Medical Nursing (III)
Subtopic:
Systemic Lupus Erythematosus
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease. In SLE, the body’s immune system malfunctions and attacks healthy tissues and organs. This misdirected immune response results in widespread inflammation and potential organ damage throughout the body. SLE can affect multiple organ systems.
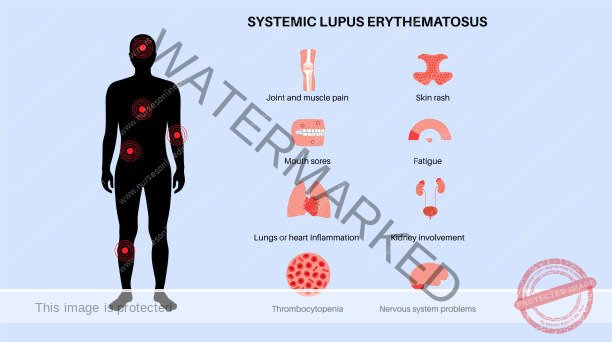
SLE can affect various parts of the body, including:
Joints
Skin
Brain
Lungs
Kidneys
Blood Vessels
The severity and specific symptoms of lupus are highly variable among individuals.
Causes of Systemic Lupus Erythematosus
The precise cause of SLE is currently unknown (idiopathic).
SLE development is considered to be multifactorial, involving a combination of:
Genetic Predisposition: Individuals may inherit genes that increase susceptibility.
Hormonal Factors: Hormones, particularly female hormones, are thought to play a role.
Environmental Triggers: Exposure to certain environmental factors may initiate SLE in susceptible individuals.
Potential environmental triggers:
Sunlight (UV radiation)
Infections
Certain Medications
Physical or Emotional Stress
The influence of female hormones may contribute to the higher prevalence of SLE in women, especially during their reproductive years.
Pathophysiology of Systemic Lupus Erythematosus
SLE pathogenesis is associated with disruptions in apoptosis, a normal process of programmed cell death for removing aged or damaged cells.
In SLE, dysregulation of apoptosis can trigger an autoimmune response, leading to the production of antinuclear antibodies (ANAs).
Normal Apoptosis: Damaged or old cells undergo apoptosis and are cleared from the body.
SLE Disruption:
SLE risk factors (e.g., UV light) can induce cell damage and apoptosis.
Dying cells form apoptotic bodies, exposing nuclear components (DNA, histones, proteins).
In genetically susceptible individuals, the immune system misidentifies these nuclear components as foreign (nuclear antigens).
Impaired clearance of apoptotic bodies can further contribute to the accumulation of nuclear antigens.
Antinuclear Antibody (ANA) Production:
B-cells produce ANAs against nuclear antigens.
ANAs bind to nuclear antigens, forming Antigen-Antibody Complexes.
Immune Complex Deposition and Tissue Damage:
Antigen-Antibody complexes circulate in the bloodstream and deposit in blood vessel walls and organs (kidneys, skin, joints, heart).
Deposition triggers local inflammation.
Complement System Activation: Inflammation activates the complement system, leading to cell lysis and further tissue damage.
In SLE, this process mistakenly targets healthy cells.
Type 3 Hypersensitivity Reaction: Tissue damage from deposited immune complexes is a Type 3 Hypersensitivity Reaction, characterized by immune complex deposition and inflammation.
Type 2 Hypersensitivity Reaction: If antibodies target blood cells (red/white blood cells) or phospholipids, it leads to cell destruction via phagocytosis. This is classified as a Type 2 Hypersensitivity Reaction, involving direct antibody-mediated cell destruction.
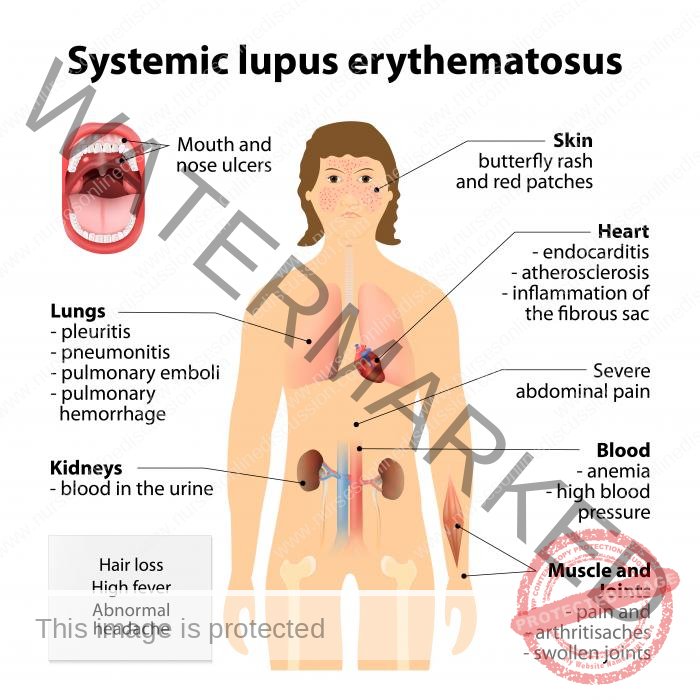
Clinical Features of Systemic Lupus Erythematosus
The progression of Systemic Lupus Erythematosus (SLE) is characterized by alternating periods of heightened disease activity, known as flares, and periods of symptom reduction, called remissions. The frequency and intensity of these flares and remissions are highly variable among individuals.
Symptoms can manifest with varying degrees of severity, ranging from mild to severe, and can appear gradually or abruptly. These symptoms may be transient or persistent. The specific symptoms experienced depend on the organs and systems affected by SLE. The clinical presentation of lupus is diverse and can affect many parts of the body.
Frequently Reported Symptoms:
Fever: Elevated body temperature indicating inflammation.
Fatigue: Persistent, overwhelming tiredness unrelieved by rest.
Dyspnea: Shortness of breath or feeling of insufficient air intake.
Chest Pain: Discomfort in the chest area, potentially linked to inflammation of heart or lung linings.
Dry Eyes: Insufficient tear production or rapid tear evaporation.
Butterfly Rash (Malar Rash): Distinctive reddish rash across the cheeks and bridge of the nose.
Headaches: Pain in the head, varying in intensity and frequency.
Cognitive Issues: Confusion and memory problems, indicating difficulties with clear thinking and recall.
Raynaud’s Phenomenon: Fingers and toes turning white or blue in response to cold or stress due to reduced blood flow.
Hair Loss (Alopecia): Diffuse thinning or fragile hair with visible breakage, not attributable to other causes.
Anemia: Lower than normal red blood cell count, leading to fatigue.
Joint Issues: Joint swelling and pain, indicative of inflammation.
Photosensitivity: Unusual sensitivity to sunlight leading to sunburn or skin rashes.
Diagnosis and Investigations
Diagnosing Systemic Lupus Erythematosus (SLE) can be challenging as no single test is definitive. Accurate diagnosis relies on a combination of assessments.
Diagnostic methods include:
Blood and Urine Tests: To evaluate various blood components and kidney function.
Complete Blood Count (CBC): Assesses blood cell levels.
Urinalysis: Examines urine for abnormalities.
Erythrocyte Sedimentation Rate (ESR) & C-Reactive Protein (CRP): Measure inflammation levels in the body.
Antinuclear Antibody (ANA) Test: Detects antibodies commonly present in lupus.
Imaging Tests: To visualize internal organs.
Chest X-ray: Visualizes lungs and heart structures.
Echocardiogram: Assesses heart structure and function.
Biopsy: Examination of a small tissue sample to confirm organ involvement, if needed.
Established SLE Criteria: Use of standardized diagnostic criteria, such as those from the American College of Rheumatology or SLICC criteria, to aid in diagnosis.
Systemic Lupus International Collaboration Criteria (SLICC) for the diagnosis of SLE
These SLICC criteria, an update to the American College of Rheumatology criteria, provide a standardized framework for SLE diagnosis. A diagnosis of SLE is considered if specific clinical and immunological criteria are met.
Diagnostic Criteria Include:
Malar Rash: Rash across the cheeks, typically sparing the folds between the nose and mouth.
Discoid Rash: Raised, scaly, circular skin patches that may cause scarring.
Photosensitivity: Skin reaction resulting from heightened sensitivity to sunlight.
Oral Ulcers: Sores or breaks in the mucous membrane of the mouth or throat.
Arthritis: Joint inflammation affecting multiple joints.
Serositis: Inflammation of membranes around the lungs (pleuritis) or heart (pericarditis).
Renal Disorder: Kidney abnormalities indicated by significant protein in urine (greater than 0.5 grams per day) or cellular casts in urine.
Neurologic Disorder: Neurological issues such as seizures or psychosis.
Antinuclear Antibody (ANA): Positive ANA antibody test result.
Immunologic Disorder: Abnormal immune test results, including positive anti-Smith, anti-dsDNA, or false positive syphilis serology.
Hematologic Disorder: Blood abnormalities such as low red blood cell count or low white blood cell count.
Management of Systemic Lupus Erythematosus
The objectives of Systemic Lupus Erythematosus (SLE) management are comprehensive and focused on improving long-term patient health and well-being.
Management Aims:
Prolonged Survival: To manage the disease and prevent life-threatening complications, aiming for long-term survival.
Minimal Disease Activity: To achieve the lowest possible level of disease activity, minimizing flares.
Organ Protection: To prevent damage to vital organs from the effects of lupus.
Drug Toxicity Minimization: To use medications cautiously to reduce potential adverse effects.
Enhanced Quality of Life: To help patients maintain a fulfilling and active lifestyle.
Nurse’s Role in the management of Systemic Lupus Erythematosus
Nurses are vital in the care of individuals with SLE, providing essential education, monitoring, and support. The acronym L.U.P.U.S. can be a helpful memory aid for key nursing care aspects.
L.U.P.U.S. – Nursing Care in SLE
L – Labs: Essential for diagnosis and monitoring disease flares.
Antibody Labs: Specific tests to detect and monitor autoimmune activity.
Positive ANA (Antinuclear Antibodies): Indicates antibodies attacking the body’s own cell nuclei.
Anti-dsDNA (Anti-double stranded DNA Antibody): Antibody specific to DNA, often associated with lupus severity.
Anti-Sm Antibody (Anti-Smith Antibody): Highly specific antibody for lupus diagnosis.
Inflammation Markers:
Elevated ESR (Erythrocyte Sedimentation Rate) & CRP (C-Reactive Protein): Indicators of systemic inflammation.
Routine Blood Tests:
CBC, Metabolic Panel, etc.: Assess overall health and organ function.
U – Use Medications: Medications are crucial for symptom control, flare reduction, and organ damage prevention.
Steroids (Corticosteroids): Prednisone, Prednisolone, etc.
Action: Potent anti-inflammatory drugs for rapid inflammation control.
Use: Effective for quick symptom relief but have potential long-term side effects. Often used for severe flares or when other medications are insufficient.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Ibuprofen, Naproxen, etc.
Action: Reduce pain and inflammation.
Use: Helpful for managing fever and joint pain, milder symptoms.
Antimalarials: Hydroxychloroquine (common SLE medication).
Action: Regulates the immune system, reducing antibody attacks.
Use: Long-term disease control, preventing flares.
Immunosuppressants: Azathioprine, Mycophenolate Mofetil, etc.
Action: Suppress the immune system.
Use: For severe lupus cases, “steroid-sparing” effect (reducing steroid dosage). Requires infection risk monitoring. Patient education on infection prevention is vital as these medications, including steroids, can mask infection signs (e.g., fever).
Vaccines: Up-to-date vaccinations recommended, but avoid live vaccines (shingles, MMR, intranasal flu, smallpox, rotavirus) due to immunosuppression.
Biologics: Belimumab.
Action: Targets specific immune system components, reducing B-cell activity.
Result: Decreases antibody attacks and inflammation.
Vaccines: No LIVE vaccines should be administered.
P – Pregnancy: Education for women of childbearing age is essential.
Pre-conception Planning: Women planning pregnancy should ensure lupus is well-controlled for at least 6 months prior to conception. Pregnancy and postpartum periods can increase flare risk.
U – Understanding Flares: Recognizing and managing flares is key for patient self-management.
Flare Triggers: Sunlight, stress, infections, medication non-adherence or need for adjustment.
Flare Prevention: “LESS” Flares Strategy:
L – Lower Stress: Avoid overwork, manage emotional stress, prevent illness, utilize stress reduction techniques.
E – Exercise: Regular exercise benefits joints and weight management.
S – Sleep: Adequate sleep (more than 8 hours) to prevent exhaustion.
S – Sun Protection: Sunscreen, wide-brimmed hats – sunlight can trigger flares.
S – Signs of a Flare: Educate patients to monitor symptoms and keep a diary to detect flares early.
Flare Symptoms: Fatigue increase, low-grade fever, achy joints, new or worsening rash, edema in legs and hands.
Medical Management
Treatment for Systemic Lupus Erythematosus (SLE) is individualized and depends on disease severity and specific patient symptoms.
Treatment Intensity Categories:
Mild Cases: Disease pattern with one or two organ systems involved.
Moderate Cases: More than two organ systems involved during flares with low-grade involvement, or one to two organs with more extensive involvement.
Severe Cases: Life-threatening complications and multiple (more than 2) organ system involvement.
Medications Commonly Used:
Hydroxychloroquine: 200-400 mg daily, single or divided doses. Foundational medication for most SLE patients regardless of severity.
Combination Therapy (Common for Active Disease):
Hydroxychloroquine (200-400 mg daily) AND Methylprednisolone (IV 0.5-1g/day for 3 days in acute cases, or 1-2 mg/kg/day in stable patients).
OR Hydroxychloroquine (200-400 mg daily) AND Prednisone (oral 40-60 mg/day).
Fever Management:
Celecoxib: 100-200 mg twice daily. (NSAID)
OR Acetaminophen: 1000 mg every 6 hours, max 3000 mg daily.
Raynaud’s Phenomenon Treatment:
Calcium Channel Blocker (Nifedipine): 10-30 mg three times daily.
Chronic Pain Management:
Moderate Pain: Mild prescription opiates.
Co-codamol (Acetaminophen + Codeine): Acetaminophen (300-1000mg)/codeine (15-60mg) every 4 hours PRN (max: acetaminophen 4000mg/codeine 360mg per 24 hours).
Moderate to Severe Chronic Pain: Stronger opioids.
Hydrocodone: Single doses >40mg or >60mg with total daily dose ≥80mg.
Cutaneous Lupus Erythematosus (Skin Lupus):
High Potency Topical Steroids: Twice daily for CLE lesions.
Hydrocortisone 1% or 2.5%: For facial involvement.
Lupus Nephritis Treatment (Kidney Lupus):
Aggressive Antihypertensive Therapy: Blood pressure goal of 130/85 mmHg.
Antiproteinuric Therapy (for Proteinuria): Renin-Angiotensin System blockade.
ACE Inhibitors (e.g., Captopril): 25 mg three times daily.
ARBs (e.g., Losartan): Initial 50 mg once daily, can increase to 100mg based on BP response.
Other Considerations:
Vitamin D & Calcium Supplements: To prevent osteoporosis in corticosteroid users.
Antihypertensives & Statins: Recommended for corticosteroid users to manage blood pressure and cholesterol.
Nursing Interventions and Rationales
Nurses implement various interventions tailored to the specific needs of SLE patients, based on their symptoms and treatment plan.
Nursing Interventions & Rationales:
Nutrition and Hydration: Encourage adequate intake.
Rationale: Promotes healthy skin and wound healing.
Skin Care: Instruct client on proper skin care.
Cleaning & Moisturizing: Clean, dry, moisturize intact skin; use warm (not hot) water, especially over bony areas; unscented lotion; mild shampoo.
Rationale: Gentle care prevents irritation and breakdown. Scented lotions may contain drying alcohol. Prescribed solutions can reduce scalp dryness.
Avoid Harsh Chemicals: Instruct client to avoid harsh chemicals, wear protective gloves as needed, avoid hair dyes, permanents, curl relaxers.
Rationale: Chemicals aggravate skin conditions.
Pressure Relief: Recommend prophylactic pressure-relieving devices (e.g., special mattress, elbow pads).
Rationale: Prevents skin breakdown.
For Skin Rash:
Sun Protection: Wear protective eyewear, wide-brimmed hat, carry umbrella, avoid UV rays.
Rationale: Sun exacerbates rash and can trigger flares. Special lotions and glasses may be needed.
Special Makeup: Inform client about special makeup to cover rashes, especially facial rashes.
Rationale: Cosmetics improve body image by concealing rashes and pigmented areas, aiding adjustment to body image changes.
Hydroxychloroquine Education: Introduce or reinforce information about hydroxychloroquine.
Rationale: Educate about a key medication. It’s a slow-acting anti-inflammatory that may take 8-12 weeks to be effective. Retinal toxicity is a potential side effect requiring ophthalmologist follow-up every 6 months. Topical cortisone may also be used.
For Oral Ulcers:
Dietary Modification: Instruct client to avoid spicy or citrusy foods.
Rationale: These foods irritate mucous membrane ulcers.
Mouth Rinse: Instruct client to rinse mouth with half-strength hydrogen peroxide three times daily.
Rationale: Hydrogen peroxide keeps ulcers clean.
Ulcerated Skin Care: Instruct client to keep ulcerated skin clean and dry, apply dressings as needed.
Rationale: Prevents infection and promotes healing.
Topical Ointments: Instruct client to apply topical ointments as prescribed.
Vitamins: Vitamins A and E may be beneficial for skin health.
For Hair Loss:
Scalp Hair Loss Information: Instruct client that scalp hair loss occurs during disease exacerbation.
Rationale: Scalp hair loss can be an early sign of flare. It may not be permanent and can regrow as disease activity subsides.
Medication-Related Hair Loss: Instruct client that hair loss can be caused by high-dose corticosteroids (prednisone) and immunosuppressants.
Rationale: Hair may regrow as medication doses are reduced.
Coping Strategies: Encourage client to explore ways to conceal hair loss (e.g., scarves, hats, wigs).
Rationale: Hair loss can impact lifestyle and self-image.
Complications
Skin Scarring: Permanent marks or changes in skin appearance resulting from lupus-related skin conditions.
Joint Deformities: Lasting alterations in joint shape or alignment due to persistent inflammation and damage within the joints.
Renal Failure: Loss of kidney function, potentially necessitating dialysis or kidney transplantation due to severe lupus-induced kidney damage.
Cerebrovascular Accident (Stroke): Interruption of blood supply to the brain, possibly occurring from blood clots or inflammation of brain blood vessels associated with lupus.
Myocardial Infarction (Heart Attack): Damage to the heart muscle caused by reduced blood flow; risk is elevated in lupus patients due to inflammation and blood vessel problems.
Pregnancy-Related Issues: Increased likelihood of complications during pregnancy, such as pre-eclampsia, early delivery, or pregnancy loss, because of lupus effects on the maternal body.
Avascular Necrosis of the Hip: Bone tissue death in the hip joint due to insufficient blood supply; a possible complication of both lupus and its treatments.
Cataracts: Clouding of the eye’s lens, which can develop as a side effect of some lupus medications, especially corticosteroids.
Bone Fractures: Increased vulnerability to bone breaks, often linked to osteoporosis, which can be a consequence of lupus treatments like corticosteroids.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

