Neurological Disorders in Children
Subtopic:
Congenital toxoplasmosis
Congenital Toxoplasmosis
This condition impacts unborn babies or newborns. It arises when a fetus contracts Toxoplasma gondii, a parasitic microbe, from the mother during gestation.
This infection can tragically result in pregnancy loss, either as a miscarriage or stillbirth.
Even in live births, congenital toxoplasmosis may induce substantial and persistent issues impacting sight, hearing, movement abilities, thinking skills, and other developmental areas as the child matures.
Although Toxoplasma gondii infection frequently presents without symptoms in healthy people, it poses a significant risk to individuals with compromised immunity and pregnant individuals because of the possible effects on the developing fetus.
Crucially, an infant might seem healthy at delivery, yet the infection’s harm could become evident later in childhood or even adulthood.
The seriousness of congenital toxoplasmosis in the infant is mainly dictated by the timing of infection transmission during pregnancy. Earlier transmission is often associated with more severe consequences.
Causes of Toxoplasmosis
Toxoplasmosis is specifically triggered by the Toxoplasma gondii parasite.
This parasite’s life cycle includes wild and domesticated cats. Infected felines excrete a resistant parasitic form called oocysts in their waste, making cat feces a major source of environmental contamination.
Mode of Transmission
Toxoplasmosis can be contracted by humans via different pathways:
Vertical Transmission:
Congenital Transmission: This happens when a pregnant woman contracts toxoplasmosis, and the parasite traverses the placenta to infect her fetus. The mother may show no symptoms, but the infection can induce severe issues in the developing baby, notably impacting the brain, nerves, and vision.
Horizontal Transmission
Foodborne: A frequent route of toxoplasmosis acquisition is consuming undercooked meat harboring dormant, infectious stages (tissue cysts) of the T. gondii parasite. Cross-contamination may also occur when handling raw meat and then touching ready-to-eat foods, or via contaminated kitchen tools and cutting surfaces. Furthermore, ingesting raw, unpasteurized goat milk can also result in infection.
Zoonotic Transmission: This pertains to the spread from animals to humans. Domestic cats are key in this transmission pathway. Infected cats release oocysts in their feces. These tiny oocysts can be inadvertently ingested by people, for instance, by inadequate hand washing after cleaning a cat litter box, consuming oocyst-contaminated water, or through contact with contaminated soil during gardening without gloves.
Rare Transmission Routes: Though infrequent, toxoplasmosis can be transmitted via organ donation and transplantation if the donor was infected. Extremely rarely, it can also be transmitted through blood transfusions.

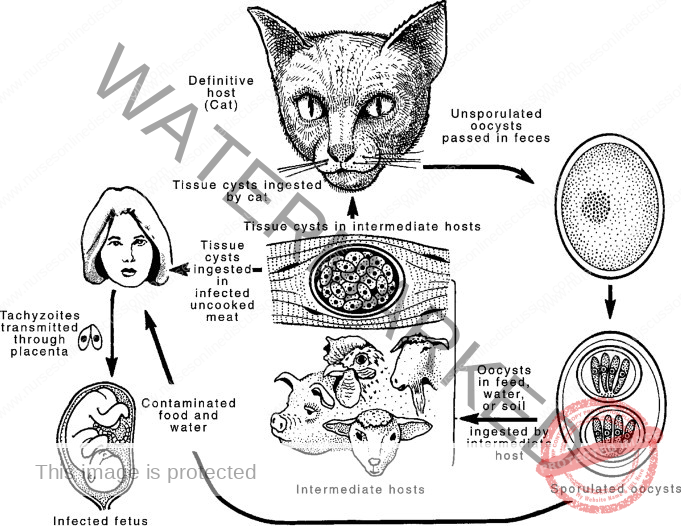
LIFE CYCLE OF TOXOPLASMA GONDII.
Toxoplasma gondii is a common, adaptable single-celled parasite that must live inside the cells of other organisms to survive and reproduce (obligate intracellular protozoa). It can infect a wide range of animals, including humans.
In cats, T. gondii has two main phases: an intestinal cycle and a cycle that occurs outside the intestines. However, in other animals (intermediate hosts), including humans, only the extra-intestinal cycle takes place.
The parasite exists in three main infectious forms: Bradyzoites, Tachyzoites, and Sporozoites.
Bradyzoites: These are slow-growing forms of the parasite that are contained within tissue cysts. These cysts typically establish themselves in skeletal and heart muscles, the eyes, and the brain, where they can persist for many months or even years within the host’s cells. When these cysts are consumed (ingested), the stomach’s digestive enzymes break down the cyst wall, releasing the viable Bradyzoites.
Tachyzoites: These are rapidly multiplying forms of the parasite that are found in the tissues during the acute (early) stages of infection. They invade neural (nerve) and muscle tissues and eventually develop into tissue cysts. Tachyzoites are responsible for the tissue damage seen in active infections. They multiply rapidly until either a cyst is formed to contain them, or the host cell they are inside is destroyed. After a host cell dies, the released Tachyzoites can invade other cells and begin multiplying rapidly again.
Sporozoites: These forms result from the parasite’s sexual reproduction, which occurs within the intestines of cats (the definitive host). When a cat sheds the parasite through its feces, these oocysts are initially not infectious. They must undergo a process called sporulation (which takes 2-3 days) to become infectious Sporozoites. This means that the risk of transmission from cat feces is lower if the litter box is cleaned daily, before the oocysts have fully developed into their infectious form.
Pathogenesis for vertical transmission
A new (acute) infection with Tachyzoites circulating in the mother’s bloodstream during pregnancy increases the likelihood of the parasite crossing the placenta and infecting the fetus (transplacental infection).
The Tachyzoites can establish themselves in the placenta and then breach the placental barrier to reach the developing fetus.
The likelihood of the parasite being transmitted to the fetus is related to the stage of pregnancy (gestational age). While the transmission rate is lower in the first trimester (early pregnancy), it is highest in the third trimester (later stages of pregnancy). However, paradoxically, if the infection occurs earlier in the pregnancy, the disease tends to be more severe for the developing baby.
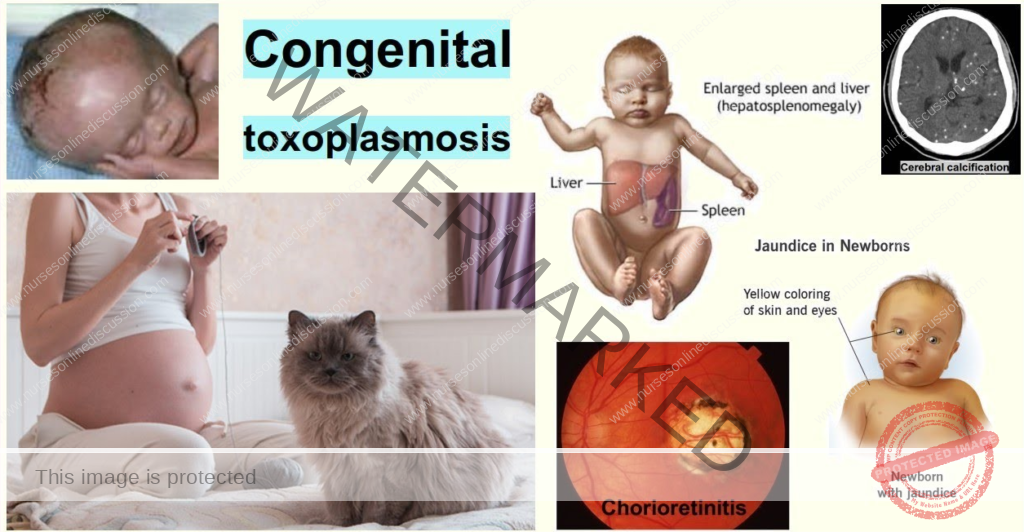
Clinical Presentation
The signs and symptoms of congenital toxoplasmosis exhibit a wide range of severity. Common manifestations include:
Preterm birth: Birth occurring earlier than the expected due date, estimated in approximately half of affected infants.
Low birth weight: Infants weighing less than expected for their gestational age at birth.
Ocular Impairment: Visual disturbances such as blurred vision, heightened sensitivity to light (photophobia), and excessive tearing (epiphora).
Intrauterine growth restriction (IUGR): Reduced fetal growth rate within the uterus compared to normal expectations.
Mild Fever: A slightly elevated body temperature.
Vomiting episodes: Frequent episodes of throwing up.
Jaundice: Yellowish discoloration of the skin and sclera (whites of the eyes) due to liver involvement.
Diarrhea: Loose and frequent bowel movements.
Anemia: Reduced levels of red blood cells in the blood.
Auditory impairment: Hearing loss resulting from damage to the auditory system.
Delayed motor and cognitive development: Slower achievement of developmental milestones and difficulties with movement skills.
Hydrocephalus: Accumulation of cerebrospinal fluid in the brain’s ventricles, leading to increased head circumference.
Feeding difficulties: Problems with sucking or swallowing.
Lymphadenopathy: Swollen lymph nodes, often painless, firm, and localized.
Hepatosplenomegaly: Enlargement of the liver and spleen.
Macrocephaly: Abnormally large head size.
Microcephaly: Abnormally small head size.
Skin Rash: A typical rash characterized as flat with small raised areas (maculopapular), often sparing the palms and soles.
Bulging fontanelle: Protrusion or swelling of the soft spot on an infant’s head.
Abnormal Muscle Tone: Muscles that are either excessively stiff or overly relaxed.
Seizures: Episodes of uncontrolled electrical activity in the brain, causing convulsions.
Intracranial Calcifications: Calcium deposits within the brain tissue, indicating areas of parasitic damage.
Diagnosis of Toxoplasmosis
Diagnosis of congenital toxoplasmosis typically involves a combination of:
Patient History: Gathering details about the mother’s pregnancy, potential exposure risks, and the infant’s symptoms.
Physical Exam: A thorough physical assessment of the newborn.
Laboratory and Imaging Studies: Various tests to confirm the diagnosis.
Serology: Blood tests measuring antibody levels. Elevated Immunoglobulin G (IgG) suggests past infection. Immunoglobulin M (IgM) testing helps determine recent infection, crucial for assessing fetal risk during pregnancy.
Culture: Attempting to grow the parasite in a lab from tissue samples like cerebrospinal fluid. Less common due to sampling difficulty.
Amniocentesis: Testing amniotic fluid for the parasite’s DNA in pregnant women.
Brain Biopsy: Rarely performed in non-responsive cases to detect toxoplasmosis cysts.
Liver Function Tests (LFTs): Blood tests assessing liver enzymes (ALT, AST) for liver involvement.
Complete Blood Count (CBC): May reveal eosinophilia (elevated eosinophils, a type of white blood cell).
Renal Function Tests (RFTs): Blood tests assessing urea and creatinine levels for kidney involvement.
Electrolyte Levels: Blood tests to check for imbalances in electrolytes like potassium, calcium, and sodium.
Imaging Studies: To evaluate disease extent:
Ultrasound: Used during pregnancy to visualize the fetal brain for hydrocephalus. May also detect hepatosplenomegaly or liver calcifications in fetuses around 20-24 weeks gestation.
Magnetic Resonance Imaging (MRI): Detailed brain images for suspected nervous system involvement.
Computed Tomography (CT) Scan: Brain scan to identify intracranial calcifications, ventriculomegaly (enlarged ventricles), and hydrocephalus.
Treatment and Management
Toxoplasmosis treatment strategies are guided by the patient’s immune status and infection severity.
Outpatient Management: Typically suitable for immunocompetent patients or those without significant organ damage.
Activity Restriction: May be advised depending on illness severity and affected organ systems.
Patient Education: Essential, especially for pregnant women, focusing on prevention and fetal risks.
Regular Follow-up: Typically bi-weekly until stabilization, then monthly during therapy.
Routine Blood Monitoring: Weekly CBC for the first month, then bi-weekly; monthly LFTs and RFTs.
Medications:
Pyrimethamine: Antimalarial drug, inhibits folic acid absorption in the parasite.
Sulfadiazine: Antibacterial, often combined with pyrimethamine for effective toxoplasmosis treatment, targeting the tachyzoite stage. Renal excretion requires dosage adjustment in kidney impairment. Avoid in G6PD deficiency due to hemolysis risk; clindamycin is an alternative.
Sulfadiazine Dosage: 1-1.5 grams four times daily (QID) for 3-4 weeks, or 100 mg/kg/day divided twice daily (2DD).
Pyrimethamine: High doses can cause hemolytic anemia, necessitating close monitoring.
Pyrimethamine Dosage: 50-75 mg once daily orally (OD PO) for 2-3 weeks, then reduced to 25-37.5 mg OD PO for 4-5 weeks.
Corticosteroids: Prednisolone (1 mg/kg/day) used when cerebrospinal fluid protein is elevated or vision is threatened by chorioretinitis, continued until resolution.
Trimethoprim/Sulfamethoxazole: Antibiotic combination, 40 mg/kg/day divided twice daily (2DD).
Dapsone (with Pyrimethamine): 100 mg/kg/day orally for 1-3 weeks.
Clindamycin (with Pyrimethamine): For sulfadiazine sensitivity, 10-12 mg/kg twice daily orally for 4 weeks.
Folic Acid: Vitamin supplementation to mitigate bone marrow suppression from pyrimethamine.
Folic Acid Dosage: 10 mg three times weekly.
Prevention
Preventing toxoplasmosis is critical, especially for pregnant women and immunocompromised individuals. Key measures include:
Avoidance of Undercooked Foods: Refrain from consuming raw or undercooked meat, unpasteurized milk, and raw eggs.
Hygiene After Raw Food Handling: Thoroughly wash hands after handling raw meat, gardening, or soil contact.
Cat Feces Precautions: Avoid contact with cat feces.
Litter Box Disinfection: Disinfect cat litter boxes with boiling water for at least 5 minutes.
Safe Cooking Temperatures: Cook food to recommended safe internal temperatures.
Fruit and Vegetable Washing: Wash and peel all fruits and vegetables before eating.
Frequent Handwashing: Wash hands often, especially after food handling, and clean meat/produce cutting boards.
Gardening Gloves: Wear gloves when gardening, or consider avoiding it, to prevent soil contact.
Litter Box Avoidance During Pregnancy: If possible, avoid cleaning cat litter boxes during pregnancy.
Complications
Congenital toxoplasmosis can lead to various complications:
Intrauterine Growth Restriction (IUGR): Reduced fetal growth within the uterus.
Chorioretinitis: Inflammation of the retina and choroid, causing blurred vision, photophobia, and epiphora.
Cerebral Calcifications: Calcium deposits in brain tissue.
Toxoplasmic Encephalitis: Brain inflammation due to toxoplasmosis.
Intellectual Disability: Impaired cognitive function.
Seizures: Recurrent, uncontrolled brain electrical disturbances.
Nursing Diagnoses for Toxoplasmosis
Common nursing diagnoses for toxoplasmosis patients include:
Hyperthermia: Related to parasitic infection secondary to toxoplasmosis, as evidenced by temperature of 38.5°C, rapid shallow breathing, flushed skin, diaphoresis, and weak pulse.
Knowledge Deficit: Related to new diagnosis of toxoplasmosis, as verbalized by the patient expressing a desire for more information about their condition, cause, and treatment.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

