Conditions of the eye
Subtopic:
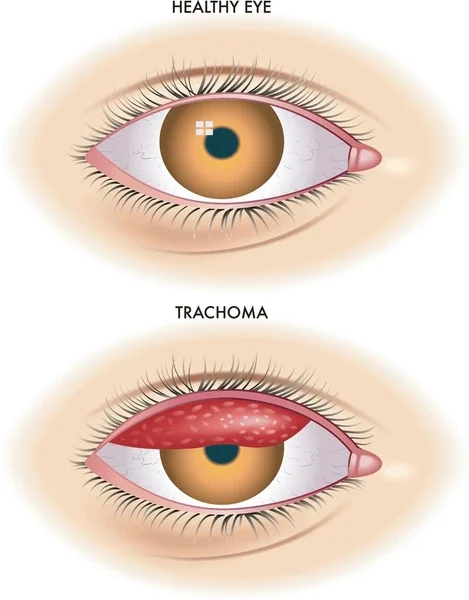
Trachoma
Trachoma is a contagious infection affecting the conjunctiva (the membrane lining the inner eyelids and covering the white part of the eye) and the cornea (the clear front surface of the eye). It is characterized by the formation of granulation (the development of small, grain-like tissue) and scarring.
Trachoma is a communicable bacterial infection that impacts the conjunctival lining, the cornea, and the eyelids.
The word “Trachoma” originates from a Greek term signifying “Roughness”.
Etiology
Trachoma is caused by the bacterium Chlamydia trachomatis. This condition is largely preventable and treatable. It stands as the primary infectious cause of blindness globally and is transmitted with considerable ease.
Predisposing Factors to Trachoma
Poor sanitation: Insufficient access to or use of facilities like latrines and proper waste disposal methods (e.g., rubbish pits).
Unclean or limited water supply: Lack of access to clean water sources can hinder hygiene practices.
Dry and dusty environment: Airborne particles can irritate the eyes and facilitate the spread of bacteria.
Overcrowding with unhygienic conditions: Close living quarters with poor sanitation increase the likelihood of transmission.
Reduced personal and community hygiene: Inadequate hygiene practices allow the bacteria to circulate and cause repeated infections.
Risk Factors of Trachoma
Dirty face: Lack of facial cleanliness allows bacteria to accumulate around the eyes.
Improper hand hygiene: Contaminated hands are a major vehicle for transmitting the bacteria.
Lack of awareness about hygiene: Limited understanding of personal and environmental hygiene practices increases risk.
Substandard housing: Inadequate or non-functional housing may lack proper sanitation.
Crowded living conditions: Sharing beds and close proximity increases the chance of transmission.
Poor water supply: Limited access to water makes maintaining hygiene difficult.
Swimming in contaminated water: Water sources can harbor the bacteria.
Poor nutrition: Malnutrition can weaken the immune system, making individuals more susceptible to infection.
Age: Children are particularly vulnerable due to close contact and hygiene habits.
Occupation: Certain occupations may involve greater exposure to risk factors.
Risks for Mode of Spread: 6 D’s
Dry: Arid climates facilitate the spread of dust and flies.
Dusty: Airborne particles can carry the bacteria.
Dirty: Unsanitary conditions promote bacterial transmission.
Density: Overcrowding increases contact between individuals.
Dung: Animal waste can harbor flies, which are vectors.
Discharge: Eye discharge from infected individuals contains the bacteria.
Mode of Transmission: 5 F’s
Fingers: Contaminated hands can transfer the bacteria to the eyes.
Flies: Certain fly species can mechanically transmit the bacteria from person to person.
Feces: Poor sanitation allows fecal contamination, which can harbor the bacteria.
Face: Direct contact with the face of an infected person can spread the infection.
Fomites: Contaminated objects like towels and clothes can transmit the bacteria.
Incubation period
The time between exposure to the bacteria and the onset of symptoms is typically 5 to 21 days.
Mode of infection
Direct spread: Transmission through close personal contact with an infected individual.
Vector transmission: Insects like bush flies and house flies carry and transmit the bacteria.
Material transfer: Sharing contaminated items like towels and clothing.
Clinical Features of Trachoma
The signs and symptoms can vary depending on whether a secondary bacterial infection is present. If a secondary bacterial infection exists, the symptoms may resemble bacterial conjunctivitis.
Conjunctiva appears congested: The lining of the eye appears red and inflamed.
Irregular scarring of the conjunctiva: Scar tissue develops on the conjunctiva.
The cornea shows superficial keratitis: Inflammation of the outer layer of the cornea.
Later corneal opacity and corneal ulcer may occur: The cornea may become cloudy, and open sores can develop.
Eye irritation: A feeling of discomfort or scratchiness in the eye.
Redness and itching: Inflammation causing visible redness and an itchy sensation.
Mucoid Discharge: Discharge that is thick and mucus-like.
Swelling of the eyelids: Inflammation causing the eyelids to become puffy.
Inflammation inside the upper eyelid: The inner lining of the upper eyelid becomes inflamed.
Scarring of the upper lid: Scar tissue formation on the inner surface of the upper eyelid.
Distortion of the upper eyelid: The shape of the upper eyelid may change due to scarring.
Development of eyelashes that turns into the eye lid then rub on the cornea causing entropion: Inward turning of the eyelashes, irritating the cornea. This condition is called entropion.
Abnormal growth of corneal blood vessels: Blood vessels invade the cornea as a result of chronic inflammation.
Foreign body sensations: A feeling that something is in the eye.
Stickiness of the lids: Eyelids may stick together, especially upon waking.
Keratitis: Inflammation of the cornea.
Conjunctival congestion: Redness and swelling of the conjunctiva.
Herbert follicles and Herbert pits develop: Specific inflammatory lesions on the conjunctiva.
Conjunctival scarring: Formation of scar tissue on the conjunctiva.
Corneal ulcer: An open sore on the cornea.
Corneal opacity: Clouding or loss of transparency of the cornea.
WHO classification of Trachoma (FISTO)
Trachomatous Follicular inflammation (TF): This indicates an active stage of the disease, characterized by the presence of at least five or more follicles (small bumps) in the upper conjunctiva, each larger than 0.5mm in diameter.
Trachomatous Intense inflammation (TI): Signifies a highly active inflammatory phase with noticeable thickening of the upper conjunctiva.
Trachomatous Scarring (TS): Visible scar tissue on the tarsal conjunctiva (the inner lining of the eyelid), appearing as white bands or thread-like fibrosis.
Trachomatous trichiasis (TT): A condition where at least one eyelash is turned inward, rubbing against the surface of the eye.
Trachomatous Corneal Opacity (CO): Significant clouding of the cornea within the pupillary area, resulting in reduced visual acuity (less than 6/18).
DIAGNOSIS :
History: Gathering information about the patient’s symptoms and medical background.
Physical examination: A visual inspection of the eyes.
Investigation: Collecting a sample of pus from the eye for laboratory analysis.
Management of Trachoma
Aims:
To prevent spread: Measures to stop the infection from transmitting to others.
To Relieve symptoms: Treatments aimed at reducing discomfort.
To prevent complications: Interventions to avoid long-term damage.
Admission: Hospitalization may be required in some cases.
Isolation: Separating the patient to prevent the spread of infection.
History taking: Collecting a detailed account of the patient’s illness.
Reassurance: Providing emotional support and explaining the treatment plan.
Observation: Monitoring the patient’s condition through physical and specific eye examinations.
Inform the ophthalmologist: Consulting with an eye specialist.
Investigations are done: Performing necessary laboratory tests.
Medical history is taken: Gathering information about the patient’s past health.
Medical Treatment: Using medications to treat the infection.
Medical management.
Topical application of antibiotics: Applying antibiotic ointments like 1% Tetracycline ointment three times a day for six weeks directly to the eye.
Erythromycin or azithromycin eyedrops: Administering these eyedrops four times daily for six weeks.
Systemic steroids: Oral medications like prednisolone or dexamethasone may be used to reduce inflammation and congestion.
Alternatively, doxycycline: An oral antibiotic, may be prescribed for 2-3 weeks, with the dosage adjusted based on the patient’s age.
Surgical management
Surgery is performed for in turned eyelids (entropion): A procedure to correct the inward turning of the eyelid.
Electrolysis: Using an electrical current to destroy the hair follicle of an ingrown eyelash.
Cryotherapy: Freezing and thawing the follicle to remove an ingrown eyelash.
Argon laser treatment: Using a laser to destroy the follicle of an ingrown eyelash.
Nursing Care
Regular cleaning of the eyes: Keeping the eyes clean to remove discharge and debris.
Disinfect equipment used: Preventing the spread of infection by disinfecting any tools used in patient care.
Ironing and cleaning linens: Destroying bacteria on bedding and clothing through heat.
Encourage hand washing: Promoting proper hygiene to prevent the spread of infection.
Barrier nursing measures: Implementing precautions to prevent the transmission of infection.
Nutrients: Ensuring adequate intake of protein and vitamins to support healing.
Rest and sleep: Allowing the body to recover.
Reassurance: Providing emotional support to the patient.
Advice on discharge: Providing instructions for continued care at home.
Health education on environmental change: Educating on ways to improve sanitation and hygiene.
Drug compliance: Emphasizing the importance of taking medications as prescribed.
Increase access to clean water and sanitation: Advocating for improved community resources.
Nursing Diagnosis for Trachoma
Acute pain: eye related to swelling of the lymph nodes, photophobia and inflammation: Pain in the eye associated with swollen lymph nodes, light sensitivity, and inflammation.
Disturbed Sensory Perception: Visual related to damage to the cornea: Changes in vision due to corneal damage.
Risk for infection, the spread related to lack of knowledge: Potential for the infection to spread due to inadequate understanding of transmission.
Body image disorders related to loss of vision: Negative self-perception stemming from vision loss.
Complications.
Trichiasis: Inward growth of eyelashes that rub on the cornea and conjunctiva.
Entropion: Eyelid turned inward against the eyeball due to muscle spasm or scarring of the conjunctiva.
Keratitis: Inflammation of the cornea.
Ptosis: Abnormal drooping of the upper eyelid.
Secondary glaucoma: Elevated eye pressure as a consequence of trachoma.
Corneal opacity, blindness: Clouding of the cornea leading to vision loss.
Preventive Measures
Avoid physical contact with a person suffering from trachoma: Limiting direct contact with infected individuals.
Personal cleanliness especially the face and hands: Maintaining good hygiene practices.
Washing hands and face frequently with soap and water: Regular handwashing is crucial.
Keep separate towels, handkerchiefs, linens for each member of the family: Avoiding sharing personal items.
Use latrines to dispose off faeces covered with lid: Proper sanitation practices.
Avoid crowded places: Reducing exposure in densely populated areas.
Wash, hang, dry and iron all linens: Disinfecting clothing and bedding.
Good hygiene during deliveries: Preventing transmission to newborns.
Avoid eye makeup: Reducing the risk of introducing bacteria.
Spray flies: Controlling fly populations.
Clean compounds to keep away flies: Maintaining a clean environment to discourage flies.
Early diagnosis and treatment: Seeking prompt medical attention.
Prevention (SAFE) Strategy by WHO.
S= Surgery: Surgical intervention for trichiasis, entropion, or corneal opacity.
A=Antibiotics: Administering antibiotics such as a single dose of Azithromycin 500mg.
F= Facial cleanliness: Promoting regular face washing.
E= Environmental Improvement: Improving access to clean water and sanitation facilities.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

