Pediatric Conditions of the Cardiovascular System
Subtopic:
Sickle Cell Disease/Sickle Cell Anaemia
Sickle cell disease is a genetic condition affecting red blood cells, causing the body to produce red blood cells that are abnormally shaped and can lead to various health problems.
Sickle cell disease is passed down through families as an autosomal recessive trait. This means that a child must inherit two copies of the faulty gene, one from each parent, to develop the disease. In this condition, the normal type of adult hemoglobin, hemoglobin A, is replaced by an abnormal type called hemoglobin S.
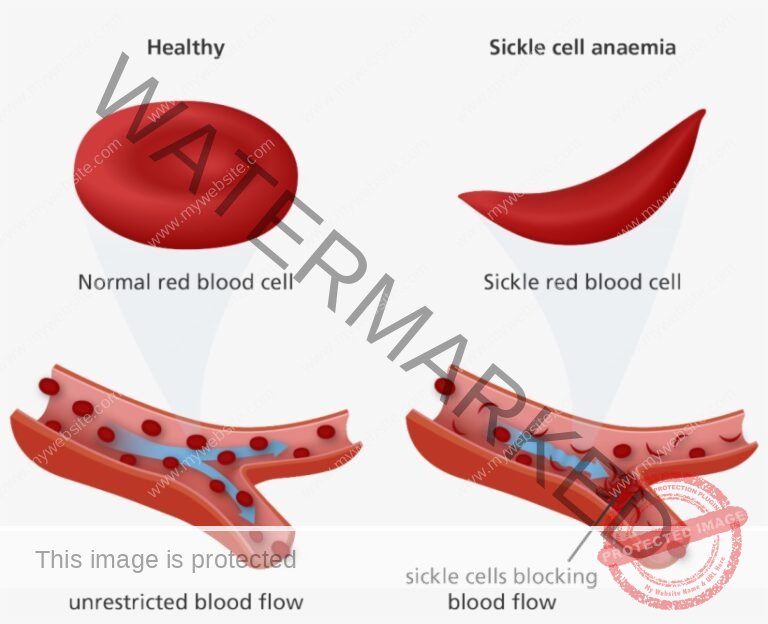
Children with sickle cell disease have an altered form of hemoglobin, known as hemoglobin S. This abnormal hemoglobin causes the typically round and flexible red blood cells to become stiff and assume a crescent or sickle shape.
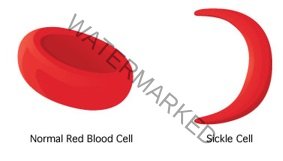
Normal red blood cells, containing normal hemoglobin, have a smooth, round, and flattened disc-like shape, similar to a doughnut without a hole in the middle. Their flexible nature allows them to easily navigate through even the smallest blood vessels.
In contrast, red blood cells containing sickle cell hemoglobin become rigid and adhesive. When these cells release oxygen, the abnormal hemoglobin inside causes them to distort into a sickle or crescent shape, resembling the letter C. These sickle-shaped cells tend to clump together and lose their ability to flow smoothly through blood vessels. This stickiness and irregular shape can obstruct the flow of blood through the smaller vessels, hindering the delivery of oxygenated blood to tissues and potentially causing pain.
Sickle cell disease is generally categorized into the following types:
1. Sickle Cell Anaemia (Homozygous): Individuals with this form of the disease have red blood cells containing only the abnormal beta globin chains, resulting in HbSS (SS) hemoglobin. This is commonly referred to as sickle-cell anaemia, and those affected exhibit the full range of signs and symptoms associated with the condition. A person with sickle cell anaemia inherits two copies of the mutated hemoglobin gene, one from each parent. This genetic makeup is represented as HbSS or SS. Other terms used to describe this condition include: HbSS, SS disease, Haemoglobin S.
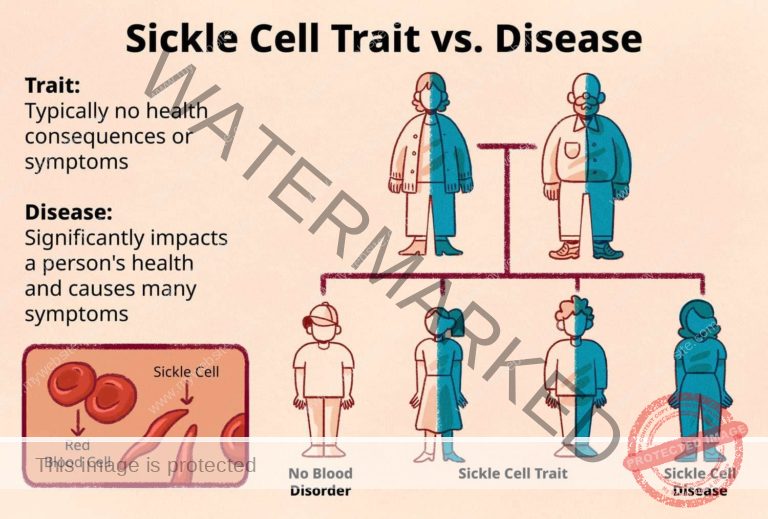
2. Sickle Cell Trait (Heterozygous): In this case, a person’s red blood cells contain a mix of both normal beta globin chains (HbA) and abnormal beta globin chains (HbS). Consequently, their hemoglobin is a combination of both HbA and HbS (HbAS). Someone with sickle cell trait inherits a single copy of the normal hemoglobin gene from one parent and one copy of the faulty hemoglobin gene from the other parent. This genetic combination is denoted as HbAS. People with sickle cell trait are typically asymptomatic, meaning they usually do not show the characteristic symptoms of sickle cell disease. They are considered carriers of the mutated gene and have the potential to pass it on to their offspring.
To understand Homozygous and Heterozygous:
SCD (Sickle Cell Disease): Think of SCD as a problem arising from faulty genetic instructions for building red blood cells. Imagine it like a construction manual with errors that should guide the making of strong, healthy red blood cells (the “bricks” of your blood). These errors lead to red blood cells that are misshapen and don’t function properly.
Autosomal: This term relates to the autosomes, which are the chromosomes responsible for most of your traits, excluding those related to sex determination (male or female). Picture these chromosomes as the foundational structure of a house.
Heterozygous: Every individual has two copies of each autosome, inheriting one from each parent. Imagine receiving one instruction manual with correct instructions from one parent and another manual with errors from the other. This means you possess one normal copy and one faulty copy of the gene associated with sickle cell disease. As a result, you are a “carrier” of the faulty gene but do not have sickle cell disease itself.
Homozygous: This indicates that you’ve received the same version of the gene from both parents. There are two possibilities here:
Homozygous dominant: You inherited two normal instruction manuals (one from each parent). Your red blood cells are built correctly, and you do not have sickle cell disease.
Homozygous recessive: You inherited two faulty instruction manuals (one from each parent). This leads to significant problems with your red blood cells, and you have sickle cell disease.
Recessive: A recessive gene will only cause a disease if an individual has two copies of the faulty gene (as seen in the homozygous recessive scenario). Think of it as needing two incorrect instruction manuals to build a house with problems.
Dominant: A dominant gene will cause a disease even if only one faulty copy is present (as in the heterozygous case). Imagine the faulty instruction manual overriding the correct one.
Summary:
SCD: Errors in the genetic instructions cause problems with red blood cells.
Autosomal: Relates to the non-sex chromosomes that determine most traits (the house’s foundation).
Heterozygous: Having one normal and one faulty copy of a gene (one correct and one faulty instruction manual).
Homozygous: Having two identical copies of a gene (two correct or two faulty instruction manuals).
Recessive: Two faulty copies of a gene are needed for the disease to be present (two faulty instruction manuals to build a bad house).
Dominant: Only one faulty copy of a gene is needed for the disease to be present (one faulty instruction manual is enough to build a bad house).
Red Blood Cells: These cells are responsible for carrying oxygen throughout the body.
Haemoglobin: This is the protein within red blood cells that binds to oxygen.
Haemoglobin Gene: This gene, located on chromosome 11, provides the instructions for making haemoglobin.
Possibility of Sickle cell Disease
Problems associated with sickle cell disease typically begin around 5 to 6 months of age. This timing is related to the decreasing levels of fetal hemoglobin in the infant’s blood. Sickle-cell disease develops when an individual inherits two copies of the abnormal haemoglobin gene, one from each parent. This gene is located on chromosome 11.
| Type of Gene Inheritance | Chance of Normal Trait | Chance of Being a Carrier (with Trait) | Chance of Having the Disease |
| One Parent with Trait | 50% | 50% | 0% |
| Both Parents with Trait | 25% | 50% | 25% |
| One Parent with Disease | 0% | 50% | 50% |
| Both Parents have Disease | 0% | 0% | 100% |
Cause of Sickle Cell Disease
The underlying cause of sickle cell disease is a defect in the beta globin chains of hemoglobin. Specifically, a particular amino acid is replaced by another (substitution of valine for glutamic acid) at position 6 of the chain. This substitution leads to the production of abnormal hemoglobin known as HbS.
In simpler terms, sickle cell disease arises from a genetic change, or mutation, in the gene responsible for producing haemoglobin, the protein in red blood cells that carries oxygen.
Normal Haemoglobin: Normal adult haemoglobin (HbA) is composed of two alpha globin chains and two beta globin chains.
Sickle Cell Haemoglobin: In sickle cell disease, a single change occurs within the genetic code for the beta globin chain. This is a point mutation where the instructions to include glutamic acid at position 6 are replaced with instructions to include valine. This altered haemoglobin is called HbS.
Pathophysiology of Sickle Cell Disease.
Normally, each haemoglobin molecule comprises four heme molecules (containing iron) attached to one molecule of globin (protein).
However, in sickle cell disease, this structure is altered, causing red blood cells to adopt a sickle shape. This shape change occurs because glutamic acid is replaced by valine in the hemoglobin molecule. These sickle-shaped cells become elongated when oxygen levels are low, in conditions of acidosis, or during dehydration.
When red blood cells (RBCs) containing only the abnormal HbS (homozygous HbS) are in environments with reduced oxygen, the sickling process is initiated. This process distorts the cell membranes, making the cells more likely to stick together. This clumping leads to increased blood viscosity, causing vessel occlusion (blockage) and subsequent tissue necrosis (tissue death due to lack of blood supply).
Importantly, these sickled cells often fail to return to their normal shape even when normal oxygen levels are restored. As a consequence, these rigid blood cells are unable to squeeze through narrow capillaries, leading to further blockage of blood vessels and ischemia (reduced blood flow) to tissues. The anaemia associated with sickle cell disease is a result of haemolysis, the premature destruction of these abnormally shaped red blood cells.
Although the bone marrow attempts to compensate for this destruction by producing new red blood cells, the rate of production cannot keep pace with the rate of destruction. While healthy red blood cells typically survive for 90–120 days, sickled cells only last for about 10–20 days. Additionally, increased trapping (sequestration) of red blood cells in the spleen also contributes to the development of anaemia.
Clinical Presentation of SCD
Children with sickle cell disease are often asymptomatic early in life, typically until later in the first year. This is because they still have higher levels of fetal haemoglobin, which protects red blood cells from sickling. The severity of symptoms can vary considerably among individuals with SCD. The disease can lead to a range of both acute and chronic complications, some of which can be life-threatening.
Common signs and symptoms include:
Painful swelling of hands and feet (Hand-foot syndrome): This is a frequent early sign in children, resulting from vaso-occlusive crises affecting the small blood vessels in the hands and feet.
Pain crisis (sickle crisis): A hallmark of the disease, characterized by episodes of intense pain caused by blocked blood flow to specific areas of the body. These crises can last for days or even weeks. Pain can be experienced in the chest, abdomen, limbs, and joints.
Anaemia: A consistent feature of SCD due to the shortened lifespan of sickled red blood cells. This leads to persistent fatigue, weakness, and paleness.
Jaundice: A yellowish discoloration of the skin and eyes, caused by the breakdown of red blood cells and the release of bilirubin.
Haemoglobin levels: Typically low, ranging from 6 g/dL to 9 g/dL, reflecting the severity of the anaemia.
Shortness of breath: Can arise from complications such as pneumonia, acute chest syndrome, and pulmonary hypertension.
Fatigue and weakness: Common symptoms due to the reduced oxygen-carrying capacity of the blood.
Priapism: A prolonged and painful erection, lasting for hours or days, caused by blocked blood flow in the penis. If not treated promptly, it can lead to impotence.
Abdominal swelling and pain: Often associated with enlargement of the spleen (splenomegaly) or blockages in the blood vessels supplying the intestines.
Unusual headache: May be a warning sign of stroke, as sickled cells can obstruct blood flow to the brain.
Loss of appetite: A frequent symptom linked to anaemia and pain.
Irritability: Can be a consequence of pain, fatigue, and other discomforts.
Bossing of the bones of the skull: An indication of increased red blood cell production (erythropoiesis) in the bone marrow to compensate for the destruction of sickle cells.
Intercurrent infections: Individuals with sickle cell disease are more susceptible to various infections, including pneumonia, acute respiratory infections, and malaria, which can be further complicated by severe anaemia.
Splenomegaly: Enlargement of the spleen is common in younger children but often the spleen shrinks and becomes damaged (splenic infarction) in older children.
Growth retardation: Can occur due to chronic illness, recurrent pain, and infections.
Stroke: A severe complication resulting from blocked blood flow to the brain, potentially causing permanent brain damage.
Newborns: May present with jaundice, delayed umbilical cord separation, and potential failure to thrive.
Clinical presentations at different ages:
Children:
Dactylitis (Hand-foot Syndrome): Painful swelling of the hands and feet is a common early sign.
Splenomegaly: Often present in younger children but may be absent in older children due to splenic damage.
Delayed growth and development: Are common due to recurrent infections and pain episodes.
Delayed puberty: Can occur, particularly in males.
Adults:
Chronic pain: A significant and often unpredictable feature of the disease.
Pulmonary complications: Pulmonary hypertension, acute chest syndrome, and pneumonia are frequent issues.
Osteonecrosis: Damage to bone tissue due to insufficient blood supply.
Avascular necrosis: Can affect bones, especially the hips and shoulders.
Chronic kidney disease: Can develop over time due to repeated damage to the kidneys.
Chronic Symptoms:
Jaundice: Persistent yellowing of the skin and eyes due to red blood cell breakdown.
Gallstones: Formation of stones in the gallbladder, often due to increased bilirubin from red blood cell destruction.
Progressive kidney impairment: Damage to blood vessels in the kidneys can lead to reduced kidney function over time.
Growth retardation: Slower growth of long bones and skeletal deformities, particularly in the spine, can occur.
Delayed puberty: The chronic illness can delay the onset of puberty.
Chronic painful leg ulcers: Related to chronic anaemia and poor blood flow to the extremities.
Decreased lifespan: While medical advancements have improved life expectancy, individuals with sickle cell disease still tend to have a shorter lifespan compared to the general population.
Altered body structures: These can include “bossing” of the skull (abnormal thickening of the skull bones) and septic necrosis (bone death due to infection) in the femur (thigh bone) and the head of the humerus (upper arm bone).
Sickle-cell crisis
A sickle cell crisis refers to episodes of sudden, severe pain that can last for several hours to several days.
The terms “sickle-cell crisis” or “sickling crisis” are often used to describe various acute conditions that can occur in individuals with Sickle Cell Disease. It happens when the misshapen red blood cells block small blood vessels that supply blood to the bones. Children experiencing a sickle cell crisis may complain of pain in the back, knees, legs, arms, chest, or stomach. The pain can be described as throbbing, sharp, dull, or stabbing.
Types of Sickle Cell Crisis.
(i) Vaso-occlusive Crisis: This is the most common type of sickle cell crisis. The sickle-shaped cells obstruct small blood vessels, leading to a lack of blood flow (ischemia) and tissue damage (infarction) in the affected area. This causes pain, swelling, and inflammation.
Symptoms: Intense pain in the bones, joints, abdomen, chest, or head. Other symptoms may include fever, fatigue, and shortness of breath.
Extremities: Bone damage can occur, leading to osteoporosis (weakening of bones) or ischaemic necrosis (bone death due to lack of blood supply).
Foot and hand syndrome (Dactylitis): This is due to lack of blood flow (aseptic infarction) in the small bones of the hands and feet (metacarpals and metatarsals), causing swelling and pain. It is often seen in infants and toddlers.
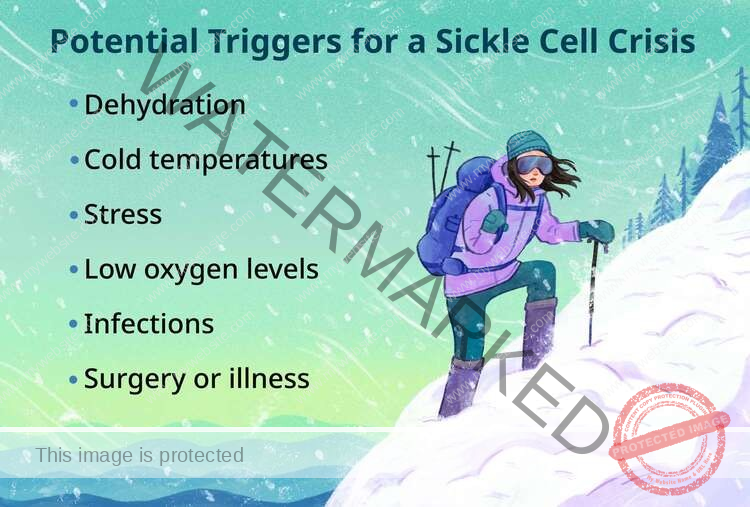
Triggers: Factors that can trigger a vaso-occlusive crisis include dehydration, infection, cold weather, high altitude, and strenuous physical activity.
Treatment: Focuses on pain management with analgesics, providing intravenous fluids, and, in severe cases, blood transfusions.
(ii) Splenic sequestration Crisis: In this type of crisis, a large volume of blood becomes trapped within the spleen, leading to a significant decrease in circulating blood volume and a drop in blood pressure. The spleen becomes markedly enlarged.
Symptoms: Abdominal pain, swelling, fever, and signs of shock. A rapid and significant decrease in red blood cell mass occurs within hours. Signs of circulatory collapse can develop quickly.
This type of crisis is a leading cause of death in infants with sickle cell disease.
Treatment: Requires immediate medical attention, including intravenous fluids, blood transfusions, and, in some cases, surgical removal of the spleen (splenectomy).
(iii) Aplastic Crisis: This occurs when the bone marrow temporarily stops producing red blood cells, leading to a sudden and severe drop in the red blood cell count (anaemia) and a worsening of symptoms.
Cause: Aplastic crises are often triggered by viral infections, such as parvovirus B19. Other causes include folic acid deficiency and exposure to substances toxic to the bone marrow (e.g., phenylbutazone).
Symptoms: Fatigue, weakness, paleness (pallor), and shortness of breath.
Treatment: Primarily involves blood transfusions to increase the red blood cell count.
(iv) Haemolytic Crisis: A haemolytic crisis happens when red blood cells are destroyed at an accelerated rate, faster than the body can replace them.
Cause: Often triggered by infections.
Symptoms: Fatigue, pallor, jaundice, and dark urine.
Treatment: Includes blood transfusions and treatment of any underlying infections.
Causes of haemolysis (red blood cell destruction) can include:
A lack of specific proteins within red blood cells.
Autoimmune diseases.
Certain infections.
Defects in the haemoglobin molecules within red blood cells.
Defects in the proteins that form the internal structure of red blood cells.
Side effects of certain medications.
Reactions to blood transfusions.
(v) Acute chest syndrome: This is a serious complication affecting the lungs. It occurs when sickle-shaped red blood cells block blood flow to the lungs, causing inflammation and damage. It can be life-threatening. It often develops suddenly, especially when the body is under stress due to infection, fever, or dehydration.
Symptoms: Chest pain, fever, shortness of breath, cough, and rapid breathing.
Treatment: Involves oxygen therapy, antibiotics, pain management, and, in some cases, mechanical ventilation to support breathing.
Precipitating Factors of Sickle Cell Crisis
Sickle cell crises, characterized by episodes of intense pain, are triggered when the abnormally shaped red blood cells obstruct blood flow within the body. Several factors can contribute to these painful events, which can be broadly categorized:
Environmental and Physiological Factors:
Dehydration: Insufficient fluid intake leads to a concentration of the blood, making it more viscous. This increased thickness makes it harder for the rigid sickle cells to navigate the narrow blood vessels, increasing the risk of blockages.
Infection: When the body fights off infections, there’s an increased demand for oxygen. This demand can place additional stress on the already compromised sickle red blood cells, making them more likely to sickle and cause blockages.
Trauma: Physical injury, even seemingly minor cuts or bruises, can initiate localized blood clotting. In individuals with sickle cell disease, this can trigger a vaso-occlusive crisis at the site of the injury.
Extreme Temperature Fluctuations: Significant changes in temperature, whether extreme heat or cold, can cause blood vessels to narrow (vasoconstriction). This constriction can impede blood flow and increase the likelihood of blockages by sickle cells.
High Altitude: At higher elevations, the air has a lower concentration of oxygen. This reduced oxygen availability (hypoxia) can directly trigger the sickling of red blood cells.
Hypoxia: Low oxygen levels in the blood, regardless of the cause, are a primary trigger for red blood cell sickling. This could be due to lung conditions or other factors affecting oxygen intake.
Acidosis: An increase in the acidity of the blood can alter the hemoglobin molecule in red blood cells, promoting the sickling process.
Lifestyle and Emotional Factors:
Strenuous Physical Exercise: Intense physical activity increases the body’s need for oxygen. This increased demand can outstrip the capacity of the abnormally shaped red blood cells to deliver oxygen efficiently, leading to sickling and potential crises.
Extreme Fatigue: Prolonged periods of exhaustion can weaken the body and its ability to cope with the conditions that trigger sickle cell crises.
Extreme Exertion: Similar to strenuous exercise, any form of intense physical effort can place undue stress on the body and trigger a crisis.
Emotional Stress: When the body experiences emotional stress, it releases hormones that can cause blood vessels to constrict. This vasoconstriction can impede blood flow and increase the risk of a sickle cell crisis.
Other Contributing Factors:
Pregnancy: The physiological changes during pregnancy, including an increase in blood volume and hormonal shifts, can make women with sickle cell disease more susceptible to experiencing crises.
Asthma: The inflammatory processes associated with asthma can contribute to conditions within the body that trigger sickle cell crises.
Anxiety: Similar to emotional stress, anxiety can trigger physiological responses, including vasoconstriction, that increase the risk of a sickle cell crisis.
Abrupt changes in temperature: Sudden shifts in environmental temperature can stress the body’s ability to regulate itself and potentially trigger a crisis.
Diagnosis and Investigations:
Family history: A significant factor in diagnosis, as sickle cell disease is inherited. A known family history of the condition strongly suggests the possibility of the disease.
Full blood count and peripheral film: A blood test that can show leukocytosis (an elevated white blood cell count), which may indicate a bacterial infection, and will allow for the visual identification of sickle-shaped red blood cells.
Haemoglobin estimation: A blood test that will typically reveal a low haemoglobin level (in the range of 6-8 g/dL), indicating anaemia. A high reticulocyte count (10-20%) suggests the bone marrow is actively trying to produce more red blood cells to compensate for their destruction.
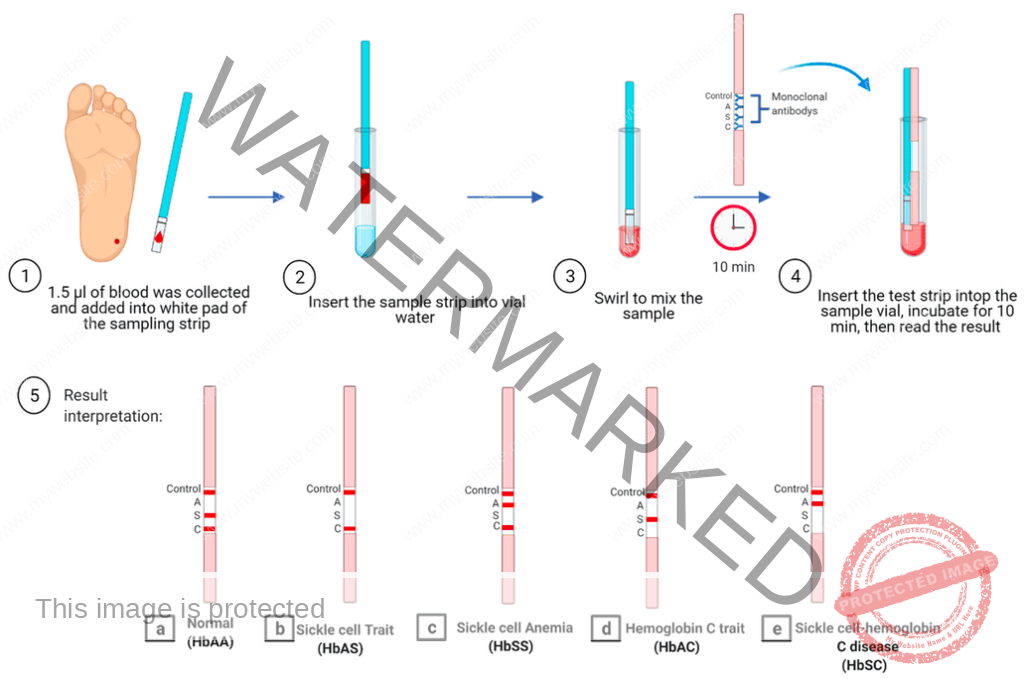
Sickling test: A straightforward screening test where a drop of blood, usually taken from a finger or heel prick, is observed under a microscope after being treated to remove oxygen. The presence of sickle-shaped cells indicates a problem with haemoglobin. However, this test cannot differentiate between sickle cell trait and sickle cell disease or other related conditions.
Haemoglobin electrophoresis: A more precise laboratory test that separates different types of haemoglobin based on their electrical charge. This test can definitively identify the presence and amount of HbS (sickle haemoglobin), providing a clear diagnosis of both sickle cell trait and sickle cell disease.
Sickledex test: A quick screening test used to detect the presence of HbS in a blood sample.
Peripheral blood smear: A blood sample is examined under a microscope to directly observe the shape of the red blood cells, identifying sickle cells and immature red blood cells (reticulocytes).
Urinalysis: A urine test to check for any signs of kidney damage, a potential complication of sickle cell disease.
Liver and renal function tests: Blood tests to assess how well the liver and kidneys are functioning.
Chest radiography: An X-ray of the chest, used to diagnose Acute Chest Syndrome, a serious lung complication.
Abdominal ultrasound: An imaging technique that can help identify problems within the abdomen, such as a mesenteric crisis (blockage of blood vessels supplying the intestines).
Sickling test (emergency screening): May be rapidly performed before surgical procedures to identify individuals who might have sickle cell disease.
Differential Diagnosis
It’s important to consider other conditions that may present with similar symptoms:
Acute anaemia
Carotid-Cavernous Fistula (CCF)
haemoglobin C Disease
Hemolytic Anaemia
Osteomyelitis in Emergency Medicine
Pulmonary Embolism (PE)
Rheumatoid Arthritis Hand Imaging
Septic Arthritis
Management of Sickle Cell Disease.
Management strategies are tailored to the specific type of crisis or the individual’s needs.
Aims of Management:
Avoiding pain episodes: Taking steps to minimize the occurrence of sickle cell crises.
Relieving symptoms: Providing treatment to alleviate the discomfort and complications of the disease.
Preventing complications: Implementing measures to reduce the risk of long-term health problems.
Acute painful attacks require supportive therapy including intravenous fluids to maintain hydration, oxygen if oxygen levels are low, antibiotics to treat any underlying infections, and appropriate pain relief.
Crises can cause severe pain that often necessitates strong pain relievers, typically narcotic analgesia. Morphine is often the preferred choice. For milder pain, codeine, paracetamol (acetaminophen), and NSAIDs (nonsteroidal anti-inflammatory drugs) may be sufficient.
Oxygen Therapy: Providing supplemental oxygen helps to correct hypoxia (low oxygen levels) and ease associated symptoms.
Prophylaxis (preventative treatment) with penicillin given twice daily is generally recommended for children up to 5 years of age due to their less developed immune systems, making them more vulnerable to early childhood infections. Vaccination against pneumococcal bacteria and Haemophilus influenzae type B is also crucial.
Hydration: Maintaining good hydration by drinking plenty of fluids is vital to prevent the blood from becoming too thick, thus improving blood flow and reducing the risk of crises.
Blood Transfusions: Regular blood transfusions are used to increase the levels of healthy haemoglobin in the blood, thereby reducing the frequency of painful crises and other complications. Transfusions are specifically indicated for conditions like heart failure, stroke, acute chest syndrome, acute splenic sequestration, and aplastic crises.
Anaemia Transfusions should only be given when there is a clear medical need.
Transfusions are generally not recommended for patients with stable, chronic anaemia, those undergoing minor surgery, or those experiencing uncomplicated painful episodes.
Transfusion and potentially splenectomy (removal of the spleen) can be life-saving interventions for young children experiencing splenic sequestration. A thorough compatibility screen must always be performed before a blood transfusion.
Folic acid 5 mg daily is generally recommended for life to support red blood cell production.
Hydroxycarbamide (hydroxyurea), starting at a dose of 20 mg/kg, is a medication widely used to treat sickle cell anaemia. It works by increasing the production of fetal haemoglobin (Hb F), and its ability to reduce the number of neutrophils (a type of white blood cell) may also be beneficial. Clinical trials have shown that hydroxycarbamide can decrease the frequency of pain episodes and acute chest syndrome, as well as the need for blood transfusions.
Malaria prevention: Individuals with sickle cell disease are more susceptible to malaria, which is a common trigger for painful crises in malaria-prone regions. Therefore, for those living in malarial countries, anti-malarial chemoprophylaxis, such as monthly sulfadoxine-pyrimethamine, is recommended for life.
Pain management: A crucial aspect of care, tailored to the severity of the pain.
Home management for pain relief may include:
Paracetamol (acetaminophen): Adult dose is 1 g every 8 hours; for children, the dose is 10-15 mg/kg every 6-8 hours.
Ibuprofen: For children, the dose is 5-10 mg/kg every 8 hours; for adults, it’s 400-600 mg every 6-8 hours.
Diclofenac: Adult dose is 50 mg every 8 hours; for children older than 9 years and weighing over 35 kg, the dose is 2 mg/kg in 3 divided doses.
If pain is not controlled with the above, adding stronger pain relievers may be necessary:
Codeine: 30-60 mg every 6 hours (only for patients older than 12 years).
Tramadol: 50-100 mg every 6-8 hours (only for patients older than 12 years).
Oral morphine: 0.2-0.4 mg/kg every 4 hours, with reassessment of pain levels.
If pain remains uncontrolled, referral to a hospital is necessary.
At the hospital, stronger pain management options are available:
Morphine oral: Child and Adult dose is 0.3-0.6 mg/kg per dose, with reassessment.
Morphine Intravenously: Child dose is 0.1-0.2 mg/kg per dose; Adult dose is 5-10 mg per dose, with reassessment.
The use of laxatives, such as bisacodyl 2.5 mg to 5 mg orally, may be necessary to prevent constipation caused by morphine intake.
Cure:
The only therapy currently approved by the FDA that offers the potential to cure SCD is a bone marrow or stem cell transplant. However, this procedure is high-risk and can have serious side effects, including death. A successful transplant requires a close match between the donor and recipient, with siblings often being the best donors.
Lifestyle Modifications:
Regular Exercise: Moderate physical activity, as tolerated, can improve cardiovascular health and potentially reduce the risk of complications.
Stress Management: Techniques like relaxation, meditation, and yoga can be beneficial in managing stress levels, which can be a trigger for crises.
Healthy Diet: A balanced and nutritious diet rich in fruits, vegetables, and whole grains supports overall health.
Avoidance of Extreme Temperatures: Both excessive heat and cold can trigger crises.
Altitude Management: Individuals with sickle cell disease should avoid high altitudes to minimize the risk of hypoxia.
Surgery:
Bone Marrow Transplant: While offering a potential cure, it is a complex and risky procedure with limited availability.
Other Surgical Interventions: Surgery may be required to correct bone deformities or treat complications such as leg ulcers.
Support and Counseling:
Genetic Counselling: Provides essential information about the inheritance patterns of sickle cell disease and options for family planning.
Psychosocial Support: Offers emotional and practical assistance to help individuals cope with the challenges of living with the condition.
Patient Education: Empowers individuals to effectively manage their condition by providing knowledge about symptoms, triggers, and treatment choices.
Prevention of Sickle cell crisis.
Preventive measures are crucial for reducing the frequency and severity of sickle cell crises.
Hydration:
Drink plenty of water: Maintaining adequate hydration is key to ensuring proper blood flow and preventing red blood cells from sickling.
Carry a water bottle and sip water regularly throughout the day.
Avoid dehydration, particularly during exercise, in hot weather, or when traveling.
Temperature Management:
Avoid extreme temperatures: Both excessive heat and cold can trigger sickle cell crises.
Stay in air-conditioned environments during hot weather.
Dress in layers to adjust to changing temperatures.
Be aware of the risk of hypothermia in cold weather.
Altitude Management:
Avoid high altitudes: The reduced oxygen levels at high altitudes can worsen sickle cell symptoms.
Oxygen Management:
Avoid situations with low oxygen levels: Limit intense physical exertion, particularly in hot, humid, or high-altitude environments.
Practice proper breathing techniques during exercise.
Infection Prevention:
Vaccination: Receive all recommended vaccinations, including the pneumococcal vaccine, to protect against infections.
Wash your hands frequently with soap and water.
Use hand sanitizer when soap and water are not available.
Avoid close contact with individuals who are sick.
Practice safe food handling and preparation to prevent foodborne illnesses.
Routine Medical Care:
Yearly visits to an eye doctor: Regular eye exams are essential to monitor for signs of retinopathy, a serious complication of sickle cell disease.
Regular checkups with a haematologist: Follow your doctor’s recommendations for regular blood tests and monitoring.
Early intervention: Seek medical attention promptly for any unusual symptoms or signs of a sickle cell crisis.
Stress Management:
Practice stress-reducing techniques: Stress can be a trigger for sickle cell crises.
Engage in enjoyable activities like meditation, yoga, or spending time in nature.
Consider counselling or therapy for help managing stress.
Lifestyle Modifications:
Maintain a healthy weight: Obesity can worsen sickle cell symptoms.
Eat a balanced diet rich in fruits, vegetables, and whole grains.
Avoid smoking and excessive alcohol consumption.
Engage in regular exercise, but consult your doctor regarding safe levels.
Advocacy and Support:
Join a sickle cell support group: Connect with others living with sickle cell disease to share experiences and resources.
Nursing Diagnosis
These are examples of nursing diagnoses commonly associated with sickle cell disease:
Acute pain related to tissue hypoxia due to the clumping (agglutination) of sickled cells within blood vessels, as evidenced by patient verbalization of pain.
Risk for infection related to a compromised immune system.
Impaired Gas Exchange related to the reduced oxygen-carrying capacity of the blood, the shortened lifespan of red blood cells and their premature destruction, the abnormal structure of red blood cells, and their sensitivity to low oxygen levels (e.g., during strenuous exercise or at high altitudes), as evidenced by difficulty breathing.
Ineffective Tissue Perfusion related to the blood vessel blockage (vaso-occlusive) nature of sickling, as evidenced by changes in vital signs, diminished peripheral pulses and delayed capillary refill, general paleness (pallor), or decreased mental alertness.
Risk for Deficient Fluid Volume related to increased fluid needs due to factors like a high metabolic rate, fever, and inflammatory processes.
Acute Pain related to sickling within the blood vessels (intravascular sickling) leading to localized blood stagnation (stasis), blockage (occlusion), and tissue damage or death (infarction/necrosis), as evidenced by generalized pain described as throbbing or severe, affecting extremities, bones, joints, back, abdomen, or head (headaches).
Risk for Impaired Skin Integrity related to poor circulation (venous stasis and vaso-occlusion).
Prevention Of Sickle Cell Disease
Genetic counselling is important for individuals who are carriers of the sickle cell trait or have the disease, to understand the risks of passing it on to their children and to explore reproductive options.
Premarital counselling is encouraged to inform prospective partners about their carrier status and the potential for having children with sickle cell disease.
Early recognition/screening of children with low haemoglobin levels can help in the early diagnosis and management of sickle cell disease.
Complications of Sickle Cell anaemia
Sickle cell anaemia can lead to various complications affecting different parts of the body.
Stroke: Circulation problems caused by sickle cells blocking blood vessels can lead to thrombolytic strokes.
Acute chest syndrome: A serious complication characterized by chest pain, fever, and difficulty breathing, requiring immediate medical attention.
Pulmonary hypertension: This type of anaemia can cause high blood pressure in the lungs due to circulation problems caused by the clumping of red blood cells.
Organ damage: The chronic inability of the red blood cells to deliver enough oxygen can lead to organ failure, which can be life-threatening.
Blindness: Damage to small blood vessels, particularly in the eyes, due to abnormal red blood cells, can cause eye damage and eventual blindness.
Leg ulcers: Poor circulation and tissue damage can lead to slow-healing leg ulcers.
Gallstones: The breakdown of abnormal red blood cells releases bilirubin, which can accumulate and lead to the formation of gallstones that can block the flow of bile.
Priapism: Men with sickle cell anaemia may experience painful and prolonged erections (priapism) due to blockages in the small blood vessels of the penis.
Pregnancy complications: Sickle cell anaemia increases the risk of high blood pressure and the formation of blood clots, which can interfere with the normal development of the fetus.
NURSING CARE PLAN FOR A PATIENT WITH SICKLE CELL CRISIS
Assessment
Cyanosis observed
Breathlessness, respiratory rate at 28 breaths per minute
Restlessness
Oxygen saturation (SpO2) at 80%
Diagnosis
Impaired Gaseous Exchange related to elevated blood viscosity as evidenced by:
Cyanosis
Breathlessness
Restlessness
Low SpO2 (80%)
Goals/Expected Outcomes
Achieve sufficient gaseous exchange within 2 hours.
Increase SpO2 by 10% within the initial 30 minutes.
Establish a normal breathing pattern without assistance within 1 hour.
Restore typical skin color in 30 minutes.
Intervention
Initiate intravenous (IV) access and administer fluids:
Normal saline solution, 500 mL every 6 hours for a total of 24 hours.
Promote oral fluid intake.
Implement fluid input and output monitoring.
Evaluate the necessity for additional fluids after 24 hours based on patient status.
Monitor vital signs frequently:
Every 30 minutes for 2 hours, with specific attention to respiratory status and SpO2 levels.
Adjust interventions based on assessment findings.
Administer supplemental oxygen:
3 Liters per minute for 1 hour via face mask.
Rationale
Establishing IV access and fluid administration helps to decrease blood thickness and improve blood flow.
Encouraging oral hydration supports overall fluid balance.
Fluid balance monitoring aids in assessing hydration status.
Regular vital sign assessment allows for timely adjustments to the treatment plan.
Oxygen therapy enhances blood oxygen levels.
Evaluation
Patient appears calmer and more relaxed.
Breathing pattern normalized, respiratory rate at 20 breaths per minute.
SpO2 improved to 98% on room air.
Skin color returned to normal, lips appear pink.
Assessment
Patient reports throbbing pain in legs and joints.
Pain score of 8 out of 10 on pain scale.
Diagnosis
Acute Pain related to restricted blood flow within small vessels due to sickled cells, leading to localized blood congestion, as evidenced by:
Patient verbalization of throbbing pain in legs and joints.
Goals/Expected Outcomes
Pain relief within 4 hours.
Enhance venous blood flow.
Improve overall blood circulation.
Intervention
Administer prescribed analgesics:
Initial dose of pethidine 50 mg.
Followed by tramadol 50 mg every 8 hours for 3 days as per physician’s order and documented protocol.
Continue intravenous fluid administration as previously prescribed.
Monitor pain levels hourly.
Rationale
Pain medications are used to provide comfort and reduce discomfort and agitation.
IV fluids help maintain adequate blood volume and flow.
Evaluation
Patient reports reduced pain after 4 hours, pain score now 2 out of 10.
Assessment
Reduced hemoglobin level of 5 g/dL based on lab results.
Swelling in lower limbs and joints.
Diagnosis
Altered Tissue Perfusion related to decreased oxygen-carrying capacity of blood cells as evidenced by:
Low hemoglobin levels (5 g/dL).
Swelling of lower limbs and joints.
Goals/Expected Outcomes
Restore normal tissue perfusion within 24 hours.
Achieve improved tissue perfusion.
Intervention
Administer blood transfusion:
Packed red blood cells at 5 mL/kg/hour as prescribed.
Continue monitoring fluid balance.
Apply warm compresses to affected areas.
Elevate affected limbs.
Rationale
Blood transfusion increases the level of hemoglobin in the blood.
Fluid balance monitoring is important to prevent overload.
Warm compresses promote blood vessel dilation and improve circulation to oxygen-deprived tissues.
Limb elevation helps reduce swelling and improve venous return.
Evaluation
Hemoglobin levels increased to 7 g/dL in post-transfusion lab report.
Swelling has decreased, and patient is able to move the limb more easily.
Assessment
Fever.
Hypermetabolic state.
Signs of dehydration: dry mucous membranes, poor skin turgor.
Diagnosis
Risk for Fluid Volume Deficit related to increased fluid requirements secondary to hypermetabolic state and fever.
Goals/Expected Outcomes
Maintain sufficient hydration.
Prevent fluid depletion.
Intervention
Regularly monitor vital signs and fluid status.
Encourage oral fluid intake.
Administer IV fluids as necessary.
Educate patient about the importance of adequate fluid intake.
Rationale
Frequent monitoring helps in early detection of fluid deficit.
Encouraging and providing fluids ensures adequate hydration and prevents complications.
Evaluation
Fluid balance is maintained, and signs of dehydration are no longer present.
Assessment
Presence of venous stasis.
Vaso-occlusion.
Decreased mobility.
Risk of skin breakdown.
Diagnosis
Risk for Impaired Skin Integrity related to compromised circulation due to venous stasis and vaso-occlusion, coupled with reduced mobility.
Goals/Expected Outcomes
Prevent skin breakdown from occurring.
Maintain intact skin integrity.
Intervention
Regularly assess skin for any signs of breakdown or pressure areas.
Reposition patient every 2 hours.
Provide diligent skin care:
Keep skin clean and dry.
Rationale
Regular skin assessment and repositioning are effective in preventing pressure ulcers.
Good skin hygiene promotes skin health and integrity.
Evaluation
Skin remains intact without any indications of breakdown.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

