Surgical Nursing (III)
Subtopic:
Peritonsillar
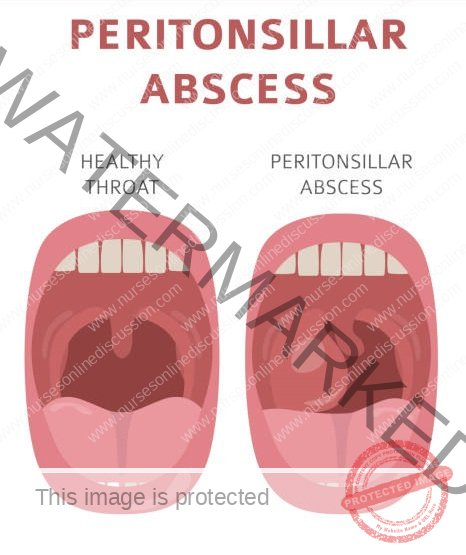
PERITONSILLAR ABSCESS
Peritonsillar Abscess (Quincy) is characterized as a localized collection of pus situated in the space between the tonsil’s outer layer (capsule) and the side wall of the pharynx (throat).
Peritonsillar abscess (Quincy) arises from a bacterial infection, most commonly involving streptococcal bacteria. It typically develops as a complication stemming from inadequately treated tonsillitis, which can initially be mild.
It manifests as a pocket filled with pus forming adjacent to one of the tonsils. Essentially, it’s an accumulation of pus in the tissues surrounding the tonsil.
This condition usually starts as a consequence of an untreated streptococcal infection in the throat or an episode of tonsillitis.
If left unaddressed, the infection has the potential to spread deeper into the neck and chest. This is a less frequent occurrence in adults.
CAUSES OF PERITOSILLAR ABSCESS
Peritonsillar abscesses typically develop as a complication of tonsillitis. When the infection breaches the tonsil itself and extends into the surrounding tissues, an abscess can form. The incidence of peritonsillar abscesses has decreased due to the widespread use of antibiotics in treating strep throat and tonsillitis.
These abscesses are caused by various bacteria, including:
Streptococcus pyogenes: This is the same bacterium responsible for both strep throat and tonsillitis.
Fusobacterium necrophorum: This bacterium can also cause infections like mastoiditis (infection of the mastoid bone), sinusitis (inflammation of the sinuses), and meningitis (inflammation of the membranes surrounding the brain and spinal cord).
Staphylococcus species of bacteria.
Haemophilus species of bacteria.
Mononucleosis (commonly known as mono), an infectious illness, can also predispose individuals to peritonsillar abscesses. Additionally, infections originating from teeth and gums can sometimes lead to this condition. In rarer instances, peritonsillar abscesses can develop without a preceding infection, typically due to inflammation of the Weber glands. These glands are located beneath the tongue and are responsible for producing saliva.
CLINICAL PRESENTATION
Trismus: Difficulty or inability to open the mouth fully.
Severe throat pain: Intense pain localized in the throat region.
Dysphagia: Difficulty swallowing.
Bad mouth odor (Halitosis): Unpleasant smell emanating from the mouth.
Ptyalism (excessive salivation): Increased production of saliva.
Thickened muffled speech: Speech that sounds unclear or as if the person is talking with something in their mouth.
Ear pain: Pain in the ear, potentially referred pain from the throat.
Fever, headache, malaise, rigors: Systemic symptoms including elevated temperature, pain in the head, a general feeling of discomfort, and shaking chills.
Enlarged cervical lymph nodes: Swollen lymph nodes in the neck region.
Tonsil and soft palate are reddish & edematous: The tonsil and the soft part of the roof of the mouth appear red and swollen.
Swelling pushing the uvula to opposite side: The swelling can displace the uvula (the fleshy extension at the back of the throat) to the unaffected side; there may be a visible bulge indicating the pus collection.
Otalgia (earache): Pain in the ear.
Difficult in swallowing: Problems with the process of swallowing.
Impaired speech: Difficulty articulating words clearly.
Swelling of the neck and face: Visible swelling in the neck and facial area.
Difficulty swallowing saliva (drooling): Inability to manage saliva in the mouth, leading to drooling.
Swelling of the face or neck: Noticeable swelling in the facial or neck regions.
Investigations
Physical Examination: A careful examination of the throat, neck, and inside of the mouth is crucial for identifying a potential abscess. The physician will look at the tonsils for swelling and redness, and check for the presence of pus or a fluctuant area (feeling of fluid underneath the surface).
Throat Swab: A sterile swab is used to collect a sample from the throat. This sample is then tested to identify the specific bacteria causing the infection, which helps in choosing the most effective antibiotic.
Complete Blood Count (CBC): This blood test measures different components of the blood, including white blood cells. An elevated white blood cell count typically indicates the body is fighting an infection.
Ultrasound: This imaging technique uses sound waves to create pictures of the inside of the body. It can be used to visualize the abscess, determine its size, and confirm its location, helping to distinguish it from other throat conditions.
CT Scan: A more detailed imaging test that uses X-rays to create cross-sectional images of the neck. It provides a comprehensive view, allowing doctors to see the precise location and extent of the abscess.
Blood Cultures: A blood sample is taken and tested to see if bacteria are present in the bloodstream. This is particularly important in severe cases to identify the specific bacteria and guide antibiotic treatment.
Management Of Peritonsillar Abscess
Aims:
To drain the abscess: The primary goal is to remove the collection of pus.
Promote healing by relieving symptoms & treating the cause: To alleviate pain and discomfort while addressing the underlying infection.
Prevent complications: To avoid further spread of infection or other serious issues.
Admission
The patient is typically admitted to a surgical ward and advised to have complete bed rest.
Initial vital signs (temperature, pulse, blood pressure, respiration rate) are recorded to establish a baseline.
In severe cases where the patient’s breathing is compromised, supplemental oxygen therapy is provided.
Pain is managed using analgesic medications such as diclofenac (75 mg) or tramadol (50 mg) as an initial measure.
A thorough general and systemic examination is performed to identify any other coexisting health problems.
An intravenous (IV) line is inserted to administer fluids and medications directly into the bloodstream. Intravenous fluids, such as dextrose alternating with normal saline, are given to maintain proper hydration.
Antibiotics, like penicillin, may be administered intravenously to start combating the infection before any surgical intervention.
PRE-OPERATIVE CARE
The medical team explains the planned procedure to the patient to reduce anxiety and ensure understanding.
Obtaining informed consent from the patient is essential before proceeding with any surgical intervention.
A nasogastric tube (NGT) may be inserted through the nose into the stomach to facilitate feeding after the surgery, especially if swallowing is expected to be difficult.
Oral care is performed to reduce the number of bacteria in the mouth, minimizing the risk of post-operative infection.
IN OPERATING THEATRE
Incision and drainage of the abscess is performed: A surgical cut is made into the abscess to allow the pus to drain out.
Tonsillectomy may be performed: This involves the surgical removal of the tonsils, which can be done at the same time as the drainage (simultaneous tonsillectomy with open abscess drainage) and may involve oral packing to control bleeding.
ON WARD
Suction is used to clear oral secretions, preventing aspiration (inhaling secretions into the lungs).
Fluid resuscitation with IV normal saline is administered as needed to maintain hydration.
Anti-pyretic medications (to reduce fever) and analgesic medications (for pain relief) are prescribed and administered.
Precautions are taken to prevent bleeding, including gentle handling of the patient and advising them to avoid actions that increase pressure in the surgical area, such as excessive coughing, laughing, or opening the mouth too wide.
Once tolerated, soft foods and liquids can be gradually introduced.
Maintaining good oral hygiene is essential until complete recovery.
Antibiotics are administered as prescribed to eradicate the remaining infection.
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are given to help control inflammation and fever.
Common antibiotic regimens include intravenous benzyl penicillin (2 million units every 6 hours for 48 hours, followed by oral amoxicillin 500mg three times a day for 7 days) or an alternative like intravenous ceftriaxone (1 gram once daily for 7 days; for children, the dose is typically 50mg/kg intravenously).
Intravenous metronidazole (500mg every 8 hours) may be added to cover anaerobic bacteria. If the patient cannot take fluids orally, an IV drip of normal saline is initiated.
Routine daily nursing care is provided until the patient is well enough to be discharged.
Advice:
Seeking early medical treatment for streptococcal throat infections can help prevent complications like peritonsillar abscess.
Maintaining good oral hygiene practices can reduce the risk of infections in the mouth and throat.
NURSING CARE PLAN.
Assessment: Difficulty opening mouth, excessive saliva and drooling, intense sore throat, trouble swallowing, halitosis (bad breath), ptyalism (overproduction of saliva), and slurred speech.
Diagnosis: Compromised Oral Mucosa Integrity linked to peritonsillar abscess, indicated by swallowing difficulty, altered speech, excessive salivation, and halitosis.
Planning (Goals/Expected Outcomes): Sustain oral cleanliness and lessen discomfort.
Implementation:
Give antibiotics and pain relievers as ordered.
Promote consistent oral hygiene practices, including mild saline rinses.
Apply pain relief measures (e.g., cool packs).
Rationale:Antibiotics combat bacterial infection source.
Consistent oral hygiene minimizes secondary infections and increases comfort.
Pain management strategies decrease discomfort levels.
Evaluation: Oral hygiene sustained, discomfort lessened.
Assessment: Elevated temperature, headache, general discomfort, chills, swollen neck lymph nodes.
Diagnosis: Hyperthermia secondary to systemic infection, as shown by elevated temperature, general discomfort, headache, and chills.
Planning (Goals/Expected Outcomes): Lower temperature and enhance comfort.
Implementation:
Give fever-reducing medication as directed.
Ensure sufficient fluid intake.
Implement cooling techniques (e.g., lukewarm sponge bath).
Rationale:Fever reducers work to decrease temperature.
Sufficient fluids prevent dehydration risks.
Cooling methods help lower body temperature.
Evaluation: Temperature decreased, comfort improved.
Assessment: Uvula displaced due to swelling, ear pain, and difficulty swallowing.
Diagnosis: Compromised Swallowing Function related to swelling and pain, indicated by swallowing difficulty and drooling.
Planning (Goals/Expected Outcomes): Enhance swallowing ability and lessen pain.
Implementation:
Recommend small, regular meals and drinks.
Administer pain medication as ordered.
Track and document fluid intake and output.
Rationale:Smaller, frequent meals ease swallowing.
Pain relievers decrease pain levels.
Monitoring fluids prevents dehydration problems.
Evaluation: Swallowing ability enhanced, pain lessened.
Assessment: Neck and facial swelling observed.
Diagnosis: Body Image Disturbance related to noticeable swelling, as indicated by patient distress.
Planning (Goals/Expected Outcomes): Bolster patient’s self-image and confidence.
Implementation:
Offer emotional support and encourage verbalization of feelings.
Inform patient that swelling is temporary.
Work with healthcare team to explore options for reducing visible swelling.
Rationale:Emotional support and education lessen anxiety and distress.
Knowing swelling is temporary helps patient manage expectations.
Investigating interventions demonstrates dedication to addressing patient worries.
Evaluation: Improved self-image and confidence.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

