Psychiatric Emergencies
Subtopic:
Status epilepticus
Status epilepticus (SE) is a serious neurological emergency defined by either:
A single seizure lasting longer than 30 minutes.
Recurrent seizures occurring for 30 minutes or more without full recovery of consciousness between episodes.
A more contemporary and clinically relevant definition considers status epilepticus to be:
A generalized convulsive seizure lasting 5 minutes or longer, OR
Two or more sequential seizures without full recovery of consciousness between them.
This condition is not a specific type of epilepsy but rather a severe complication of epilepsy, particularly grand mal epilepsy. It is considered both a medical and psychiatric emergency due to its life-threatening nature. Prompt and rapid initiation of treatment is crucial.
Diagnosis of Status Epilepticus
Diagnosis involves a multifaceted approach:
Observation of Seizure Activity: Direct observation of a seizure exhibiting characteristics such as:
Elevated body temperature (hyperthermia).
Increased heart rate (tachycardia).
Heightened brain metabolic demand.
Patient History: Obtaining a detailed patient history, including prior seizure events.
Neurological Examination: A comprehensive neurological assessment to evaluate:
Reflexes and neurological function.
Electroencephalogram (EEG): An EEG may be performed to:
Detect epileptiform activity in the brain, confirming seizure activity.
Computed Tomography (CT) Scan of the Brain: A CT scan may be used to:
Visualize brain structure and function.
Identify any underlying structural abnormalities.
Skull X-ray: Skull X-rays may be utilized to:
Detect evidence of skull lesions or trauma.
Additional Laboratory Tests: A range of laboratory tests may be conducted to identify potential underlying causes or metabolic disturbances:
Random Blood Glucose Level: To rule out hypoglycemia (low blood sugar).
Blood Slide for Malaria: To exclude malaria as a cause of seizures, especially in endemic areas.
Urinalysis: To assess for urinary abnormalities.
Renal and Liver Function Tests: To evaluate kidney and liver function.
Electrolyte Levels: To check for electrolyte imbalances (e.g., sodium, potassium).
Calcium and Magnesium Levels: To assess levels of these minerals, which are important for neurological function.
Common Triggers of Epileptic Seizures
Various factors can trigger seizures in individuals with epilepsy:
Fever: Elevated body temperature, especially in childhood.
Sleep Deprivation: Seizures may occur during sleep or shortly after waking.
Fasting: Prolonged periods without food intake.
Emotional Stress: Strong emotions such as fear, anger, or excitement.
Sensory Stimuli: Flickering lights or patterns.
Substance Use:
Alcohol intoxication.
Alcohol withdrawal.
Lifestyle Factors:
Fatigue and exhaustion.
Boredom and lack of stimulation.
Environmental Factors: High altitude.
Medication Non-adherence: Discontinuation of prescribed anticonvulsant medications.
Dehydration: Insufficient fluid intake.
Infections: Systemic infections.
Associated Injuries: Assess for injuries sustained during the seizure event.
Treatment and Management of Status Epilepticus
Due to the sudden and unpredictable nature of seizures, preparedness is crucial. Status epilepticus requires immediate and decisive action.
Aims of Management
The primary goals of managing status epilepticus are:
Prevent Patient Injury: Protect the patient from harm during the seizure.
Prevent Complications: Minimize the risk of serious complications associated with prolonged seizure activity.
Emergency Management (First Aid – Out of Hospital)
When assisting someone experiencing a seizure outside of a hospital setting:
Remain Calm: Maintain composure and speak in a calm, reassuring manner.
Ensure Safety:
Remove the person from immediate danger if possible.
If the environment is safe, do not attempt to move the person unnecessarily.
Time the Seizure: Note the starting time of the seizure. If it persists beyond 5 minutes, immediately call for emergency medical services (ambulance).
Protect the Airway: Loosen any restrictive clothing around the neck, such as ties or necklaces.
Head Protection: Support the head by placing a soft, flat object like a folded jacket underneath to cushion it and prevent head injury from jerking movements.
Clear the Area: Create a safe space around the person and minimize crowding to ensure access to fresh air.
Post-Seizure Positioning: Once the seizure subsides:
Gently turn the person onto their side (lateral recovery position) to prevent airway obstruction from saliva or vomit.
Ensure their breathing is returning to a normal pattern. If breathing is labored or shallow, call for emergency medical assistance.
Check the airway gently to ensure no obstructions, such as dentures, are present.
Stay with the Person: Remain with the person until they are fully awake and alert.
Reorientation and Reassurance: Upon regaining consciousness, reorient the person to their surroundings and offer reassurance, especially if they are embarrassed or confused.
Actions to Avoid During a Seizure (First Aid)
Do Not Insert Objects into the Mouth: Avoid placing any hard objects, like spoons, into the mouth. This can cause injury to teeth, gums, or jaw.
Do Not Restrain Limbs: Do not forcibly hold down or restrain the person’s limbs. This can cause injury and does not stop the seizure.
Do Not Offer Food or Drink: Do not give anything to eat or drink until the person is fully alert and able to swallow safely.
Do Not Perform Mouth-to-Mouth Resuscitation: Avoid attempting mouth-to-mouth breaths unless breathing is absent after the seizure has ceased and spontaneous breathing does not resume. People usually resume breathing on their own after a seizure.
Emergency Management (In-Hospital Setting)
In a hospital emergency setting, the management of status epilepticus involves:
Oxygen Administration: Provide supplemental oxygen to support respiratory function.
Hypoglycemia Management: If hypoglycemia is suspected, administer an intravenous bolus of 50ml of 50% glucose.
Thiamine Administration: If alcohol abuse is suspected as a contributing factor, consider administering parenteral thiamine to prevent Wernicke’s encephalopathy.
Anticonvulsant Medications (First-Line): Administer rapid-acting anticonvulsant medications intravenously as initial therapy:
Diazepam IV
Lorazepam IV
Clonazepam IV
Midazolam IV
Diazepam Administration Protocol:
Initial dose: 5-10mg Diazepam IV, administered slowly.
Repeat dose: May be repeated after 10-20 minutes if seizure persists.
Maximum dose: Do not exceed a total dose of 30mg Diazepam within an 8-hour period.
Pediatric dosage: For children, administer 0.05-0.3 mg/kg per dose intravenously over 2-3 minutes. Do not exceed a total dose of 10mg.
Referral: If seizures do not improve after initial Diazepam administration, immediate referral to specialized care is necessary.
Phenytoin Administration (Second-Line): If seizures recur or do not respond to Diazepam after 30 minutes, consider intravenous Phenytoin.
Phenytoin Infusion Protocol:
Intravenous infusion: Administer Phenytoin by intravenous infusion at a loading dose of 15mg/kg body weight.
Infusion rate: Infuse at a rate not exceeding 50mg per minute to avoid adverse cardiovascular effects.
Monitoring: Continuous monitoring of blood pressure and ECG (electrocardiogram) is essential during Phenytoin infusion.
Dilution: Phenytoin should be diluted with sodium chloride (normal saline) at a concentration of 1mg of Phenytoin per 1ml of normal saline.
Supportive Care and Seizure Termination: Provide comprehensive supportive care concurrently with anticonvulsant therapy, focusing on:
Prompt termination of electrical seizure activity.
Individualized patient care based on needs.
ABC Resuscitation: Prioritize basic life support measures, including:
Airway management
Breathing support
Circulation maintenance (ABCs).
Establish Etiology: Investigate and determine the underlying cause of status epilepticus. In older adults, stroke is a common underlying etiology. Status epilepticus in elderly patients carries a high mortality risk.
Manage Medical Complications: Identify and aggressively treat potential medical complications that may arise from prolonged seizure activity.
Monitoring During Status Epilepticus Management
Continuous and vigilant monitoring is crucial:
Neurological Observations: Regular neurological assessments, including monitoring of:
Level of consciousness
Pupillary response
Vital Signs: Frequent measurements of:
Pulse rate
Blood pressure
Body temperature
Advanced Monitoring:
ECG (Electrocardiogram): Continuous cardiac monitoring.
Arterial Blood Gases (ABGs): Regular blood gas analysis to assess oxygenation and acid-base balance.
Coagulation Studies: Monitoring of clotting parameters.
Complete Blood Count (CBC): Blood cell counts.
Anticonvulsant Drug Levels: Therapeutic drug monitoring to ensure adequate drug levels.
EEG Monitoring: Continuous EEG monitoring is essential for:
Refractory Status Epilepticus: Patients whose seizures are not responding to initial treatments.
Non-Epileptic Status Consideration: To rule out non-epileptic conditions that may mimic status epilepticus.
Prognosis of Status Epilepticus
The prognosis of status epilepticus is influenced by several factors:
Etiology: The underlying cause of status epilepticus is a significant prognostic factor.
Consciousness Level on Presentation: The patient’s level of consciousness upon arrival at medical care is an important predictor of outcome.
First-Time Presentation: If status epilepticus is a patient’s first-ever seizure event, the likelihood of an underlying structural brain lesion is significantly higher (greater than 50%).
Status epilepticus is associated with a high overall mortality rate.
Education for Caretakers and Individuals with Status Epilepticus
Comprehensive education is vital for patients, families, and the community to improve understanding and management of epilepsy:
Nature of Epilepsy: Educate that status epilepticus, like epilepsy in general, is a medical condition that can be effectively treated, allowing individuals to lead fulfilling lives.
Encourage Full Participation: Encourage individuals with epilepsy to participate fully in life and enjoy activities to the extent possible.
Combat Stigma and Isolation: Address and combat stigma, isolation, and labeling associated with epilepsy, which can be deeply traumatizing.
School Inclusion: Children with epilepsy should be encouraged to attend school and participate in educational activities.
Teacher and School Staff Education: Educate teachers, school children, and school personnel about epilepsy to promote understanding, reduce stigma, and ensure appropriate support in the school environment.
Adult Life and Marriage: Adults with epilepsy can marry and should be encouraged to pursue relationships and family life.
Safety Precautions: Educate individuals with epilepsy to avoid dangerous activities that pose a risk of injury during a seizure, such as:
Driving motor vehicles
Climbing heights
Operating heavy machinery
Swimming alone
Non-Contagious Nature: Emphasize that epilepsy and status epilepticus are not contagious and patients should be treated fairly and with respect, like any other individual with a medical condition.
Seizure Control with Medication: Reassure that epileptic seizures can be effectively controlled with consistent adherence to prescribed medication regimens.
When Status Epilepticus Becomes an Emergency
Status epilepticus is always a medical emergency, but certain situations warrant immediate and urgent attention:
First-Time Seizure: If the person has never had a seizure before, it is crucial to seek immediate medical evaluation.
Breathing or Walking Difficulties Post-Seizure: If the person experiences difficulty breathing or walking after a seizure, emergency medical attention is needed.
Prolonged Seizure Duration: If a seizure lasts longer than 5 minutes, it is considered status epilepticus and requires emergency intervention.
Recurrent Seizures: If a person has another seizure shortly after the first one, without regaining full consciousness in between, it is a medical emergency.
Injury During Seizure: If the person is injured during the seizure, medical evaluation and treatment are necessary.
Seizure in Water: Seizures occurring in water pose a high risk of drowning and require immediate emergency response.
Pre-existing Health Conditions: If the person has underlying health conditions such as diabetes, heart disease, or pregnancy, status epilepticus is more concerning and requires urgent medical care.
Prevention of Status Epilepticus
Preventive measures focus on reducing risk factors and managing underlying conditions:
Head Injury Prevention: Prevent head injuries through safety measures such as:
Wearing seat belts in vehicles.
Using bicycle helmets when cycling.
Prompt Medical Care for First Seizure: Seek immediate medical evaluation and management after experiencing a first seizure event.
Prenatal Care: Encourage pregnant mothers to obtain good prenatal care to minimize the risk of brain damage to the developing fetus, which can be a risk factor for epilepsy.
Hypertension Management: Effective treatment and management of hypertension (high blood pressure) can reduce stroke risk, a potential cause of seizures in older adults.
Avoid Excessive Alcohol: Avoid excessive alcohol abuse and limit alcohol intake, as alcohol withdrawal can trigger seizures in susceptible individuals.
Fever Control in Children: Aggressively treat high fevers in children to prevent febrile seizures.
Infection Treatment and Nutrition: Prompt treatment of infections and ensuring proper nutrition, including adequate vitamin intake, can contribute to overall neurological health and potentially reduce seizure risk.
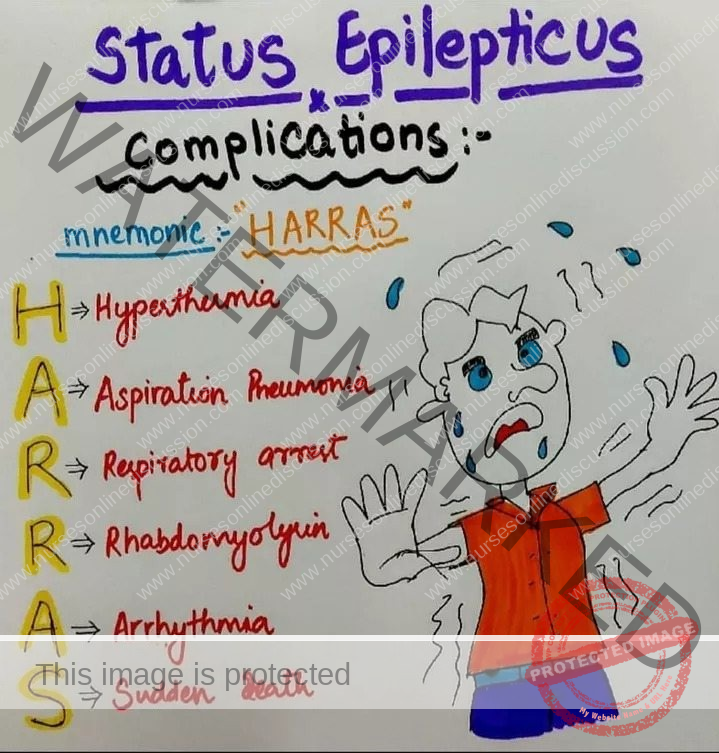
Complications of Status Epilepticus
Status epilepticus is a severe condition with potentially life-threatening complications:
Hyperthermia (dangerously high body temperature).
Aspiration pneumonia (lung infection due to aspiration of saliva or vomit).
Respiratory arrest (cessation of breathing).
Rhabdomyolysis (breakdown of muscle tissue, releasing harmful substances into the bloodstream).
Cardiac arrhythmias (irregular heart rhythms).
Sudden unexplained death in epilepsy (SUDEP).
Specific Nursing Care for a Patient with Status Epilepticus
Nurses play a critical role in the immediate and ongoing management of patients experiencing status epilepticus. Their actions are vital in ensuring patient safety and optimal outcomes. Key nursing responsibilities include:
Assessment and Continuous Monitoring:
Vital Signs Surveillance: Regularly observe and meticulously document the patient’s vital signs. This includes:
Heart rate
Blood pressure
Oxygen saturation levels
Seizure Observation and Documentation: Continuously monitor and carefully record:
Seizure duration
Seizure frequency
Specific seizure characteristics (e.g., type of movements, body parts involved).
Neurological Status Assessment: Evaluate and document the patient’s:
Level of consciousness (LOC)
Neurological status, including responsiveness and orientation.
Safety Environment Maintenance: Proactively ensure a safe patient environment by:
Removing any potential hazards or obstacles from the immediate vicinity that could cause injury during seizure activity.
Medication Administration:
Antiepileptic Drug (AED) Administration: Promptly administer prescribed Antiepileptic Drugs (AEDs) as per physician orders. This may involve:
Intravenous (IV) administration for rapid onset.
Intramuscular (IM) administration if IV access is not immediately available.
Common medications include benzodiazepines such as lorazepam, diazepam, or midazolam to rapidly terminate seizures.
Dosage Accuracy and Monitoring:
Double-check and ensure accurate medication dosages are administered.
Closely monitor the patient for any adverse reactions or side effects to the administered medications.
Airway and Respiratory Management:
Lateral Positioning: Position the patient on their side (recovery position) to:
Minimize the risk of aspiration should vomiting occur during or following a seizure.
Supplemental Oxygen: Administer supplemental oxygen therapy if the patient exhibits signs of respiratory distress, such as:
Labored breathing
Cyanosis
Decreased oxygen saturation.
Intravenous (IV) Access Management:
Establish and Maintain IV Line: Establish and maintain patent intravenous access to:
Facilitate rapid administration of emergency medications.
Provide intravenous fluids for hydration and medication dilution.
Blood Glucose Monitoring:
Check Blood Glucose Levels: Regularly monitor blood glucose levels using point-of-care testing to:
Rule out hypoglycemia as a potential trigger or contributing factor to seizures.
Detailed Seizure Documentation:
Maintain Precise Seizure Records: Keep meticulous and accurate records of all seizure activity, including:
Seizure start time
Seizure stop time
Detailed description of seizure characteristics (e.g., tonic-clonic, focal, absence)
Any associated symptoms observed before, during, or after the seizure event.
Emotional Support and Reassurance:
Provide Emotional Support: Offer empathetic and compassionate emotional support to both the patient and their family members who are likely experiencing significant anxiety and distress.
Explain Care Plan: Clearly explain the ongoing plan of care and the treatment strategies being implemented to manage the status epilepticus and address their concerns.
Injury Prevention Measures:
Implement Safety Precautions: Take proactive steps to prevent patient injuries during seizures:
Pad bed side rails with protective padding to cushion against injury from involuntary movements.
Implement other protective measures in the environment to minimize risks.
Protect the patient from self-inflicted injuries due to uncontrolled movements.
Restraint Use (If Necessary): Utilize soft restraints only if absolutely necessary and appropriately prescribed to ensure patient safety and prevent accidental self-harm during severe seizures.
Ongoing Neurological Assessment:
Continuous Neurological Monitoring: Continuously assess and document the patient’s neurological status to detect any changes or deterioration. This includes monitoring:
Pupil size and reactivity to light.
Responsiveness to verbal and painful stimuli.
Motor function and strength in extremities.
Collaboration and Referral:
Neurology Consultation: Actively consult with a neurologist or epilepsy specialist as soon as possible for:
Expert evaluation of the patient’s condition.
Guidance on further diagnostic workup and specialized management strategies.
Consideration of transfer to a higher level of care if needed.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

