Surgical Nursing (III)
Subtopic:
Tonsillitis
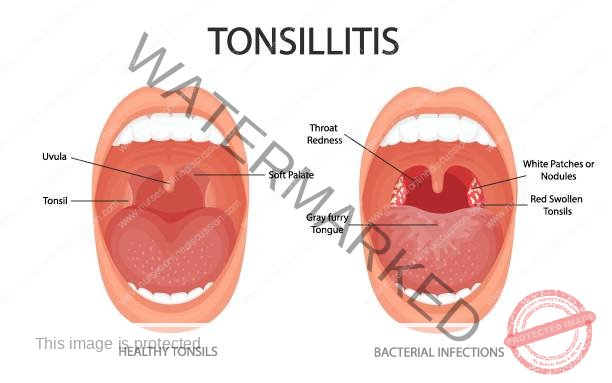
Tonsillitis refers to the inflammation of the tonsils. The tonsils are two oval-shaped masses of tissue situated at the rear of the throat, with one tonsil on each side. Tonsillitis is infectious and can be easily spread, particularly before noticeable symptoms appear. The tonsils play a protective role by capturing pathogens that could otherwise enter the respiratory system and cause bodily infection. They are also involved in the production of antibodies, which help fight off infections. Tonsillitis can present as either a sudden, short-term condition (acute) or a long-lasting or recurring problem (chronic).
Tonsils
Tonsils are composed of a collection of lymphatic tissue, positioned on either side of the oropharynx, which is the middle part of the throat.
Their primary function is to act as a component of the body’s defense system.
Specifically, tonsils contribute to the body’s ability to resist infection by trapping invading pathogens.
CAUSES OF TONSILLITIS
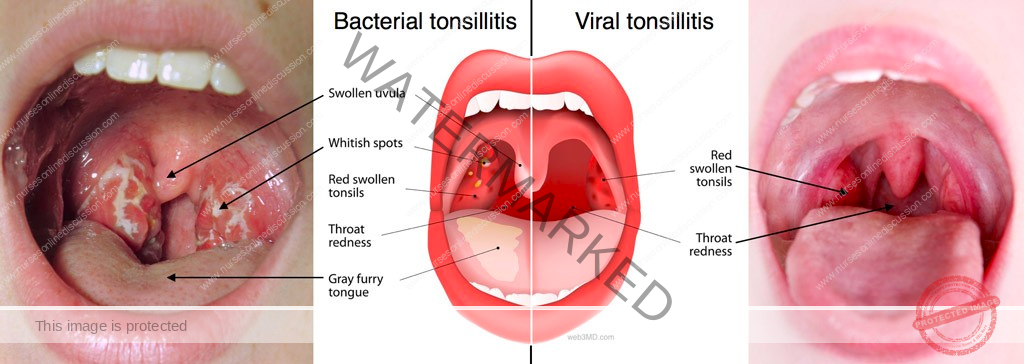
Tonsillitis can arise from viral infections, often associated with the common cold. Indeed, viruses are the most frequent cause of tonsillitis, resulting in what is known as viral tonsillitis. The same viruses responsible for the common cold are often the culprits behind tonsillitis; however, various other viruses can also cause this condition. These include rhinoviruses, the Epstein-Barr virus (EBV), the hepatitis A virus, and the human immunodeficiency virus (HIV).
Given that the Epstein-Barr virus is capable of causing both infectious mononucleosis (mono) and tonsillitis, individuals with mono may subsequently develop tonsillitis as a secondary bacterial infection.
Another significant cause of tonsillitis is bacterial infection. The bacterium most commonly associated with tonsillitis is Streptococcus pyogenes (which causes strep throat); however, other bacterial species can also be responsible.
Tonsillitis is particularly prevalent in children within the age range of 5 to 15 years.
The tonsils, being composed of lymphatic tissues, are particularly susceptible to acute infections due to their role in the immune system and their location in the throat.
TYPES OF TONSILLITIS
Tonsillitis is broadly categorized into two main forms:
Acute Tonsillitis: This refers to a sudden onset of tonsil inflammation.
Chronic Tonsillitis: This indicates a long-term or repeatedly occurring inflammation of the tonsils.
ACUTE TONSILLITIS (Recurring): This condition involves a rapid and widespread inflammation affecting the tonsils. Frequently, it also includes inflammation of the nearby palatal arches and the pharynx, resulting in a sore throat. It is more prevalent in children compared to adults. The typical cause is bacteria, specifically Group A Beta-hemolytic Streptococcus, though viral infections can also be responsible.
CHRONIC TONSILLITIS: This form is defined by a continuous, ongoing inflammation within the tonsils. Frequent recurrence of acute episodes, such as 5 to 6 times annually, may suggest a lack of sufficient immune response, leading to the classification as chronic tonsillitis.
CLINICAL FEATURES OF TONSILLITIS
Signs and symptoms of tonsillitis may present as:
Abrupt symptom onset.
Throat pain, often described as intense.
Fever and chills.
Snoring due to airway obstruction from enlarged tonsils.
Headache and vomiting may occur.
Painful and difficult swallowing (dysphagia).
Tonsils appear enlarged, often with pus or whitish/yellowish spots (exudates) visible.
Swollen and painful lymph nodes in the neck region.
Increased saliva production.
Foul breath odor (halitosis).
Neck stiffness and unexplained weight loss, especially in chronic cases.
Cough and nasal congestion can sometimes be present, more often in viral cases.
DIAGNOSIS AND INVESTIGATIONS
The diagnostic process for tonsillitis typically includes:
Patient history collection.
Physical throat examination, including neck palpation to assess for enlarged lymph nodes.
Throat swab to collect pus from the posterior pharynx for culture and sensitivity (C/S) testing, to identify the causative microorganism.
Complete blood count (CBC) blood test to aid in differentiating between bacterial and viral causes, guiding appropriate treatment strategies.
Management of tonsillitis can be Medical or Surgical, depending on the condition’s severity and how often it occurs.
AIMS of Management
Treatment goals for tonsillitis are focused on:
Restricting or preventing infection spread.
Relieving signs and symptoms such as pain and elevated temperature.
Treating the underlying cause of the infection itself.
Preventing potential complications from arising.
Medical Management
Patient admission to a medical isolation unit, implementing strict isolation protocols and barrier nursing techniques to limit infection transmission.
Patient and family reassurance.
Vital signs monitoring (temperature, heart rate, respiratory rate, and blood pressure) and noting specific indicators like tonsil size.
Fever reduction using tepid sponging methods (applying lukewarm water to the skin surface).
Medication administration:
Antibiotics, particularly penicillin (e.g., Penicillin V 500mg every 6 hours for 10 days), are used for confirmed bacterial infections. Antibiotics are ineffective against viral tonsillitis.
Analgesics, such as aspirin, to alleviate pain and reduce fever.
Normal saline gargles (saltwater rinse) instructions for the patient.
Encouraging ample oral fluid intake (minimum 4-5 liters per day) and promoting oral hygiene through frequent mouth rinsing.
Routine daily nursing care as needed for any patient.
Neck support during swallowing if the patient is a child.
Provision of a highly nutritious diet that is soft in texture and easy to swallow, gradually progressing diet consistency as tolerated.
Frequent oral care to maintain cleanliness of the mouth.
Special Observations
Monitor for facial swelling (edema), especially in the morning, which could suggest kidney inflammation (nephritis).
Observe for joint pain, which might indicate rheumatic fever development.
Monitor fluid intake and urine output for decreased urine production and presence of protein in urine (albuminuria).
Continuous monitoring for other possible complications.
SURGICAL MANAGEMENT (for chronic tonsillitis only)
Surgical intervention, specifically tonsillectomy, is considered for managing chronic tonsillitis. However, simply having enlarged tonsils without frequent infections is generally not a reason for removal, as tonsil size in children is naturally larger and tends to decrease with age.
Pre-operative management is similar to that for any surgical procedure.
TONSILLECTOMY
Tonsillectomy is the surgical procedure involving the removal of the tonsils. It is indicated for severe, chronic tonsillitis, when frequent recurrences disrupt schooling or daily life, and when there is concern about disease-related complications.
Surgery is performed under general anesthesia, where the tonsils are carefully removed from the underlying pharyngeal tissue by dissection.
Pre-operative preparation includes standard procedures for general anesthesia, with special attention to oral hygiene and prophylactic intravenous antibiotic administration, such as ceftriaxone.
POST-OPERATIVE CARE
Upon patient transfer from the operating room, a post-operative recovery bed is prepared with all necessary equipment.
Post-operative positioning involves placing the patient on their side in a recovery position with a slightly lowered head to prevent aspiration of blood or tonsil tissue fragments. This position is maintained until full alertness is achieved.
Regular post-operative observations of temperature, pulse, respiration, and blood pressure are performed.
Skin color monitoring and observation for bleeding signs, such as frequent swallowing. Significant bleeding may require a return to the operating room for surgical ligation of bleeding points.
Encourage spitting out secretions rather than swallowing.
Antibiotic administration to prevent or manage infections, such as intravenous ceftriaxone post-operatively, or oral penicillin V if the original tonsillitis was acute.
Fluid and soft food introduction is encouraged the day after surgery.
Oral care, ideally with warm saline gargles, is recommended.
Discharge occurs once patient condition improves, along with appropriate discharge instructions.
Complications of Tonsillitis
Untreated or severe tonsillitis can lead to various complications, including:
Rheumatic fever: an inflammatory condition affecting the heart, joints, brain, and skin.
Nephritis: kidney inflammation.
Asthma exacerbation: worsening of respiratory symptoms.
Peritonsillar abscess (quinsy): a pus collection behind the tonsil.
Peritonsillar cellulitis: bacterial infection of tissues surrounding the tonsils.
Otitis media: middle ear infection.
Complications following Tonsillectomy
Hemorrhage (bleeding): the most common immediate post-tonsillectomy complication.
Secondary bacterial infections at the surgical site.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

