Drugs Used in the Reproductive System
Subtopic:
Benign Prostatic Hyperplasia (BPH)
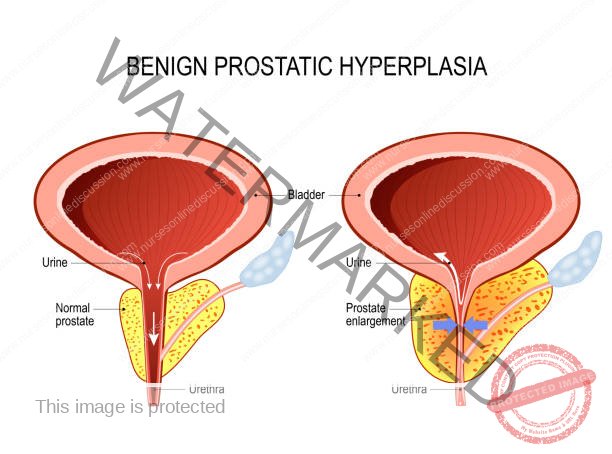
Benign Prostatic Hyperplasia (BPH) is a condition characterized by the enlargement, or hypertrophy, of the prostate gland.
BPH is a prevalent condition, particularly affecting older men, commonly those over the age of 60.
Common Causes of BPH and Pathophysiology
The development and progression of BPH are influenced by two primary categories of factors:
Anatomical Factors: These relate to the physical structure of the prostate gland.
Enlargement of the prostate gland itself creates a physical obstruction.
This enlargement compresses the bladder neck, impeding the free flow of urine.
The prostate gland becomes more sensitive and responsive to hormonal influences, specifically androgens and estrogens.
Dynamic Factors: These arise from the physiological function of the prostate and surrounding structures.
Excessive stimulation of the sympathetic nervous system plays a role.
This stimulation acts via alpha-1 adrenergic receptors located in the prostate gland.
Increased sympathetic tone leads to heightened constriction (tone) of the urinary bladder sphincter and the smooth muscle within the prostate itself.
The Pathophysiology of BPH is as follows:
The development of BPH involves a complex interplay of factors ultimately leading to urinary symptoms:
Resistance: BPH arises from the intricate interaction of resistance within the prostatic urethra. This resistance is due to both:
Mechanical Effects: Physical obstruction caused by the enlarged prostate tissue.
Spastic Effects: Increased smooth muscle tone contributing to urethral narrowing.
Obstruction: The enlarged (hypertrophied) lobes of the prostate gland can directly compress or obstruct critical areas:
Bladder Neck: The outlet of the bladder.
Urethra: Specifically, the prostatic urethra, the portion passing through the prostate.
This obstruction impairs bladder emptying, leading to:Incomplete Bladder Emptying: The bladder is unable to fully expel urine.
Urinary Retention: Urine remains in the bladder after voiding.
Dilation: Over time, the chronic obstruction can lead to structural changes in the upper urinary tract:
Gradual Dilation of the Ureters: The tubes carrying urine from the kidneys to the bladder can widen.
Gradual Dilation of the Kidneys: The renal collecting systems within the kidneys can also become distended due to back pressure.
Resulting Symptoms of BPH
BPH produces a range of characteristic urinary symptoms:
Urinary Frequency: An early indicator of BPH is often an increased need to urinate more often than usual. This involves:
Frequent trips to the bathroom to void.
Urinary Urgency: A sudden, compelling, and immediate need to urinate that is difficult to postpone.
Nocturia: The need to wake up and urinate frequently during the night.
Weak Urinary Stream: The force and continuity of the urinary stream are diminished. This is characterized by:
Decreased force of the urine stream.
Intermittent stream with stops and starts.
Dribbling Urine: Involuntary leakage of urine, specifically:
Urine dribbles or leaks out involuntarily after completing urination.
Straining: Difficulty initiating urination and maintaining a consistent stream, often requiring:
Abdominal straining or pushing to begin urination.
Urinary Retention: Inability to fully empty the bladder.
Decrease in Force of Urinary Output: Reduced power and pressure of the urine stream.
Intermittency During Urination: The urinary stream is not continuous, with interruptions and starts and stops during voiding.
Investigations and Diagnosis of BPH
The diagnosis of BPH typically involves several components:
Digital Rectal Examination (DRE)
A DRE is a key initial step in evaluating the prostate gland.
During a DRE, the physician can often assess the prostate and identify characteristic features of BPH, such as:
Enlarged Prostate: The gland feels larger than normal.
Rubbery Consistency: The prostate has a smooth, elastic texture.
Nontender Prostate: The gland is not painful to the touch, helping to differentiate BPH from prostatitis (prostate inflammation).

Urinalysis
A routine urinalysis is essential to:
Screen for hematuria (blood in the urine), which can indicate underlying conditions.
Screen for urinary tract infection (UTI), a common complication of BPH.
Urinalysis Findings in BPH/UTI:
Color: May vary from normal yellow to abnormal shades:
Dark brown or dark urine.
Bright red or dark red, indicating bloody urine.
Appearance: Urine may appear cloudy instead of clear.
pH: A pH of 7 or higher can suggest the presence of a UTI.
Microscopic Examination: Microscopic analysis may reveal:
Bacteria: Indicating infection.
White blood cells (WBCs): Elevated levels suggest inflammation or infection.
Red blood cells (RBCs): Presence of blood in the urine (hematuria).
Urine Culture
A urine culture may be performed to identify specific bacterial pathogens in cases of suspected UTI.
Common Bacterial Pathogens in UTI:
Staphylococcus aureus
Proteus species
Klebsiella species
Pseudomonas species
Escherichia coli
Urine Cytology
Urine cytology is a test to examine urine sediment for abnormal cells.
Purpose: To rule out bladder cancer as a cause of urinary symptoms.
Blood Urea Nitrogen (BUN) and Creatinine (Cr)
BUN and creatinine are blood tests that assess kidney function.
Elevated BUN/Cr levels suggest:
Compromised Renal Function: Kidney function may be impaired due to back pressure from urinary obstruction.
Prostate-Specific Antigen (PSA)
PSA is a glycoprotein produced by prostatic epithelial cells. It is normally present in the blood of adult men.
PSA Level Testing is Recommended:
For men with a life expectancy of at least 10 years.
When the knowledge of prostate cancer presence would alter management decisions (e.g., watchful waiting vs. active treatment).
PSA Levels in BPH and Prostate Cancer:
Elevated PSA in Prostate Cancer: Significantly elevated PSA levels are strongly associated with prostate cancer.
Elevated PSA in BPH: PSA levels can also be moderately elevated in BPH due to prostate enlargement, but typically not to the same extent as in cancer.
Free PSA Percentage: Research suggests that:
Elevated PSA with Low Percentage of Free PSA: More likely indicative of prostate cancer.
Elevated PSA with Higher Percentage of Free PSA: More likely associated with benign conditions like BPH.
White Blood Cell Count (WBC)
A Complete Blood Count (CBC) may include a WBC count.
Elevated WBC Count (Leukocytosis):
A WBC count above 11,000/mm³ may suggest infection, provided the patient is not immunocompromised.
Uroflowmetry
Uroflowmetry is a non-invasive test that measures the rate and pattern of urine flow during voiding.
Purpose: Assesses the degree of bladder outlet obstruction. Reduced maximum flow rate and prolonged voiding time are typical findings in BPH.
Intravenous Pyelogram (IVP) with Post-Voiding Film
IVP is an X-ray study of the urinary tract using contrast dye. A post-voiding film is taken after urination.
IVP Findings in BPH:
Delayed Bladder Emptying: Contrast dye remains in the bladder after voiding.
Varying Degrees of Urinary Tract Obstruction: Indicates the level and location of blockage.
Prostatic Enlargement: Visualizes the enlarged prostate gland.
Bladder Diverticula: Outpouchings of the bladder wall due to chronic obstruction.
Abnormal Thickening of Bladder Muscle (Trabeculation): Result of the bladder working harder to overcome obstruction.
Voiding Cystourethrography (VCUG)
VCUG is an X-ray study of the bladder and urethra during voiding, using contrast dye instilled into the bladder.
VCUG vs. IVP: VCUG may be used as an alternative to IVP to visualize the bladder and urethra, often using local dyes rather than intravenous contrast.
Cystometrogram
Cystometrogram is a urodynamic test that measures pressure and volume changes in the bladder during filling and voiding.
Purpose: Identifies bladder dysfunction unrelated to BPH. Helps distinguish BPH-related symptoms from other bladder issues like overactive bladder.
Cystourethroscopy
Cystourethroscopy is a procedure using a thin, lighted scope (cystoscope) inserted into the urethra to visualize the bladder and urethra directly.
Purpose:
View Degree of Prostatic Enlargement: Directly visualizes the size and shape of the prostate gland.
Assess Bladder Wall Changes: Detects bladder wall abnormalities like bladder diverticula and trabeculation.
Cystometry
Cystometry is another urodynamic test that specifically focuses on bladder muscle function.
Purpose: Evaluates detrusor muscle function and tone. Detrusor muscle is the bladder’s main muscle responsible for contraction during urination.
Transrectal Prostatic Ultrasound (TRUS)
TRUS is an imaging technique using ultrasound waves via a probe inserted into the rectum to visualize the prostate.
TRUS Applications in BPH:
Measures Prostate Size: Accurately determines the volume of the prostate gland.
Measures Residual Urine: Quantifies the amount of urine remaining in the bladder after voiding (post-void residual).
Locates Lesions Unrelated to BPH: Can help identify other prostate abnormalities, including suspicious lesions that may warrant biopsy to rule out prostate cancer.
Classification of Drugs for BPH
Medications for BPH are primarily classified into three major categories:
5-Alpha Reductase Inhibitors
Alpha-1 Selective Blockers
Combined Therapies (using both 5-alpha reductase inhibitors and alpha-1 blockers)
1. 5-Alpha Reductase Inhibitors
Mechanism of Action: These drugs work by inhibiting the enzyme 5-alpha reductase.
5-alpha reductase is responsible for converting testosterone into dihydrotestosterone (DHT) within the prostate gland.
DHT is a potent androgen that stimulates prostate growth.
By blocking 5-alpha reductase, these drugs reduce DHT production in the prostate, thereby suppressing androgen activity in the prostate gland.
Overall Effect: Leads to decreased growth of the prostate gland and, in some cases, shrinkage of the enlarged prostate.
Important Note: The therapeutic effects of 5-alpha reductase inhibitors are not immediate. They do not provide rapid relief of urinary retention or acute symptoms. It may take several months of treatment to see noticeable symptom improvement.
Examples and Dosing:
Finasteride: 5mg orally once daily (o.d.).
Dutasteride: 0.5mg orally once daily (o.d.).
Both medications are administered orally in tablet form.
2. Alpha-1 Selective Blockers
Mechanism of Action: Alpha-1 selective blockers target and block alpha-1 adrenergic receptors.
These receptors are located in the smooth muscle of the prostate gland and bladder neck.
Blocking alpha-1 receptors causes relaxation of smooth muscle in these areas.
Result: Relaxation of the bladder neck and prostate sphincter muscles leads to improved urine flow and reduced bladder outlet obstruction.
Subcategories based on Duration of Action:
Short-Acting Alpha-1 Blockers: Provide shorter duration of symptom relief, may require more frequent dosing.
Examples: Prazosin, Indoramin, Alfuzosin.
Long-Acting Alpha-1 Blockers: Offer longer-lasting symptom control, typically administered once daily.
Examples: Tamsulosin, Doxazosin, Terazosin.
Dosing Examples:
Prazosin: Initial dose 0.5-1mg orally once daily (o.d.) at bedtime. Dosage gradually increased after a few days to a maintenance dose of 1mg twice daily (b.d.) for 3 days per week (3/7). Note: Prazosin is less commonly used for BPH due to its non-selective alpha-blocking effects and potential for blood pressure effects.
Terazosin: Initial dose 1mg orally once daily, titrated up to a typical maintenance range of 2-10mg once daily (o.d.).
Doxazosin: Initial dose 1mg orally once daily (o.d.), with gradual titration to maintenance doses as needed.
Tamsulosin: 0.4mg orally once daily (o.d.) administered with meals. Note: Tamsulosin is highly selective for alpha-1A receptors in the prostate and bladder neck, leading to fewer cardiovascular side effects compared to less selective alpha-blockers.
Key Notes on Alpha-1 Blockers:
Tamsulosin’s Selectivity: Tamsulosin is often preferred as a long-acting alpha-1 blocker for BPH because of its high selectivity for alpha-1A receptors in the prostate. This selectivity minimizes effects on blood pressure compared to less selective agents.
Prazosin’s Dosing and Hypotension: Prazosin, being less selective, can cause postural hypotension (orthostatic hypotension). Starting with a low dose at bedtime and gradually increasing it helps mitigate this risk.
Faster Onset of Action: Alpha-1 blockers generally provide more rapid symptom relief compared to 5-alpha reductase inhibitors. They are often used in combination with finasteride or dutasteride for comprehensive BPH management.
Adverse Effects of Alpha-1 Blockers (Class-Related):
Postural Hypotension (Orthostatic Hypotension): Dizziness or lightheadedness upon standing due to blood pressure drop.
Reflex Tachycardia: Compensatory increase in heart rate in response to blood pressure lowering.
Less Commonly Used Alpha-Blockers:
Phentolamine and phenoxybenzamine are less frequently used alpha-blockers in BPH management due to their non-selectivity and side effect profiles.
Medical Management of BPH
The primary goals of medical management for BPH are to:
Improve Quality of Life: Alleviate bothersome urinary symptoms and improve patient well-being.
Treatment Strategy Tailoring: The specific treatment approach depends on the severity of the patient’s symptoms, overall health, and individual preferences.
Emergency Management – Acute Urinary Retention
Catheterization: In emergency situations where a patient presents with acute urinary retention (inability to void), immediate catheterization is performed to drain the bladder and provide relief.
Cystostomy: In rare cases, when urethral catheterization is not possible or appropriate, a suprapubic cystostomy (surgical incision into the bladder to insert a drainage tube) may be necessary to establish urinary drainage.
Pharmacologic Management – Medications
Medications are a mainstay of BPH management and aim to reduce symptoms and improve urinary function.
Alpha-Adrenergic Blockers: These are first-line medications for symptomatic BPH.
Examples: Alfuzosin, terazosin, doxazosin, tamsulosin, silodosin.
Mechanism: Relax smooth muscle in the bladder neck and prostate, improving urine flow.
5-Alpha Reductase Inhibitors: Used for men with significantly enlarged prostates.
Example: Finasteride, dutasteride.
Mechanism: Reduce prostate size by blocking DHT production.
Combination Therapy: For men with moderate to severe symptoms, combination therapy using both an alpha-blocker and a 5-alpha reductase inhibitor may be more effective than monotherapy.
Hormonal Manipulation (Antiandrogens): 5-alpha reductase inhibitors like finasteride are antiandrogen agents.
Mechanism: Decrease prostate size by preventing testosterone conversion to DHT.
Phytotherapeutic Agents and Dietary Supplements
Herbal Remedies: While widely used by some men, the use of phytotherapeutic agents and dietary supplements for BPH is generally not recommended by medical guidelines due to a lack of robust scientific evidence of efficacy and inconsistent product quality.
Common examples: Serenoa repens (saw palmetto berry) and Pygeum africanum (African plum).
Saw Palmetto: Despite limited evidence of overall effectiveness, saw palmetto remains a popular herbal remedy for BPH symptoms. Some studies suggest modest symptom improvement in some men, but larger, well-designed trials are needed to confirm benefits.

Surgical Management
When medical management is insufficient or not appropriate, surgical or minimally invasive procedures are considered for BPH treatment. These interventions range from heat-based therapies to prostate resection.
Transurethral Microwave Thermotherapy (TUMT). This procedure utilizes microwave energy to generate heat within the prostate gland. The targeted heat application is designed to reduce excess prostatic tissue.
Transurethral Needle Ablation (TUNA). TUNA employs radiofrequency energy. Thin needles are inserted into the prostate gland to deliver low-level radio frequencies. This targeted energy application creates localized heat, intentionally destroying problematic prostate tissue while aiming to minimize damage to surrounding healthy tissues.
Transurethral Resection of the Prostate (TURP). TURP is a surgical procedure where an endoscope is inserted through the urethra to access the prostate gland. The inner portion of the prostate, which is typically the source of obstruction in BPH, is then surgically removed using specialized instruments passed through the endoscope.
Open Prostatectomy. This is a more invasive surgical approach typically reserved for cases where the prostate gland is significantly enlarged. Open prostatectomy involves a surgical incision in the lower abdomen (suprapubic or retropubic approach) or perineum (perineal approach) to directly access and remove the inner, obstructing part of the prostate gland.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

