Psychopharmacology
Subtopic:
Anxiolytic and Hypnotic Agents
Anxiolytic agents are medications designed to depress the central nervous system (CNS). Their purpose is to alleviate the signs and symptoms associated with anxiety.
Hypnotic agents are also CNS depressants, but their primary function is to induce sleep.
Common Terms
Anxiety: This is an uncomfortable sensation of strain, apprehension, or unease in response to a stimulus in the environment. This stimulus can be real or imagined.
Barbiturate: Historically, barbiturates were a primary class of drugs for treating anxiety, inducing sedation, and promoting sleep. However, their use has become less favored due to potentially severe adverse effects and numerous interactions with other drugs.
Benzodiazepine: This type of medication acts on the limbic system and the reticular activating system. It enhances the effectiveness of gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter. This enhancement leads to reduced neuron firing. Benzodiazepines depress the CNS to alleviate anxiety symptoms and can induce sedation and hypnosis at higher doses.
Hypnosis: This represents a state of profound sedation, resulting in significant CNS depression and sleep.
Sedation: This is a state of reduced awareness and responsiveness to environmental stimuli.
Sedative: A sedative is a drug that works by depressing the CNS. It leads to a diminished awareness of and reaction to the surrounding environment.
Drugs Used as Anxiolytic and Hypnotic Agents
| BENZODIAZEPINES USED AS ANXIOLYTICS | BARBITURATES USED AS ANXIOLYTIC-HYPNOTICS | OTHER ANXIOLYTIC AND HYPNOTIC DRUGS |
| alprazolam (Xanax) | phenobarbital | promethazine (Phenergan) |
| diazepam (Valium) | butabarbital | zolpidem |
| clonazepam | amobarbital | buspirone |
| oxazepam | pentobarbital | meprobamate |
BENZODIAZEPINES USED AS ANXIOLYTICS
Benzodiazepines are the most frequently prescribed medications for anxiety. They are effective in reducing anxiety symptoms without typically causing significant drowsiness at typical anxiolytic doses. Furthermore, compared to older sedative-hypnotics used for anxiety relief, benzodiazepines are considered to have a lower risk of causing physical dependence.
Dose
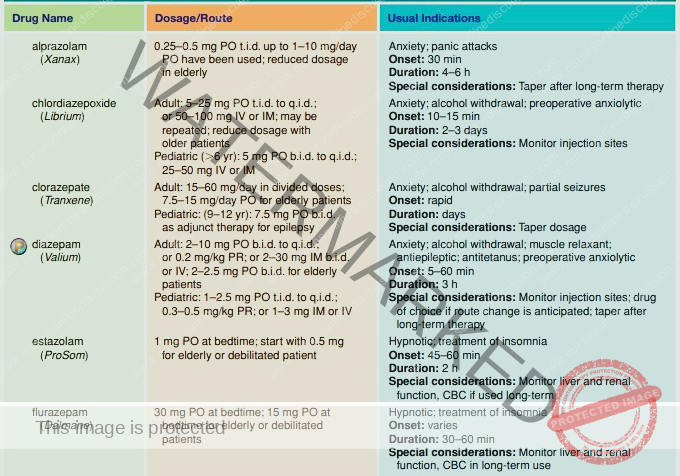
Indications of Benzodiazepines used as Anxiolytics
Benzodiazepines are prescribed for the management of various conditions, including:
Anxiety Disorders: Effective in treating different forms of anxiety disorders, such as:
Generalized Anxiety Disorder (GAD)
Social Anxiety Disorder
Panic Disorder
Alcohol Withdrawal: Used to manage symptoms associated with alcohol withdrawal.
Hyperexcitability and Agitation: Helps to reduce states of excessive excitability and agitation.
Obsessive-Compulsive Disorder (OCD): May be used as part of a treatment plan for OCD.
Preoperative Anxiety Relief: Administered before surgery to alleviate anxiety and tension, contributing to balanced anesthesia.
Pharmacodynamics
These medications exert their effects within the limbic system and the Reticular Activating System (RAS). They enhance the action of gamma-aminobutyric acid (GABA), a key inhibitory neurotransmitter in the brain. By increasing GABA’s effectiveness, benzodiazepines interfere with neuronal firing.
GABA functions to stabilize the postsynaptic neuron. This stabilization results in an anxiolytic effect at doses lower than those needed to induce significant sedation or hypnosis.
Note: The precise mechanism of action is not yet fully elucidated and is an area of ongoing research.
Mechanism of Action
Anxiolytics, specifically benzodiazepines, boost the activity of gamma-aminobutyric acid (GABA) and depress the Central Nervous System (CNS). This CNS depression impacts the limbic system, which is crucial for integrating emotional responses and regulating emotions. GABA’s enhanced activity leads to:
Relaxation of skeletal muscles.
Anticonvulsant effects.
Calming of emotional responses.
Benzodiazepines induce Central Nervous System (CNS) depression by potentiating GABA. GABA reduces neuronal excitability throughout the brain, leading to a calming effect.
Pharmacokinetics
Benzodiazepines are generally well absorbed after oral administration from the gastrointestinal (GI) tract. Peak plasma concentrations are typically reached within 30 minutes to 2 hours.
They are highly lipid-soluble, allowing for good distribution throughout the body. They readily cross the placenta and are also present in breast milk.
Metabolic processing of benzodiazepines occurs extensively in the liver. For patients with compromised liver function, dosage adjustments (typically lower doses) are necessary, and close monitoring is crucial.
Excretion of benzodiazepines and their metabolites is primarily renal, via the urine.
Contraindications and Cautions
Allergy: Known hypersensitivity to any benzodiazepine medication is a contraindication.
Psychosis: Benzodiazepines are contraindicated in psychosis, as sedation may worsen psychotic symptoms.
Ocular Conditions: Avoid in acute narrow-angle glaucoma due to potential exacerbation.
CNS Depression: Contraindicated in conditions of significant CNS depression, such as shock, coma, or acute alcohol intoxication, as benzodiazepines can further depress CNS function.
Pregnancy: Benzodiazepines are contraindicated during pregnancy, particularly in the first trimester, due to an association with a potential pattern of congenital malformations including cleft lip or palate, inguinal hernia, cardiac defects, microcephaly, or pyloric stenosis. Neonatal withdrawal syndrome is also a risk.
Lactation: Breastfeeding is not recommended due to the potential for adverse effects in the neonate, such as sedation.
Elderly or Debilitated Patients: Use with caution due to increased risk of unpredictable reactions.
Renal or Hepatic Dysfunction: Use with caution in patients with kidney or liver problems. These conditions can impair drug metabolism and excretion, potentially leading to toxicity. Dose adjustments are usually required.
Adverse Effects and Side Effects
Adverse effects of benzodiazepines are primarily related to their CNS and peripheral nervous system actions:
Nervous System Effects:
Sedation
Drowsiness
Depression
Lethargy
Blurred vision
Headache
Apathy
Light-headedness
Confusion
Gastrointestinal (GI) Effects:
Dry mouth
Constipation
Nausea
Vomiting
Elevated liver enzymes
Cardiovascular Effects:
Hypotension
Hypertension
Arrhythmias
Palpitations
Respiratory difficulties
Hematological Effects:
Blood dyscrasias (rare)
Anemia (rare)
Genitourinary (GU) Effects:
Urinary retention and hesitancy
Loss of libido
Changes in sexual function
Note: Abruptly stopping benzodiazepine medication, especially after prolonged use, can trigger a withdrawal syndrome. Symptoms may include nausea, headache, vertigo, malaise, and nightmares.
Drug Interactions
CNS Depressants: Concurrent use with alcohol or other CNS depressants increases the risk of additive CNS depression. This combination should generally be avoided.
Increased Benzodiazepine Effects: The effects of benzodiazepines may be enhanced when taken with cimetidine, oral contraceptives, or disulfiram.
Decreased Benzodiazepine Effects: The effectiveness of benzodiazepines may be reduced when administered with theophyllines or ranitidine.
Remember: Flumazenil is the specific antidote used to reverse benzodiazepine overdose.
Special Nursing Considerations when using Benzodiazepines as Anxiolytics
Intra-arterial Administration: Avoid intra-arterial administration as it can lead to severe arteriospasm and gangrene. Closely monitor IV sites for any signs of local reactions and promptly address them.
IV Drug Mixing: Do not mix IV benzodiazepines with other medications in solution due to potential drug interactions.
Parenteral vs. Oral Administration: Use parenteral (e.g., IV, IM) forms only when oral administration is not feasible. Transition to oral formulations, which are generally safer and have fewer adverse effects, as soon as possible.
IV Administration Rate: Administer IV benzodiazepines slowly. Rapid IV administration has been linked to hypotension, bradycardia, and cardiac arrest.
Narcotic Analgesic Dosage Adjustment: When co-administering with narcotic analgesics, consider reducing the narcotic dose to minimize additive sedative effects and potential potentiation.
Post-Parenteral Administration Monitoring: Patients receiving parenteral benzodiazepines should remain recumbent in bed for at least 3 hours post-administration. Advise ambulatory patients against operating motor vehicles after injection to ensure safety.
Long-Term Therapy Monitoring: For patients on long-term benzodiazepine therapy, regularly monitor hepatic and renal function and complete blood count (CBC) to detect any dysfunction. If dysfunction is identified, arrange to gradually taper and discontinue the drug.
Gradual Dose Tapering: After prolonged therapy, especially in patients with epilepsy, gradually taper the benzodiazepine dose. Abrupt withdrawal can precipitate seizures in epileptic patients and may also cause a general withdrawal syndrome.
Comfort Measures: Implement comfort measures to help patients manage drug effects. These may include advising patients to void before dosing, establishing a bowel management plan if needed, administering the drug with food if GI upset is significant, managing the environment (light, temperature, noise), implementing safety precautions (side rails, assistance with ambulation), and providing orientation support.
Patient Education: Provide comprehensive patient education. Include the drug name, prescribed dosage, methods to minimize adverse effects, warning signs indicating potential problems, and the necessity for regular monitoring and evaluation. This education is crucial for improving patient understanding of their medication and promoting adherence.
Psychological Support: Offer emotional support and encouragement to assist patients in coping with their diagnosis and medication regimen.
Flumazenil Availability: Ensure availability of flumazenil, the benzodiazepine antidote, for managing potential overdose situations.
BARBITURATES USED AS ANXIOLYTIC-HYPNOTICS
Barbiturates historically served as the primary class of medications for sedation and sleep induction. However, in contemporary practice, they are less favored as anxiolytic-hypnotics.
This shift is largely due to several factors:
Increased Side Effect Profile: Barbiturates are associated with a higher incidence of sedation and other undesirable adverse effects compared to more recently developed sedative-hypnotic agents.
Risk of Dependence and Addiction: The potential for both physical dependence and addiction is significantly greater with barbiturates than with many newer alternatives.
Consequently, due to these safety and tolerability concerns, modern anxiolytic and hypnotic therapy has largely transitioned away from barbiturates, favoring newer drug classes with improved profiles.
Dose
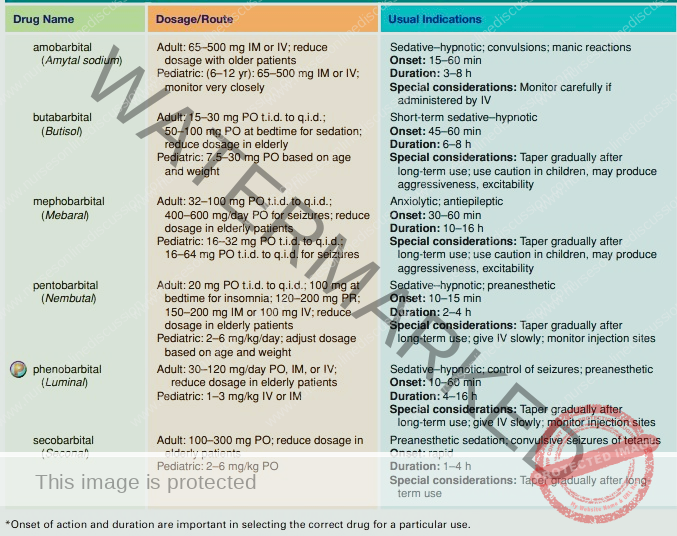
Indications
Barbiturates may be considered for:
Alleviating signs and symptoms of anxiety.
Inducing sedation, including pre-anesthetic sedation.
Managing sleep disorders such as insomnia.
Treatment of seizure disorders.
Pharmacodynamics
Barbiturates function as general depressants of the central nervous system (CNS). They exert their effects by:
Inhibiting neuronal impulse conduction within the ascending Reticular Activating System (RAS).
Depressing the cerebral cortex.
Altering cerebellar function.
Reducing motor nerve output.
Through these actions, barbiturates can induce a spectrum of CNS depression ranging from sedation and hypnosis to anesthesia and, in severe cases, coma.
Pharmacokinetics
Absorption: Barbiturates are generally well absorbed following administration, typically reaching peak plasma concentrations within 20 to 60 minutes.
Metabolism: They undergo hepatic metabolism in the liver.
Excretion: Barbiturates are eliminated from the body primarily through urinary excretion.
Longer-acting Barbiturates: These tend to be metabolized more slowly and are excreted to a greater extent in their unchanged form in the urine.
Contraindications
Barbiturates are contraindicated in the following situations:
Known allergy or hypersensitivity to any barbiturate medication.
History of addiction or dependence, particularly to other sedative-hypnotic drugs, due to the heightened addictive potential of barbiturates.
Porphyria, a group of genetic disorders, as barbiturates can exacerbate this condition.
Hepatic impairment or nephritis (kidney inflammation), as these conditions can compromise drug metabolism and excretion, increasing the risk of toxicity.
Respiratory distress or severe respiratory dysfunction, which can be worsened by the CNS-depressant effects of barbiturates.
Pregnancy, due to the potential for adverse effects on the fetus. Congenital abnormalities have been associated with barbiturate use during pregnancy.
Adverse Effects
Barbiturates are associated with a range of adverse effects that are generally more pronounced and serious compared to newer hypnotic agents. This less favorable side effect profile contributes to their diminished role in routine anxiety treatment.
Central Nervous System (CNS) Effects:
Drowsiness, somnolence, and lethargy.
Ataxia (loss of coordination) and vertigo (dizziness).
“Hangover” feeling upon awakening.
Thinking abnormalities and confusion.
Paradoxical excitement or agitation.
Anxiety and hallucinations.
Gastrointestinal (GI) Effects:
Nausea and vomiting.
Constipation or diarrhea.
Epigastric pain.
Cardiovascular System (CVS) Effects:
Bradycardia (slow heart rate).
Hypotension, particularly with intravenous (IV) administration.
Syncope (fainting).
Respiratory Effects:
Serious hypoventilation (reduced breathing rate and depth).
Respiratory depression and laryngospasm, especially with IV administration.
Hypersensitivity Reactions:
Skin rash.
Serum sickness.
Stevens-Johnson syndrome, a severe and potentially fatal skin reaction.
Drug Interactions
Barbiturates can interact with a variety of other drugs, potentially altering their effects or increasing the risk of adverse events.
Increased CNS Depression: Concurrent use with other CNS depressants, including alcohol, antihistamines, and other tranquilizers, can lead to additive CNS depression. Dose adjustments may be necessary if these combinations are unavoidable.
Altered Phenytoin Response: Barbiturates can alter the response to phenytoin, an anticonvulsant medication.
Increased Effects with MAOIs: Combining barbiturates with monoamine oxidase inhibitors (MAOIs) may lead to increased serum levels and enhanced effects of barbiturates.
Reduced Effectiveness of Other Drugs: Barbiturates, through enzyme induction in the liver, can reduce the effectiveness of numerous medications, including:
Oral anticoagulants.
Digoxin.
Tricyclic antidepressants (TCAs).
Corticosteroids.
Oral contraceptives and estrogens.
Acetaminophen.
Metronidazole.
Phenmetrazine.
Carbamazepine.
Beta-blockers.
Griseofulvin.
Phenylbutazones.
Theophyllines.
Quinidine.
Doxycycline.
Special Nursing Considerations when using Barbiturates as Anxiolytic-Hypnotics
Avoid Intra-arterial Administration: Do not administer barbiturates intra-arterially due to the risk of serious arteriospasm and gangrene. Carefully monitor injection sites for local reactions.
Do Not Mix IV Drugs: Avoid mixing IV barbiturates with other drugs in solution to prevent potential drug interactions.
Use Parenteral Forms Judiciously: Reserve parenteral forms for situations where oral administration is not feasible. Transition to oral forms as soon as possible to minimize the risk of serious reactions.
Administer IV Medications Slowly: Inject IV medications slowly, as rapid administration can lead to cardiac complications.
Prepare for Life Support: Ensure standby life-support facilities are available in case of severe respiratory depression or hypersensitivity reactions.
Taper Dosage Gradually: After long-term therapy, especially in patients with epilepsy, gradually taper the dose to prevent seizures or withdrawal syndrome.
Implement Comfort Measures: Provide comfort measures to help patients tolerate drug effects. This includes:
Small, frequent meals.
Easy access to bathroom facilities.
A bowel management program as needed.
Administering medication with food if GI upset is significant.
Environmental control (lighting, temperature, stimulation).
Safety precautions (side rails, assistance with ambulation).
Orientation support and appropriate skin care as needed.
Provide Thorough Patient Education: Educate patients comprehensively about:
Drug name and prescribed dosage.
Measures to avoid adverse effects.
Warning signs that may indicate potential problems.
Emphasize Periodic Monitoring: Instruct patients about the necessity of periodic monitoring and evaluation to enhance their understanding of drug therapy and promote compliance.
Offer Support and Encouragement: Provide emotional support and encouragement to help patients cope with their diagnosis and medication regimen.
OTHER ANXIOLYTIC AND HYPNOTIC DRUGS
Besides benzodiazepines and barbiturates, other pharmacological agents are utilized for managing anxiety or inducing hypnosis. These drugs do not belong to either the benzodiazepine or barbiturate classes.
Antihistamines: Certain antihistamines, such as promethazine (Phenergan) and diphenhydramine (Benadryl), possess significant sedative properties in some individuals. They are used in the perioperative setting as preoperative medications and postoperatively to reduce the need for opioid analgesics.
Buspirone (BuSpar): Buspirone is a newer anxiolytic agent with a distinct pharmacological profile. It lacks sedative, anticonvulsant, and muscle relaxant properties typically associated with benzodiazepines. Its precise mechanism of action remains incompletely understood. However, buspirone effectively reduces anxiety symptoms with a reduced incidence of CNS effects and severe adverse reactions compared to many other anxiolytic medications. It is rapidly absorbed following oral administration, undergoes hepatic metabolism, and is excreted in the urine.
Zaleplon (Sonata) and Zolpidem (Ambien): Both zaleplon and zolpidem are medications specifically indicated for the short-term management of insomnia due to their sedative effects. Their mechanism is thought to involve modulation of serotonin levels within sleep centers located near the Reticular Activating System (RAS). These drugs are metabolized in the liver and eliminated via urinary excretion.
other indications

Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

