individuals more susceptible to pericarditis.
Side effects of some medications: Certain drugs, such as Isoniazid and Tetracycline, have been linked to pericarditis as an adverse effect.
Malignancy: Cancer, either primary or metastatic, can affect the pericardium.
Scleroderma: This autoimmune disease can cause inflammation and thickening of the pericardium.
Radiation Induced: Radiation therapy to the chest can sometimes damage the pericardium.
Myxedema: Severe hypothyroidism can lead to pericardial effusion.
Acute MI (Myocardial Infarction): Inflammation can occur following a heart attack.
Dissection of Aortic Aneurysm: A tear in the wall of the aorta can sometimes affect the pericardium.
Ankylosing spondylitis: This inflammatory condition can sometimes involve the pericardium.
Inflammatory bowel disease: Conditions like Crohn’s disease and ulcerative colitis have been associated with pericarditis.
Rheumatic fever: This inflammatory disease, a complication of strep throat, can affect the heart, including the pericardium.
Cancer (including leukemia): Various cancers, including blood cancers, can involve the pericardium.
Pathophysiology of Pericarditis
The initial inflammatory response in the pericardium can result in the accumulation of either a thin, watery (serous) fluid or a thicker, pus-filled (purulent) fluid, or the deposition of a dense, fibrous material. In viral pericarditis, the fluid is typically serous, present in small amounts, and usually resolves without intervention.
In cases of pericarditis caused by cancer, tuberculosis, or bacterial infection, there may be large fluid accumulations that are exudative (rich in protein and cellular debris), hemorrhagic (containing blood), and filled with white blood cells.
A gradual build-up of fluid in the pericardial sac, even significant amounts up to 250 mL, may not initially produce noticeable symptoms.
Signs and Symptoms of Pericarditis
Beck’s triad is a classic combination of three signs suggesting acute cardiac tamponade, a dangerous condition where the heart is compressed.
These signs are:
Low arterial blood pressure: Reduced pressure in the arteries.
Distended neck veins: Swollen veins in the neck due to increased pressure.
Distant, muffled heart sounds: Heart sounds that are faint and difficult to hear.
Chest pain associated with pericarditis often has the following characteristics:
Sharp and stabbing chest pain: This distinctive pain is caused by the inflamed pericardial layers rubbing against each other with each heartbeat. The pain may worsen with activities like coughing, taking deep breaths, or lying flat.
Relief by sitting up and leaning forward: Adopting this position can reduce the friction and ease the pain. You might instinctively bend over or hold your chest to breathe more comfortably.
Other clinical features may include:
Pain radiating to the back, neck, or left shoulder.
A dry cough, not producing mucus.
Feelings of anxiety or unusual tiredness.
Difficulty breathing when lying down (orthopnea).
Swelling (edema) of the feet, legs, or ankles. This can be a sign of constrictive pericarditis.
In constrictive pericarditis, the pericardium becomes rigid and thickened, restricting the heart’s ability to expand fully and impacting its function.
Fever, indicating an inflammatory process.
Tachycardia, an elevated heart rate.
The compression from constrictive pericarditis can cause blood to back up, leading to swelling in the lungs, abdomen, and legs.
Palpitations, the sensation of skipped or rapid heartbeats.
Weakness and a general feeling of being unwell.
Irritability and mood changes.
Fatigue and lack of energy.
Loss of appetite.
Irregular heart beat (arrhythmia).
Cyanosis, a bluish discoloration of the skin due to low oxygen.
Cough, which may or may not be productive.
Hoarseness, voice weakness, or even complete loss of voice (aphonia) due to pressure on nerves.
Dysphagia, difficulty swallowing.
Distended neck veins, especially in cases of fluid buildup or constriction.
Persistent abdominal or leg swelling in long-term pericarditis.
Diagnosis of Pericarditis
Medical history and physical examination: The doctor will inquire about your symptoms and medical history to identify potential risk factors. During the physical exam, listening to the heart sounds may reveal a pericardial rub, a scratching or grating sound caused by the inflamed layers rubbing together.
Laboratory tests: Blood and urine tests can help identify the underlying cause of the pericarditis, such as infection or inflammation markers.
Electrocardiogram (ECG): This test records the electrical activity of the heart and can show characteristic changes associated with pericarditis, indicating its effect on heart function.
Chest X-ray: This imaging technique can reveal the size and shape of the heart and may show signs of fluid accumulation around the heart.
Echocardiogram: Using ultrasound waves, this procedure provides a moving image of the heart, allowing doctors to assess the heart’s pumping ability and detect fluid buildup.
CT scan of the chest: This detailed imaging technique provides cross-sectional views of the heart and surrounding structures. It can be particularly useful in identifying constrictive pericarditis and ruling out other heart conditions.
MRI scan of the chest: Another advanced imaging technique that can be used if other imaging results are unclear, providing detailed anatomical information.
Management and Treatment of Pericarditis
Treatment strategies for pericarditis are tailored to the underlying cause. Some mild cases may resolve spontaneously without specific intervention.
1. Medication Therapy: Various medications can be used to manage the symptoms and inflammation associated with pericarditis.
Analgesics: Pain relievers are frequently prescribed to alleviate the chest pain.
Anti-gout medication: Certain medications used for gout can also be effective in pain management for pericarditis.
Corticosteroids: These powerful anti-inflammatory drugs are often used to reduce pericardial inflammation.
2. Pericardiocentesis: This procedure involves inserting a needle into the pericardial sac to drain excess fluid. It is typically guided by ultrasound imaging for precision.
3. Pericardiectomy: This surgical procedure involves the removal of the pericardium. It is usually reserved for severe cases of constrictive pericarditis where the thickened pericardium is severely restricting heart function.
Nursing Interventions
Regularly assess and document the patient’s pain level, evaluating within 30 minutes of intervention.
Administer prescribed pain medications, such as morphine, to provide pain relief.
Continuously monitor the patient’s pain level and the effectiveness of administered analgesics.
Help the patient find a comfortable position, often sitting up and leaning forward.
Monitor and record vital signs regularly.
Educate the patient about the disease process, its signs, and symptoms, including those of expanding or impending aneurysm (if relevant as a differential).
If surgery is necessary, provide emotional support and prepare the patient for the procedure.
For post-operative patients, educate them about warning signs of complications like fever, surgical site inflammation, bleeding, and swelling.
Monitor the patient’s weight daily to track fluid balance.
Closely monitor and report persistent cough, vomiting, or a systolic blood pressure above 180 mmHg to the physician due to the increased risk of hemorrhage.
Ensure the patient rests in bed until fever, chest pain, and pericardial friction rub have resolved.
Administer supplemental oxygen as needed to maintain an oxygen saturation level above 90%.
Administer prescribed medications, such as NSAIDs and steroids, with food to minimize gastric irritation.
Ensure antibiotics are administered on schedule.
Continue intravenous antihypertensive medications if high blood pressure persists.
Meticulously track fluid intake and output.
Reassure the patient that their chest pain is not caused by a myocardial infarction (heart attack) to reduce anxiety.
Assess for signs and symptoms of cardiac tamponade at least every 8 hours and as needed (PRN).
Assist the patient with personal hygiene, such as bathing, if necessary.
Advise the patient to gradually resume their daily activities.
Establish a positive and trusting relationship with the patient to alleviate anxiety.
In cases of cardiac tamponade, open surgical drainage is often the preferred treatment.
Nursing Diagnosis
Hyperthermia related to the disease process of bacterial pericarditis, as evidenced by a temperature of 38.0 degrees Celsius, rapid breathing, profuse sweating, and chills.
Alteration in comfort related to chest pain due to pericardial inflammation, as evidenced by facial grimacing.
Decreased cardiac output related to pericarditis, as evidenced by fatigue and inability to perform Activities of Daily Living as normal.
Alteration in comfort related to chest pain due to pericardial inflammation, as evidenced by clutching of hands or chest.
Acute Pain related to the inflammatory process of bacterial pericarditis, as evidenced by a chest pain score of 10 out of 10, guarding sign, and shortness of breath.
Altered tissue perfusion related to tissue ischemia, as evidenced by abnormal hemodynamic readings.
Activity intolerance related to acute chest pain, as evidenced by fatigue, disinterest in activities of daily living due to pain, verbalization of tiredness, and generalized weakness.
Anxiety related to threat to body image, as evidenced by decreased energy, irritability, crying, and feelings of helplessness.
Complications of Pericarditis
Constrictive Pericarditis: This is a serious long-term complication where the inflamed pericardium becomes stiff, scarred, thickened, and adheres to itself, restricting the heart’s ability to function properly.
Pericardial Effusion: Rapid accumulation of fluid in the pericardial sac can lead to cardiac tamponade, a life-threatening compression of the heart that severely impairs its pumping action.
Cardiac tamponade: As mentioned above, this is a critical condition caused by fluid buildup compressing the heart.
Pericardial effusion: This refers to the buildup of fluid in the space surrounding the heart, which can lead to tamponade if it occurs rapidly.
Myocardial ischemia: Reduced blood flow to the heart muscle can occur due to the inflammatory process or compression, preventing the heart from receiving enough oxygen.
Stroke: Although less direct, in severe cases, complications affecting the heart’s function could potentially impact blood flow to the brain, leading to a stroke (brain attack).
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

