Psychopharmacology
Subtopic:
Anticonvulsants
Anticonvulsant medications, also known as antiepileptic drugs, are a class of pharmaceuticals designed to prevent or manage seizures or convulsions. They achieve this by regulating irregular electrical activity within the brain.
Common Terms
Absence Seizure: A type of generalized seizure characterized by a sudden, brief lapse in consciousness, sometimes accompanied by staring or rapid blinking lasting a few seconds. This was previously known as a petit mal seizure.
Antiepileptic: A medication specifically used to treat epilepsy by counteracting the abnormal and excessive bursts of electrical energy in the brain that are characteristic of this condition.
Convulsion: The involuntary, forceful muscle contractions (tonic-clonic reactions) resulting from excessive electrical discharge from nerve cells in the brain.
Epilepsy: A neurological condition encompassing a spectrum of syndromes, all defined by the recurring occurrence of seizures.
Generalized Seizure: A seizure that starts in one area of the brain and quickly involves both hemispheres, leading to widespread electrical disturbance.
Partial Seizures: Also referred to as focal seizures, these seizures originate in a specific area of the brain and do not spread to the entire brain. They may manifest with varied symptoms depending on the affected brain region.
Seizure: A sudden, uncontrolled surge of electrical activity in the brain, triggered by nerve cells becoming excessively active and excitable.
Status Epilepticus: A dangerous condition characterized by seizures that occur in rapid succession or as a continuous, prolonged seizure. It is the most severe form of generalized seizure and requires immediate medical intervention.
Tonic-Clonic Seizure: A type of generalized seizure involving distinct phases: a tonic phase marked by muscle rigidity, followed by a clonic phase of rhythmic muscle contractions and relaxation. Consciousness is lost, and upon regaining awareness, there is typically exhaustion and limited recall of the event. This was formerly termed a grand mal seizure.
A seizure arises from an abrupt, uncontrolled surge of electrical signals in the brain. This neurological event is triggered when brain cells, or neurons, become overly active.
Seizures are broadly categorized into two main types based on their origin in the brain:
Focal Seizures: These seizures begin in a localized area of the brain, typically within one hemisphere. They can occur with or without affecting a person’s awareness or consciousness.
Generalized Seizures: These seizures involve both hemispheres of the brain from the onset. They almost invariably lead to a loss of consciousness.
Seizures can be understood as the result of an imbalance in the brain’s neurochemical processes, specifically between inhibitory and excitatory mechanisms. This imbalance leads to either insufficient inhibitory activity or excessive excitatory activity in the brain.
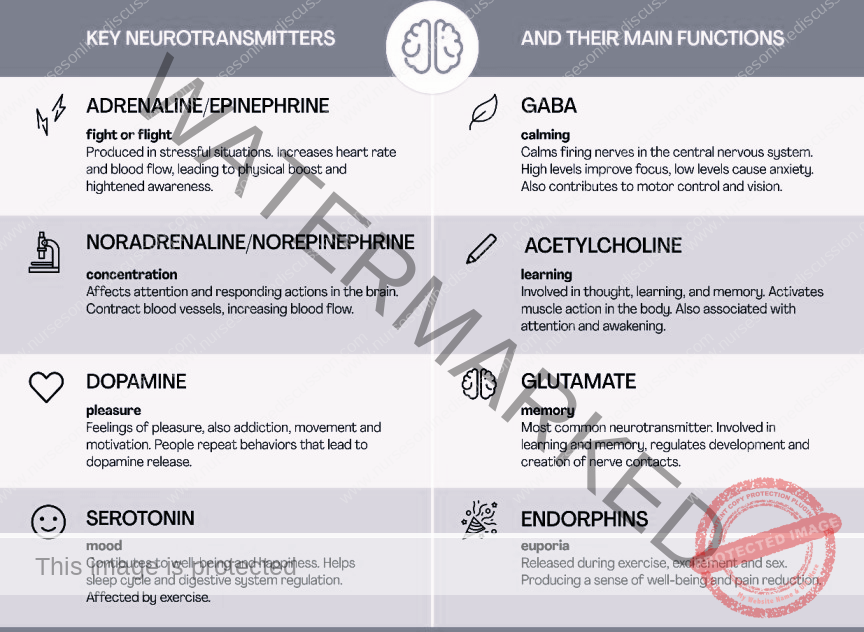
Inhibition and Excitation Neurotransmitters
Neurotransmitters play a critical role in brain function, acting as chemical messengers. They are broadly classified based on their effects:
Excitatory Neurotransmitters: These neurotransmitters stimulate neurons, making them more likely to transmit an electrical signal. They essentially “activate” the neuron, allowing the message to propagate to the next nerve cell. Examples include glutamate, epinephrine, and norepinephrine.
Inhibitory Neurotransmitters: These neurotransmitters have the opposite effect; they reduce the excitability of neurons, making them less likely to transmit a signal. They function to “block” or prevent a message from continuing to be passed along. Examples of inhibitory neurotransmitters are gamma-aminobutyric acid (GABA), glycine, and serotonin.
Modulatory Neurotransmitters: These neurotransmitters do not directly excite or inhibit neurons in the same way. Instead, they refine or adjust the communication between cells at synapses. They can influence the effects of excitatory and inhibitory neurotransmitters, often affecting larger groups of neurons simultaneously to fine-tune brain activity.
DRUGS FOR TREATING GENERALIZED SEIZURES
Medications employed to manage generalized seizures primarily work by stabilizing nerve cell membranes. This stabilization is achieved by either blocking ion channels within the cell membrane or by modulating receptor sites. Due to their broad action on the central nervous system (CNS), side effects such as sedation and other CNS-related effects are common.
Several drug classes are utilized for generalized seizures, including:
Hydantoins
Barbiturates and Barbiturate-Like Drugs
Benzodiazepines
Succinimides
Oxazolidinediones
Sulfonamides
Valproates / Valproic Acid Derivatives
These medications exert a widespread effect on the brain, reducing the likelihood of sudden, uncontrolled electrical discharges that characterize generalized seizures.
Hydantoins
This class includes medications such as ethotoin (Peganone) and phenytoin (Dilantin). Hydantoins are often preferred due to their lower sedative properties compared to other antiepileptic drugs, making them suitable for patients who wish to minimize sedation. However, they are associated with notable adverse effects, which has led to the increased use of less toxic alternatives like benzodiazepines in many clinical scenarios.
Indications of Hydantoins:
Management of tonic-clonic and psychomotor seizures.
Short-term control of status epilepticus.
Prophylaxis against seizures following neurosurgical procedures.
Dose (Phenytoin as example):
Adults: Oral: 100 mg three times daily, adjusted up to 300–400 mg/day; IV: 10–15 mg/kg.
Children: Oral: 5–8 mg/kg per day; IV: 5–10 mg/kg in divided doses.
Contraindications of Hydantoins:
Known hypersensitivity to hydantoin medications.
Pregnancy and lactation: Hydantoins are linked to potential birth defects and are generally avoided unless seizure control benefit outweighs fetal risk. Women of childbearing potential should use effective barrier contraception.
Adverse Effects:
Neurological: Nystagmus (involuntary eye movements), ataxia (loss of coordination), slurred speech, depression, confusion, drowsiness, lethargy, fatigue.
Gastrointestinal: Constipation, dry mouth, anorexia.
Cardiovascular: Cardiac arrhythmias, blood pressure fluctuations.
Genitourinary: Urinary retention, loss of libido.
Barbiturates and Barbiturate-Like Drugs
Barbiturates and similar drugs act by inhibiting nerve impulse transmission in the ascending reticular activating system (RAS), depressing the cerebral cortex, altering cerebellar function, and reducing motor nerve output. They stabilize neuronal membranes throughout the CNS by influencing ion channels, thereby decreasing neuronal excitability and reducing hyper-responsiveness to stimuli.
Indications:
Treatment of tonic-clonic and absence seizures.
Anxiolytic and hypnotic applications.
Emergency management of status epilepticus and acute seizures related to eclampsia, tetanus, and other conditions.
Treatment of cortical focal seizures.
Dose (Phenobarbital as example):
Adults: Oral: 60–100 mg/day; IM or IV for acute episodes: 200–320 mg, may repeat in 6 hours; dosage adjustment needed for elderly and those with renal or hepatic impairment.
Children: Oral: 3–6 mg/kg per day; IM or IV: 4–6 mg/kg per day; IV for status epilepticus: 15–20 mg/kg over 10–15 minutes.
Contraindications and Adverse Effects: Similar to hydantoins.
Benzodiazepines
Benzodiazepines enhance the effects of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter that stabilizes nerve cell membranes. These drugs primarily act in the limbic system and the RAS, inducing muscle relaxation and reducing anxiety without significantly impairing cortical function. They stabilize nerve membranes across the CNS, reducing both general excitability and hyper-excitability.
Indications:
Management of absence and myoclonic seizures.
Treatment of severe convulsions, tonic-clonic seizures, status epilepticus.
Management of alcohol withdrawal and tetanus.
Relief of tension and preoperative anxiety.
Used for patients unresponsive to succinimides.
Investigational uses include panic attacks, restless leg syndrome, hyperkinetic dysarthria, acute manic episodes, tic disorders, and neuralgias.
Dose (Diazepam as example):
Adults: Oral: 2–10 mg twice to four times daily; Rectal: 0.2 mg/kg PRN, may repeat in 4–12 hours; IM or IV: 2–20 mg.
Geriatric/Debilitated: Oral: 2–2.5 mg twice daily; IM or IV: 2–5 mg.
Pediatric: Oral: 1–2.5 mg three to four times daily; Rectal: 0.3–0.5 mg/kg.
Contraindications and Adverse Effects: Similar to hydantoins.
DRUGS FOR TREATING PARTIAL SEIZURES
Partial seizures can be categorized as simple (affecting a single muscle or function) or complex (involving sequences of actions or emotional changes). Medications for partial seizures include carbamazepine, among others. Some drugs effective for generalized seizures are also beneficial in treating partial seizures.
These drugs control partial seizures by stabilizing nerve membranes either directly, by modulating sodium and calcium channels, or indirectly, by enhancing GABA activity, thereby reducing excessive neuronal activity.
Carbamazepine and oxcarbazepine are often used as monotherapy, while other drugs in this category serve as adjunctive treatments.
Carbamazepine
Indications:
First-line treatment for partial seizures and tonic-clonic seizures.
Management of trigeminal neuralgia and bipolar disorder.
Dose:
Adults: Oral: 800–1200 mg/day in divided doses every 6–8 hours.
Pediatric (> 12 years): Adult doses, not exceeding 1000 mg/day.
Pediatric (6–12 years): Oral: 20–30 mg/kg per day in divided doses three to four times daily.
Pediatric (< 6 years): Oral: 35 mg/kg per day.
Gabapentin
Indications:
Adjunctive therapy for partial seizures.
Management of postherpetic neuralgia in adults and children (3–12 years), migraines, bipolar disorders.
Treatment of tremors in multiple sclerosis and nerve-related pain conditions.
Dose:
Adults: Oral: 900–1800 mg/day in divided doses three times daily.
Pediatric (3–12 years): Oral: 10–15 mg/kg per day in divided doses.
Contraindications and Adverse Effects for Partial Seizure Medications:
Contraindications:
Known allergy to the specific drug.
Bone marrow suppression, which can be exacerbated by these drugs.
Severe hepatic dysfunction, which can interfere with drug metabolism.
Pregnancy: Carbamazepine, clorazepate, gabapentin, and oxcarbazepine have shown potential fetal risks and should be avoided during pregnancy. Women of childbearing age should use contraception.
Lactation: These drugs can pass into breast milk and potentially harm the infant. Alternative feeding methods should be considered if these medications are necessary during breastfeeding.
Adverse Effects:
Neurological: Drowsiness, fatigue, weakness, confusion, headache, insomnia.
Gastrointestinal: GI distress including nausea, vomiting, and anorexia.
Respiratory: Upper respiratory infections.
Hematologic/Hepatic: Potential liver toxicity and bone marrow suppression.
Nursing Considerations for Patients Receiving Anticonvulsants
Assess Contraindications and Cautions: Verify for allergies to anticonvulsants to prevent hypersensitivity reactions.
Medical History Review: Check for a history of bone marrow suppression or renal stones, which could be worsened by these medications.
Hepatic and Renal Function: Evaluate for pre-existing renal or hepatic dysfunction that might affect drug metabolism and excretion.
Pregnancy and Lactation Status: Determine current pregnancy or lactation status, as these conditions may contraindicate or require caution when using these drugs.
Skin Assessment: Inspect skin for color and lesions to detect potential dermatological side effects.
Cardiovascular Assessment: Monitor pulse, blood pressure, and auscultate heart sounds to assess for cardiac effects.
Neurological Assessment: Evaluate level of orientation, affect, reflexes, and grip strength to identify CNS effects.
Gastrointestinal and Genitourinary Assessment: Monitor bowel sounds and urine output to detect GI or GU effects.
Renal and Liver Function Tests: Assess renal and liver function via lab tests to determine therapy appropriateness and need for dose adjustments.
Hematologic Monitoring: Regularly check urinalysis and complete blood count (CBC) with differential to monitor for bone marrow function changes.
Nursing Diagnoses
Acute Pain related to GI and CNS effects.
Disturbed Thought Processes related to CNS effects.
Risk for Injury related to CNS effects.
Risk for Infection related to bone marrow suppression.
Deficient Knowledge regarding drug therapy.
Implementation with Rationale
Administer with Food: Give medication with food to lessen GI irritation.
Monitor CBC: Check CBC before and periodically during therapy to detect and manage bone marrow suppression.
Infection Precautions: Protect patient from infection if bone marrow suppression occurs.
Discontinuation for Adverse Reactions: Stop drug if rash, bone marrow suppression, depression, or personality changes arise to prevent severe adverse effects.
Gradual Withdrawal: Discontinue drug slowly; abrupt withdrawal can precipitate seizures.
Counseling for Women of Childbearing Age: Counsel women about the risk of fetal harm and advise barrier contraception.
Safety Measures: Implement safety precautions to prevent injury from CNS effects.
Patient Education: Provide comprehensive teaching on drug name, dosage, adverse effects, warning signs, and need for regular lab tests to promote adherence and safety.
Evaluation
Monitor Therapeutic Response: Assess for reduced seizure frequency or absence.
Monitor for Adverse Effects: Evaluate for CNS changes, GI distress, bone marrow suppression, skin reactions, liver toxicity, renal stones.
Evaluate Teaching Effectiveness: Verify patient understanding of drug regimen, adverse effects, and safety measures.
Long-Term Therapy Considerations: Educate patients on the chronic nature of epilepsy management and the importance of long-term adherence and lifestyle adjustments.
MULTIPLE CHOICE QUESTIONS
c. The most prevalent neurological disorder.
d. Complex seizures.
b. Carry a Medical form identification.
a. barbiturates, benzodiazepines, and hydantoins.
c. carbamazepine.
c. involve only part of the brain.
a. carbamazepine.
b. stabilizing overexcited nerve membranes.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

