Special Investigations in Surgical Nursing
Subtopic:
Tetanus
Tetanus is a serious acute infectious disease affecting the central nervous system. The primary cause is the bacterium Clostridium tetani. A key symptom of tetanus is muscle spasms, often initially affecting the muscles of the jaw.
Tetanus is commonly known as ‘Lock-jaw.’
The popular name for tetanus, “Lock-jaw,” highlights a prominent symptom where the jaw muscles become tightly contracted.
Tetanus is a severe bacterial infection characterized by intermittent spasms (twitching) of voluntary muscles.
This is a serious bacterial infection. A defining feature is the occurrence of sporadic and involuntary muscle contractions throughout the body.
It is caused by the neurotoxin tetanospasmin produced byClostridium tetani, an anaerobic bacterium commonly found in soil, dust, and animal feces. The incubation period ranges from a few days to several weeks (averaging 7-10 days), with shorter periods indicating a more severe infection.
The illness is triggered by tetanospasmin, a potent neurotoxin released by Clostridium tetani. This bacterium thrives in environments lacking oxygen (anaerobic), frequently found in soil, dust, and animal waste. The time between infection and symptoms (incubation period) varies, typically around 7-10 days, but a shorter duration often suggests a more aggressive form of the disease.
Causative Agent and Transmission:
Tetanus is caused by the exotoxins of clostridiumtetani.
The root cause of tetanus lies in the exotoxins, specifically tetanospasmin, produced by the bacterium Clostridium tetani.
The causative agent is Clostridium tetani, whose spores enter the body through various routes:
The infectious agent is Clostridium tetani, and its resilient spores can gain entry into the body in several ways:
Deep penetrating wounds: Injuries that pierce the skin deeply, like puncture wounds, lacerations, burns, and crush injuries, create an oxygen-free environment where spores can germinate. Umbilical cord: In newborns, particularly in cases of neonatal tetanus, infection can result from using unhygienic methods on the umbilical cord stump. Other routes: Less common entry points include ear infections, wounds sustained during childbirth, and septic abortions.
The organism can live for a long time in any condition, especially dirty environments. So it can be found in dust, soil, or grass.
The tetanus-causing bacteria can survive for extended periods in diverse conditions, particularly in unsanitary places like dust, soil, and even on grass.
The clostridia can be normal organisms in the alimentary canal of animals but when passed out and gain entry to the human body, they become harmful. The organism can be found in cows, horse, sheep, or goat.
While Clostridium tetani can exist harmlessly in the digestive systems of animals, it becomes pathogenic when it enters the human body through wounds. Animals such as cows, horses, sheep, and goats can carry the bacteria.
Incidence of tetanus:
In babies born at home before arrival at the hospital.
The occurrence of tetanus is higher in infants delivered at home before reaching a healthcare facility.
In homes where domestic animals are kept.
The risk of tetanus infection is also elevated in households where domestic animals are present.

Pathophysiology of Tetanus
The development of tetanus begins with the introduction of Clostridium tetani bacteria or their hardy spores into the body. This typically happens through deep puncture wounds or cuts. These bacteria thrive and reproduce in areas with little to no oxygen (anaerobic conditions). It’s important to understand that any wound that isn’t properly cleaned presents a notable risk for tetanus infection. Once Clostridium tetani establishes itself within the wound, it releases two types of potent toxins into the nearby tissues: tetanospasmin and tetanolysin.
Tetanospasmin, the more influential toxin, is key to the observable symptoms of the disease. Its primary target is the central nervous system (CNS). Specifically, the toxin interferes with the function of motor nerve cells located in the spinal cord and the brain. This interference disrupts normal nerve signaling, leading to the characteristic muscle spasms in the muscles controlled by the affected nerves.
Route of entry
The Clostridium tetani bacteria can enter the body through a number of ways, each potentially leading to infection:
Infected ulcerated wound: Open sores or ulcers that become infected can provide an entry point.
Postoperative wounds: Surgical incisions, if not properly cared for, can become infected.
Umbilical stumps (in newborns): In newborns, especially when delivery occurs in non-sterile environments, the umbilical cord stump is a vulnerable point of entry.
Gun-shot wounds: The nature of gunshot injuries, often deep and introducing foreign material, creates a high risk.
Septic abortion: Infections related to unsafe abortions can allow the bacteria to enter the body.
Jiggers or foreign bodies: Penetration of the skin by parasites like jiggers or other foreign objects can introduce the bacteria.
Burns and scalds: Damaged skin from burns creates an opening for infection.
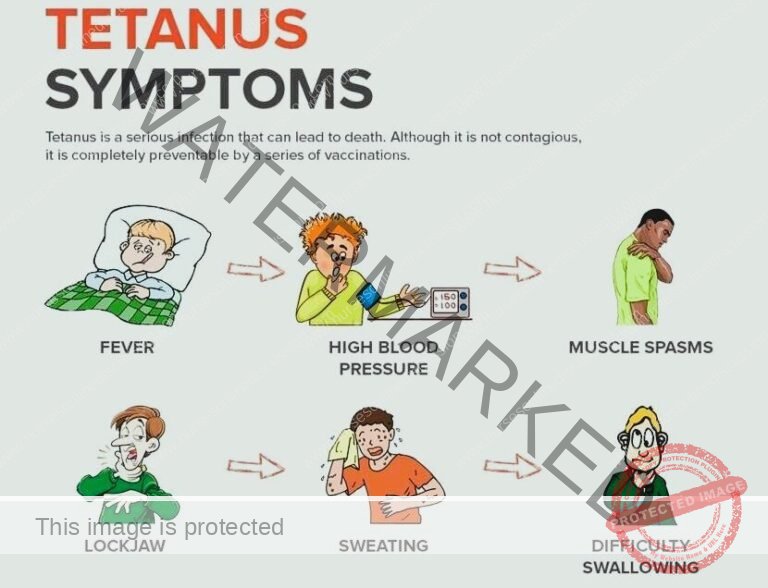
Clinical Features of Tetanus:
The start of symptoms usually involves localized muscle stiffness, which then progresses to more widespread signs:
Trismus (Lockjaw): Indicated by difficulty in opening the mouth because of spasms in the masseter muscles responsible for chewing. This stiffness is an early and noticeable sign, primarily affecting the jaw muscles. The spasms in the facial muscles, especially those in the cheek and jaw, make opening the mouth a struggle, hence the term trismus.
Risus sardonicus: A distinctive facial expression resembling a grimace or a sardonic smile. The corners of the mouth are pulled back and upwards, creating this characteristic forced-looking smile, also known as the “Devil’s grin“.
Dysphagia: Problems with swallowing. The muscle spasms affect the muscles of the mouth and throat (esophagus), making it difficult to move food and liquids down.
Weight loss: Can occur as a consequence of the difficulties in eating. The inability to swallow comfortably or effectively can lead to reduced food intake and ultimately starvation if severe.
Muscle spasms: Intense and painful, these spasms typically begin in the jaw and neck area before spreading to other muscle groups in the body. These spasms can be triggered by external stimuli such as loud sounds or bright light, highlighting the nervous system’s heightened sensitivity.
Opisthotonos: A severe and dramatic arching of the back due to powerful muscle contractions. Despite the intensity of the spasms, the patient remains conscious. The head is forced backwards, and the spine arches significantly due to the rigidity of the neck and back muscles, a condition referred to as opisthotonus.
Fever: Often present as the body responds to the infection. Patients may have an elevated body temperature and an increased heart rate (rapid pulse).
Signs of inflammation: Indicators of infection may be noticeable, especially around the entry point. In newborns, this might include swelling of the umbilical cord, a persistently moist cord, an unpleasant odor, or pus discharge from the wound site.
Respiratory distress: A dangerous complication caused by spasms in the muscles responsible for breathing. These spasms can lead to respiratory failure, a life-threatening situation. The spasms in the respiratory muscles can cause prolonged periods without oxygen (anoxia), which can be fatal.
Autonomic nervous system instability: Indicates that the part of the nervous system controlling involuntary functions is affected. This can result in unpredictable changes in blood pressure, excessive sweating, and a rapid heartbeat (tachycardia).
Hyperreflexia: Overly active or exaggerated reflexes. The body’s normal reflex responses become more pronounced and intense.
Absence of a visible wound: A tetanus diagnosis is still possible even without an obvious injury. The infection can sometimes occur through minor or unnoticed breaks in the skin.
Spasms of the sphincters: Contraction of the muscles that control the release of urine and stool. This can lead to retention of urine or stool. In severe cases, the pressure from these spasms can even cause sphincter rupture.
Patients may have a wound or a history of a wound: Often, there is evidence of an injury that could have served as the entry point for the tetanus bacteria.
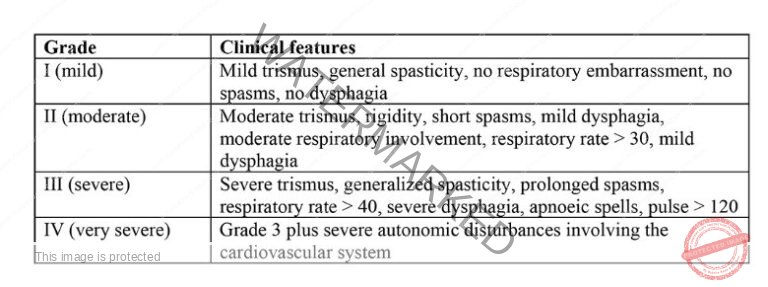
Alblett Classification of Tetanus
There are several ways to categorize the severity of tetanus. The Ablett classification system is a commonly used method to grade patients based on the intensity of their muscle spasms and the involvement of their respiratory and autonomic systems.
Management of Tetanus
Tetanus has no definitive cure, making immediate and ongoing supportive care crucial while the illness runs its course.
Aims of Management
The primary goals of tetanus management are: controlling muscle spasms, eliminating the Clostridium tetani bacteria and its toxins, preventing complications, and ensuring the patient receives adequate nutrition.
Specific treatment measures include:
Penicillin: Administering penicillin is a critical intervention to destroy the tetanus-causing bacteria.
Anti-tetanus serum: Giving anti-tetanus serum is important for neutralizing the toxins that have been released and stopping them from causing further damage.
Sedation and muscle relaxants: Medications such as diazepam and chlorpromazine are used to calm the patient and relax their muscles, effectively reducing the severity of spasms and making them more comfortable.
Wound management: If a wound exists as the entry point for the bacteria, removing dead or damaged tissue (debridement) is essential. The wound is also thoroughly cleaned with hydrogen peroxide. Leaving the wound open, instead of stitching it closed, helps expose it to oxygen, which inhibits the growth of the anaerobic Clostridium tetani bacteria.
Neutralizing the Toxin:
Tetanus Immunoglobulin (TIG): Administering human TIG is vital to neutralize the toxins circulating in the body. The dosage depends on the patient’s age and the severity of the contamination:
Adults and children: 150 IU/kg is given, ensuring it’s injected into at least two different muscles (IM sites) and away from where the tetanus toxoid vaccine is given.
Neonates: 500 IU IM is administered, also split between at least two different muscle injection sites.
Tetanus Toxoid (TT) or DPT: Giving the appropriate vaccine, either TT or DPT, immediately is necessary to develop active immunity against tetanus. Specific vaccination schedules for different age groups should be followed.
Eliminating the Source of Toxin:
Wound management: Thorough cleaning and debridement of any wounds are essential to remove dead tissue and get rid of the source of the bacteria. In cases of neonatal tetanus, meticulous cleaning and debridement of the umbilical stump are especially important.
Antibiotic Treatment:
First-line: Metronidazole is typically the first choice, given intravenously or orally. The adult dose is 500 mg every 8 hours for 7 days, while the children’s dose is 7.5 mg/kg every 8 hours.
Second-line: If metronidazole isn’t suitable, benzylpenicillin is an alternative. The adult dosage is 2.5 MU every 6 hours for 10 days. For children, the dose is 50,000-100,000 IU/kg per dose, and for newborns, it’s 100,000 IU/kg every 12 hours for 10-14 days.
Control of Muscle Spasms:
First-line: Diazepam is often the first medication used, administered intravenously or rectally. The adult dose is 10 mg every 1-4 hours, while for children, it’s 0.2 mg/kg IV or 0.5 mg/kg rectally every 1-4 hours, with a maximum dose of 10mg. For newborns, the dosage is 0.2 mg/kg IV or 0.5 mg/kg rectally every 1 to 4 hours. Other agents: Magnesium sulfate can be used either alone or with diazepam, and chlorpromazine can also be used alone or alternating with diazepam. It’s important to watch for side effects like respiratory depression with diazepam and loss of the knee-jerk reflex with magnesium sulfate. The chlorpromazine dosage for newborns is 1 mg/kg orally every 8 hours via a nasogastric tube (NGT).
Pain Control:
Morphine: Can be used to manage pain, given intravenously. The adult dose is 2.5-10 mg every 4-6 hours, and it’s crucial to monitor for respiratory depression. For children, the dose is 0.1 mg/kg per dose.
Paracetamol: Another option for pain relief, given every 8 hours for adults at a dose of 1 g. For children, the dose is 10 mg/kg every 6 hours.
Prevention:
Routine childhood immunization: Ensuring all children receive the recommended tetanus toxoid-containing vaccines (such as DTP, Tdap, or Td) according to the national immunization schedule is a fundamental preventative measure.
Proper wound care: Taking care of wounds promptly and appropriately, including cleaning and debridement, significantly lowers the risk of tetanus infection.
Prophylactic TIG: Administering TIG preventatively is recommended for individuals with contaminated wounds who have incomplete or unknown tetanus immunization status. The dosage varies by age:
Children < 5 years: 75 IU
Children 5-10 years: 125 IU
Children > 10 years and adults: 250 IU
Wound care: Proper care of wounds, including thorough cleaning and removing any dead or damaged tissue (debridement), is a crucial step in preventing infection.
Control of spasms involves the following measures:
Absolute rest and isolation: Keeping the patient in a quiet, dimly lit room helps to minimize things that might trigger spasms.
Prevention of external stimuli: Taking steps like using soft-closing mechanisms on doors helps prevent loud noises that could cause spasms.
Warming hands before touching: Nurses should warm their hands before touching the patient to avoid any sudden sensations that might initiate spasms.
Medication administration: Sedatives and muscle relaxants, such as chlorpromazine (Largactil) and Diazepam, are given regularly through a nasogastric tube to maintain a calm state and reduce spasms.

General Management:
Close observation and airway management: Continuous monitoring of the patient is essential. Ensuring the airway remains clear, potentially using a mucous extractor to remove secretions, is a priority to prevent breathing difficulties.
Vital signs monitoring: Regular checks of the patient’s temperature, pulse, and respiratory rate are necessary to track their condition. Detailed recording of spasm characteristics, including their strength, how often they occur, how long they last, and which body parts are affected (using a spasm chart), is vital for assessment.
Nutrition: Maintaining adequate nutrition is crucial for recovery. Nasogastric tube feeding is preferred to avoid triggering spasms that could be caused by injections. Care must be taken to prevent aspiration, where fluids enter the airway.
Catheterization: Inserting a urinary catheter helps ensure proper emptying of the bladder, especially if the patient is unable to do so themselves.
Fluid balance chart: Carefully tracking fluid intake and output is important to maintain proper hydration. Initially, intravenous fluids may be necessary before transitioning to nasogastric tube feeding.
Hygiene: Daily care includes cleaning the umbilical cord with normal saline in newborns, and meticulous oral care to prevent infection. Turning the patient every two hours helps prevent pressure sores from developing.
Vaccination: To prevent future tetanus cases, it’s crucial to ensure all individuals receive the complete course of the DPT (diphtheria, pertussis, and tetanus) vaccine.
Use sterile equipment: Employing sterile equipment during all medical procedures is essential to prevent cross-infection.
Bowel and bladder care: Monitoring and assisting the patient with bowel movements and urination is part of the supportive care.
Medication: Administering all prescribed medications as directed is critical for managing the condition.
Physiotherapy: Incorporating physiotherapy sessions with deep breathing exercises and active limb
movements can aid in recovery.
Complications of Tetanus
Fracture of bones or the spine: The powerful and repeated muscle spasms can generate enough force to cause fractures, particularly in the bones or spine, especially if the spasms are severe and uncontrolled.
Pneumonia: When patients are heavily sedated to control spasms, their breathing may become shallow, and they might have difficulty clearing their airways. This increases the risk of pneumonia, a serious lung infection.
Brain damage: The potent toxins released by the tetanus bacteria can affect the central nervous system, potentially leading to brain damage in severe cases.
Growth retardation: In children with tetanus, the illness can interfere with their ability to get proper nutrition, which can hinder their growth and development, leading to growth retardation.
Exhaustion: The constant and intense muscle spasms require a significant amount of energy, leading to extreme exhaustion and weakening the patient.
Respiratory failure: If the spasms affect the muscles involved in breathing, it can lead to respiratory failure, where the patient cannot breathe adequately on their own and may require support.
Retention of urine: Spasms in the muscles of the pelvic region can cause the sphincters controlling urine flow to tighten, leading to difficulty urinating and potential urine retention.
Death due to airway obstruction: In the most severe cases, the intense spasms, particularly in the jaw and neck muscles, can block the airway, leading to suffocation and potentially death.
Test Questions
Which bacterium causes tetanus?
a) Streptococcus pyogenes
b) Staphylococcus aureus
c) Clostridium tetani
d) Escherichia coli
Answer: c) Clostridium tetani
Explanation: Clostridium tetani is the bacterium responsible for causing tetanus.
What is the common term used to describe tetanus due to spasms in the jaw muscles?
a) Trismus
b) Opisthotonus
c) Risus sardonicus
d) Tetanospasmin
Answer: a) Trismus
Explanation: Trismus is the medical term for difficulty in opening the mouth due to jaw muscle spasms, which is commonly known as “Lock-jaw.”
What is the primary goal of managing tetanus?
a) Preventing complications
b) Destroying the toxin
c) Controlling fever
d) Alleviating pain
Answer: a) Preventing complications
Explanation: The main aim of managing tetanus is to prevent complications associated with the disease and ensure the best possible outcome for the patient.
What is the specific treatment given to destroy the tetanus-causing organism?
a) Penicillin
b) Paracetamol
c) Aspirin
d) Ibuprofen
Answer: a) Penicillin
Explanation: Penicillin is administered to destroy the Clostridium tetani bacterium responsible for causing tetanus.
Which complication of tetanus can lead to respiratory failure?
a) Pneumonia
b) Fracture of bones
c) Brain damage
d) Respiratory muscle spasms
Answer: d) Respiratory muscle spasms
Explanation: Tetanus-induced spasms affecting the respiratory muscles can lead to respiratory failure, where the patient is unable to breathe adequately on their own.
Why is the use of a mucous extractor important in tetanus management?
a) To prevent dehydration
b) To clear the airway
c) To alleviate muscle spasms
d) To prevent fever
Answer: b) To clear the airway
Explanation: A mucous extractor is used to clear the airway and prevent obstruction caused by excessive secretions, which is crucial in tetanus management.
What is the recommended method for feeding tetanus patients to avoid spasms triggered by injections?
a) Intravenous feeding
b) Nasogastric tube feeding
c) Oral feeding
d) Intramuscular injections
Answer: b) Nasogastric tube feeding
Explanation: Nasogastric tube feeding is used to provide nutrition and administer drugs to tetanus patients while avoiding the stimulation of spasms caused by intramuscular injections.
Which immunization should be given to prevent future tetanus cases?
a) Hepatitis B
b) Measles, Mumps, and Rubella (MMR)
c) Diphtheria, Pertussis, and Tetanus (DPT)
d) Polio
Answer: c) Diphtheria, Pertussis, and Tetanus (DPT)
Explanation: The DPT vaccine provides immunity against diphtheria, pertussis (whooping cough), and tetanus, preventing future tetanus cases.
What measure can be taken to prevent tetanus in newborns with umbilical stumps?
a) Cleaning the stump with cow dung
b) Applying native medicine on the stump
c) Keeping the stump dry and clean
d) Ignoring the stump until it falls off naturally
Answer: c) Keeping the stump dry and clean
Explanation: Maintaining cleanliness and dryness of the umbilical stump can prevent infection and the risk of tetanus in newborns.
What is the purpose of physiotherapy in tetanus management?
a) To provide pain relief
b) To promote muscle strength
c) To control spasms
d) To increase body temperature
Answer: b) To promote muscle strength
Explanation: Physiotherapy aims to promote muscle strength and mobility, which can be helpful in the recovery process of tetanus patients.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

