Introduction to Occupational Health Hazards
Subtopic:
Injection safety and management
Introduction to Injection Safety
Injections are an extraordinarily common medical procedure globally. It is estimated that approximately 95% of injections are administered for therapeutic purposes, treating a wide range of illnesses. Immunizations account for about 3% of all injections given, playing a vital role in disease prevention. The remaining injections are utilized for diverse medical reasons, such as blood transfusions, contraceptive administration, and diagnostic procedures.

Addressing the Problem of Unnecessary Injections:
A significant challenge in many developing and transitional countries is the overuse of injections, with a substantial proportion being administered when oral medications would be equally or more appropriate and effective. Studies indicate that in some primary healthcare settings, as many as 9 out of 10 patient visits result in an injection. However, it is estimated that over 70% of these injections are clinically unnecessary and could be effectively replaced by oral medication formulations, highlighting the need for rationalizing injection practices and promoting oral alternatives when appropriate.
Importance of Safe Injection Practices:
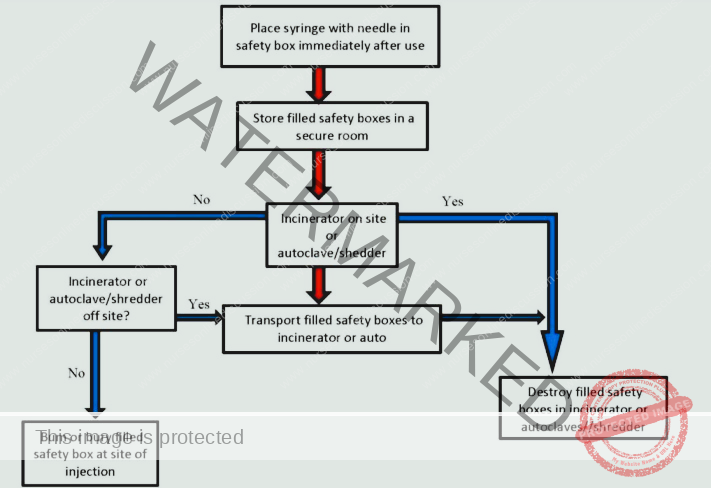
Following injection administration, the safe collection and disposal of used needles and syringes are critically important components of comprehensive injection safety. Proper waste management is integral to ensuring injection safety from start to finish, protecting healthcare workers, patients, and the community.
Three Key Dimensions of Injection Safety:
When evaluating the safety of injection practices, three fundamental considerations must be prioritized:
Patient Safety: Ensuring the safety and well-being of the individual receiving the injection is paramount. Safe injection practices protect patients from infection, injury, and other adverse events associated with injections.
Healthcare Worker Safety: Protecting the safety and well-being of the healthcare worker administering the injection is equally crucial. Safe injection techniques and protocols minimize the risk of accidental needle-stick injuries and occupational exposure to bloodborne pathogens.
Community Safety: Ensuring the safety and protection of the broader community where injections are being administered is a vital public health responsibility. Safe injection practices and proper waste disposal prevent the spread of infections within communities and minimize environmental hazards associated with improperly discarded sharps waste.
Therefore, upholding injection safety is not only a matter of individual patient and provider safety, but also a critical component of broader public health and community well-being.
Injection Safety Guidelines (WHO, 2005)
According to the World Health Organization (WHO) guidelines established in 2005, a safe injection is comprehensively defined as one that:
Causes No Harm to the Recipient: Does not result in any adverse health consequences or complications for the person receiving the injection, ensuring patient safety and well-being.
Presents No Unnecessary Risk to the Provider: Does not expose the healthcare worker administering the injection to any avoidable occupational hazards or risks, protecting their safety and health.
Generates No Dangerous Waste: Does not create hazardous or improperly managed waste that could pose a risk to the community or the environment, emphasizing responsible waste disposal practices.
Principles to Follow for Safe Injections:
Adherence to the following core principles is essential for ensuring safe injection practices:
Single-Use Syringes and Needles: Always use a brand new, sterile, single-use syringe and needle for each injection administered to every patient. Never reuse syringes or needles, even if the needle is changed. Single-use equipment is critical to prevent patient-to-patient transmission of bloodborne pathogens.
Maintaining Equipment Sterility: Maintain the sterility and cleanliness of all injection equipment and vaccine vials throughout the preparation and administration process. Proper aseptic technique is paramount to prevent contamination and reduce the risk of injection-site infections.
Clean Injection Preparation Area: Prepare injections in a designated clean and aseptic area where the risk of contamination is minimized. Choose a location with:
Low likelihood of airborne contaminants.
Minimal chance of contamination from blood or other bodily fluids.
A clean and disinfected work surface.
Sterile Needle for Multi-Dose Vial Entry: When accessing multi-dose vials, always use a clean, sterile needle to puncture the rubber stopper each time a dose is withdrawn. This prevents contamination of the vial contents and maintains the sterility of subsequent doses.
Needle Left in Vial Stopper (Avoid): Do not leave the needle inserted into the rubber stopper of a multi-dose vial between uses. Leaving the needle in the stopper can compromise the sterility of the vial contents and increase the risk of contamination.
Finger Protection Opening Ampoules: When opening glass ampoules, protect your fingers using a small gauze pad or ampoule breaker. This simple precaution minimizes the risk of cuts or sharps injuries from broken glass during ampoule opening.
Discard Contaminated Needles: Immediately discard any needle that comes into contact with non-sterile surfaces, even inadvertently. If a needle touches anything that is not sterile, such as your hands, non-sterile surfaces, or the patient’s skin preparation site after disinfection, it is considered contaminated and must be discarded and replaced with a new sterile needle.
Anticipate Patient Movement: Be prepared for potential sudden movements from the patient both during and immediately after the injection. Secure the injection site and be ready for unexpected patient reactions to prevent needle-stick injuries or accidental displacement of the needle.
No Recapping of Used Needles: To prevent needle-stick injuries, never recap used needles. Recapping is a high-risk procedure that significantly increases the chance of accidental needle pricks.
Immediate Sharps Container Disposal: Immediately after use, dispose of used syringes and needles directly into a designated sharps container at the point of use. Place sharps containers conveniently close to where injections are administered to encourage immediate and safe disposal. Ensure sharps containers are:
Puncture-resistant to prevent needle penetration.
Clearly labeled as “sharps waste” for easy identification.
Properly sealed and closed when they reach the fill line, typically marked on the container.
Do not move, shake, or overfill sharps containers, as this increases the risk of sharps injuries and spillage of contaminated waste.
Safe Sharps Container Handling: Close and securely seal sharps containers according to established protocols before transporting them to a designated safe disposal area. Strictly adhere to safe handling procedures:
Do not attempt to reopen sealed sharps containers.
Never empty or reuse sharps containers, as this poses a significant risk of sharps injuries and infection exposure.
Environmentally Sound Waste Disposal: Handle and dispose of injection waste (sharps containers, contaminated materials) in a manner that is environmentally responsible and compliant with local regulations. Ensure that sharps waste is:
Segregated from general waste streams.
Treated as biohazardous waste and disposed of according to established protocols, such as incineration or autoclaving, to render it safe.
Prevent Sharps Injuries to Waste Handlers: Implement safe waste disposal procedures that are specifically designed to prevent accidental sharps injuries to waste handlers and sanitation workers involved in collecting and disposing of medical waste. Proper sharps container disposal and waste segregation are crucial to protect waste management personnel.
Vial Disposal: Do not place empty medication vials into sharps containers. Empty vials, while considered pharmaceutical waste, do not pose a sharps injury risk and should be disposed of separately, as sharps containers are specifically for needles and syringes. Empty vials may also burst or shatter if incinerated within sharps containers.
Sharps Container Contents (Limited to Sharps): Only place potentially contaminated injection equipment (used needles, syringes, lancets, sharps) into sharps containers. Avoid placing other types of waste, such as:
Empty medication vials (dispose of separately).
Cotton pads or gauze (dispose of in biohazardous waste bags).
General trash or non-sharps waste (dispose of in designated waste receptacles).
Sharps containers are specifically designed for sharps waste and should not be used for general medical waste disposal.
Guidelines for Safe Injection Practices (General)
Beyond sharps disposal, comprehensive safe injection practices encompass broader guidelines to prevent infection and ensure patient and provider safety:
Strict Infection Control: Rigorous adherence to infection control practices is paramount throughout the entire injection process, from medication preparation to administration and waste disposal. This includes:
Performing hand hygiene (handwashing or alcohol-based hand rub) before and after each injection.
Using appropriate skin disinfection techniques at the injection site.
Maintaining a clean and aseptic environment for injection preparation and administration.
Patient-Dedicated Syringes: Never use the same syringe for multiple patients, even if the needle is changed or if medication is administered through intravenous tubing. Cross-patient syringe reuse is a major cause of healthcare-associated infections.
No Vial Re-entry with Used Syringe: Never re-insert a used needle or syringe into a medication vial. Once a syringe or needle has been used on a patient, it is considered contaminated and should not be reintroduced into a medication vial, as this can contaminate the entire vial and pose a risk to subsequent patients if the vial is reused.
Single-Use Medication Vials: Do not use medications packaged in single-dose vials for more than one patient. Single-dose vials are intended for individual patient use only. Any remaining medication after a single dose should be discarded appropriately and not used for another patient, even if it appears to be unused.
Single-Patient IV Solution Bags: Do not use bags of intravenous (IV) solution for more than one patient. IV solution bags are intended for single-patient use. Leftover IV solution after a single patient’s infusion should be discarded appropriately and not used for another patient, as this can pose a risk of contamination and infection transmission.
Single-Patient Multi-Dose Vials (Preferred): Ideally, use multi-dose vials for a single patient whenever possible. While multi-dose vials are designed for multiple entries, limiting their use to a single patient minimizes the potential for cross-contamination between patients and enhances infection control.
Multi-Dose Vial Storage and Preparation: If using multi-dose vials, adhere to strict protocols for their storage and preparation:
Do not keep multi-dose vials in patient treatment areas or immediate patient care environments. Store multi-dose vials in a designated clean medication preparation area, away from potential contamination sources.
Prepare medications in a designated clean medication preparation area, away from any potential contamination sources, such as patient treatment areas or areas where used syringes or contaminated materials are handled. Do not prepare medications in close proximity to areas where used syringes are handled to minimize contamination risk.
Face Mask Use for Specific Injections: Wear a facemask during specific injection procedures that carry a higher risk of infection or contamination, such as:
When injecting material or placing a catheter into the epidural or subdural space (e.g., epidural anesthesia, spinal anesthesia). These procedures involve accessing sterile body cavities, requiring enhanced aseptic precautions, including facemask use.
Strategies to Prevent Unsafe Injection Practices
Preventing unsafe injection practices requires a multifaceted approach encompassing education, supervision, regulation, and infrastructure improvements:
Healthcare Worker Education: Implement comprehensive and ongoing education programs for all healthcare workers who administer injections. These programs should thoroughly cover:
All aspects of injection safety guidelines and protocols.
The risks associated with unsafe injection practices, including infection transmission and sharps injuries.
Proper techniques for injection preparation, administration, and safe disposal of sharps waste.
Healthcare Worker Supervision: Implement systems for supervising healthcare workers during medication administration and injection procedures. Supervision ensures:
Adherence to established injection safety protocols and best practices.
Identification and correction of any unsafe injection practices or deviations from standards.
Rules and Regulations Enforcement: Establish and rigorously enforce clear rules, regulations, and policies related to injection safety at all levels of the healthcare system. These regulations should mandate:
Adherence to safe injection techniques and protocols.
Proper sharps waste management and disposal procedures.
Accountability mechanisms for non-compliance with safety standards.
Qualified Healthcare Worker Recruitment: Prioritize the recruitment and retention of qualified and adequately trained healthcare workers. Sufficient staffing levels and trained personnel are essential for:
Ensuring safe and effective delivery of healthcare services, including injections.
Reducing workload pressures that may contribute to unsafe practices or shortcuts.
Intern Nurse Supervision: Provide close and direct supervision of intern nurses and novice healthcare providers when they are administering injections. Close supervision is crucial during the training and orientation period to:
Ensure they develop and consistently apply safe injection techniques from the beginning of their practice.
Prevent errors and unsafe practices through direct observation and guidance.
Preventing Needle-Stick Injuries
Accidental needle-stick injuries are a significant occupational hazard for healthcare workers. Implementing preventive measures is essential:
Utilize Safety Needles: Transition to and consistently use safety needles and sharps devices whenever possible. Safety needles incorporate engineered safety features, such as:
Retractable needles that automatically retract into the syringe after use, shielding the sharp point.
Shielded needles with protective covers that can be manually or automatically activated to cover the needle after use.
Safety-engineered needles significantly reduce the risk of accidental needle pricks by physically shielding the sharp point after injection.
Proper Needle Handling Techniques: Train healthcare workers on and strictly enforce proper needle handling techniques. This includes:
Handling needles with extreme care at all times.
Avoiding recapping used needles, a high-risk practice.
Immediately discarding used needles and sharps directly into designated sharps containers after each use, minimizing handling and transportation of unprotected sharps.
Personal Protective Equipment (PPE): Ensure that healthcare workers consistently wear appropriate personal protective equipment (PPE) whenever handling needles or potentially encountering blood or body fluids. This includes:
Always wearing gloves when administering injections, handling sharps, or cleaning up blood spills.
Using other appropriate PPE, such as eye protection or gowns, as needed based on the specific procedure and risk of exposure.
Safe Sharps Disposal Practices: Implement and reinforce safe sharps disposal practices throughout healthcare facilities. This includes:
Properly disposing of all used needles, syringes, and other sharps immediately after use into designated, puncture-resistant sharps containers.
Ensuring sharps containers are readily accessible and conveniently located in all patient care areas to encourage immediate and safe disposal.
Needleless Systems Adoption: Employ needleless systems and devices whenever clinically feasible and appropriate for medication preparation and administration. Needleless systems, such as needle-free IV connectors and medication vial access systems, significantly reduce or eliminate the need for needles in certain procedures, thereby minimizing needle-stick injury risks.
Engineering Controls Implementation: Invest in and implement engineering controls that are specifically designed to enhance sharps safety and minimize needle-stick risks. This includes:
Installing safety-engineered sharps disposal containers that are puncture-resistant, clearly labeled, and designed for safe and easy disposal.
Utilizing safety-engineered devices and equipment with built-in safety mechanisms to reduce needle exposure risks during procedures.
Comprehensive Education and Training: Provide thorough and mandatory education and training to all healthcare workers on all aspects of needle safety. Training programs should cover:
Proper needle handling techniques and best practices.
Safe sharps disposal protocols and procedures.
Appropriate use of safety-engineered needles and sharps devices.
Institutional sharps injury prevention policies and reporting procedures.
Sharps Injury Prevention Program: Establish a comprehensive sharps injury prevention program within healthcare facilities. This program should include:
Systematic identification of potential sharps injury risks and hazards in various clinical settings and procedures through risk assessments.
Providing clear guidance and protocols for sharps safety and injury prevention to all staff.
Establishing a confidential and non-punitive system for encouraging and facilitating the reporting of any needle-stick or sharps injury incidents, promoting a culture of safety and learning from incidents.
Safe Sharps Container Management: Train staff on safe procedures for managing sharps containers, including:
Properly closing and securely sealing sharps containers when they reach the designated fill line, preventing overfilling and potential sharps exposure.
Arranging for regular, scheduled disposal and replacement of full sharps containers with empty ones, ensuring timely and safe waste removal.
Sharps Container Accessibility: Ensure that sharps containers are readily accessible and conveniently located in all areas where injections are administered, medications are prepared, or sharps are used. Convenient placement encourages immediate and proper disposal of sharps at the point of use.
Post-Procedure Safety Focus: After completing any procedure involving needles or sharps, emphasize a conscious pause for safety before rushing to dispose of equipment. Take a moment to:
Ensure proper and immediate disposal of used needles and sharps into designated containers.
Verify that all safety measures have been followed and the immediate work area is left safe.
Open Communication and Collaboration: Foster a culture of open communication and collaboration among healthcare team members regarding needle safety concerns and potential risks. Encourage:
Open dialogue and feedback on sharps safety protocols and procedures.
Collaborative problem-solving to identify and implement safer practices.
Shared responsibility for maintaining a safe working environment and preventing sharps injuries.
Needleless Catheter Systems: Promote and implement the use of needleless catheter systems for intravenous (IV) access whenever clinically appropriate and feasible. Needleless systems, which eliminate needles for IV connections and medication administration, significantly reduce the overall need for needles in IV therapy and consequently lower needle-stick injury risks.
Safety Syringe Implementation: Transition to and consistently implement the use of safety syringes for injection administration across all relevant clinical settings. Safety syringes, equipped with built-in safety mechanisms, offer a significant layer of protection against needle-stick injuries during both injection and withdrawal phases of medication administration.
Regular Review and Protocol Updates: Establish a system for regularly assessing and updating needle safety protocols and procedures based on:
Emerging new safety technologies and best practices in sharps injury prevention.
Ongoing evaluation of sharps injury data and incident reports within the healthcare facility.
Continuous review and updates ensure that needle safety protocols remain current, effective, and aligned with the latest advancements in sharps injury prevention.
Managing an Accidental Needle Prick (Post-Exposure Protocol)
Accidental needle-stick injuries, while preventable, can still occur. Knowing how to respond promptly and appropriately is crucial to minimize potential risks:
Stay Calm and Assess: Immediately following a needle-stick injury, the first and most important step is to remain calm and avoid panic. Take a deep breath and quickly assess the situation to understand the nature of the exposure.
Encourage Bleeding (Do Not Squeeze Forcefully): If the needle-stick has caused a small cut or puncture wound, gently allow the wound to bleed freely for a short period. Do not squeeze the area forcefully, as gentle bleeding helps to naturally flush out any potentially infectious material from the wound.
Wash the Wound Thoroughly: Immediately and thoroughly wash the affected area with soap and running water. Wash the wound gently but thoroughly for a minimum of 20 seconds to effectively cleanse the puncture site and reduce the risk of infection.
Inform Supervisor Immediately: As soon as possible after the incident, inform your immediate supervisor or instructor about the accidental needle prick. Prompt reporting is crucial for initiating appropriate post-exposure protocols and documentation.
Report to Occupational Health: Report to your institution’s Occupational Health department or designated medical personnel for formal evaluation and management of the needle-stick injury. Occupational Health professionals will:
Assess the specific risk level associated with the exposure.
Provide guidance on necessary post-exposure actions, including testing and potential prophylaxis.
Identify Source Patient (If Possible): If feasible and without compromising patient confidentiality, attempt to identify the source patient – the individual whose blood or body fluids you were potentially exposed to through the needle-stick. Identifying the source patient is important for:
Assessing the potential risk of exposure to bloodborne pathogens such as HIV, Hepatitis B, and Hepatitis C.
Guiding decisions regarding post-exposure testing and prophylaxis.
Collect Exposure Information: Document and collect detailed information about the needle-stick incident. This documentation should include:
The type of exposure (e.g., needle gauge, hollow bore needle, visible blood).
The circumstances surrounding the needle-stick injury, including the procedure being performed and factors contributing to the accident.
Any available information about the source patient, if known.
Date and time of the incident.
Specific actions taken immediately after the exposure (e.g., washing wound, reporting).
Accurate and detailed documentation is crucial for medical evaluation, follow-up, and potential legal or insurance purposes.
Testing and Treatment Decisions: Based on the risk assessment and source patient information (if available), Occupational Health personnel will determine the need for:
Blood tests for the exposed healthcare worker to check for baseline infection status and monitor for potential seroconversion.
Blood tests for the source patient (if consent is obtained) to assess their status for bloodborne pathogens.
Post-Exposure Prophylaxis (PEP): Determine if post-exposure prophylaxis (PEP) is medically indicated to reduce the risk of infection, particularly for HIV exposure. PEP is most effective when initiated as soon as possible after exposure, ideally within hours.
Follow Medical Recommendations: If Post-Exposure Prophylaxis (PEP) or any other medical treatments are recommended or prescribed by Occupational Health, ensure you:
Carefully follow all medical recommendations and instructions provided by healthcare professionals.
Adhere strictly to the prescribed PEP regimen, including medication dosages and duration, to maximize its effectiveness in preventing infection.
Incident Documentation: Maintain a personal record of the needle-stick incident for your own files. This documentation should include:
Dates and times of the incident and subsequent medical evaluations.
All actions taken following the exposure.
Details of any medical treatments received, including PEP.
This personal record is important for your own medical history, potential future follow-up, and any workers’ compensation or insurance claims, if applicable.
Disposal criteria in mass immunization
Methods
Waste Burial Pit/Cement Encapsulation or Immobilization (using materials like sand or plaster)
Burning (at temperatures below 400°C)
Medium Temperature Incineration (ranging from 800°C to 1000°C)
High Temperature Incineration (above 1000°C)
Needle Removal/Needle Destruction (various models from manual to electrical)
Melting Syringes
Steam Sterilization (autoclaving, hydroclaving, microwaving with shredding)
Strengths
Waste Burial Pit/Cement Encapsulation or Immobilization
Straightforward application
Low implementation expenses
Technologically basic
Discourages syringe and needle re-employment
Mitigates risks of puncture injuries and infections for waste handlers and scavengers
Burning (<400°C)
Cost-effective method
Reduces the quantity of waste
Decreases infectiousness of materials
Medium Temperature Incineration (800°-1000°C)
More economical compared to high-temperature incinerators
Effective in reducing waste bulk
Reduces the potential for infection from waste materials
High Temperature Incineration (>1000°C)
Achieves nearly complete combustion and sterilization of injection tools
Further minimizes harmful emissions when equipped with pollution control technologies
Significantly decreases the total volume of immunization-related waste
Needle Removal/Needle Destruction
Stops needles from being reused
Lowers job-related hazards for those managing waste
Some plastics can be processed for recycling post-treatment
Available in both manual and battery-powered options
Melting Syringes
Substantially diminishes the waste volume
Prevents the reuse of syringes
Steam Sterilization
Long-standing successful method for treating both sharps and general healthcare waste from immunization activities
Offers a variety of models with different capacities
Effectively sterilizes used injection equipment
Results in fewer dangerous air emissions (minimal dioxins or heavy metals)
Waste volume is lessened when combined with shredding processes
Plastics can be recycled after being separated from other materials
Weaknesses
Waste Burial Pit/Cement Encapsulation or Immobilization
Possibility of waste being unearthed if pit coverage is inadequate and waste is not properly encased
Does not reduce the overall volume of waste
No disinfection of the waste is achieved
Pit can rapidly fill up during extensive immunization programs
Not advisable for infectious waste that is not sharp
Poses risks to the community if burial is not correctly done
Unsuitable for areas prone to heavy rainfall or with high water tables
Burning (<400°C)
Combustion process may be incomplete
Sterilization might not be fully effective
Produces significant smoke and carries fire risks
Requires fuel and dry waste to initiate burning
Releases toxic substances into the air (including heavy metals, dioxins, furans, and fly ash)
Generates hazardous ash that contains leachable metals, dioxins, and furans
Risk of needlestick injuries remains as needles are not destroyed
Medium Temperature Incineration (800°-1000°C)
Combustion may be incomplete
Potential for substantial smoke production
Demands fuel and dry waste for starting and maintaining high temperatures
Requires skilled personnel for operation
Potential release of toxic airborne pollutants (like heavy metals, dioxins, furans, and fly ash), possibly violating environmental or health regulations
Production of hazardous ash containing variable leachable metals, dioxins, and furans
Risk of needlestick injuries as some needles may remain intact
Needs consistent monitoring during operation and regular upkeep throughout the year
High Temperature Incineration (>1000°C)
High initial, operational, and maintenance costs
Needs electricity, fuel, and trained staff for operation
Toxic air emissions (like metals, dioxins, furans, fly ash) may still occur without effective pollution controls
Can produce hazardous ash with leachable metals, dioxins, and furans
Needle Removal/Needle Destruction
Splashes of fluid may contaminate the working area or operator
Fluid splashback and handling of needles can increase the risk of disease transmission in some situations
Used needles and syringes might need additional treatment for final disposal in certain cases
Safety profile is not fully defined
Melting Syringes
Releases potentially harmful gaseous emissions
Requires electricity to operate
Steam Sterilization
High initial investment
Requires both electricity and water
High ongoing operational expenses
Demands significant maintenance
May release volatile organic compounds in steam when depressurizing and opening the chamber
Requires further processing to prevent reuse (e.g., shredding)
Sterilized waste still necessitates appropriate final disposal
Injection Misuse and Overuse: Promoting Safe and Responsible Practices
Introduction: Addressing the Issue
Injections, while vital medical tools, are sometimes used inappropriately or excessively, leading to potential harm. It’s crucial to understand the reasons behind this misuse and overuse and to implement effective preventive strategies.
Reasons for Injection Misuse and Overuse:
Injections are sometimes misused or overused due to several factors:
Misconception of Superiority: Many believe injections are stronger and work faster than oral medications, leading to a preference for injections, even when unnecessary.
Perceived Doctor Preference: Some patients believe doctors consider injections the most effective treatment, influencing their expectations and requests for injections.
Patient Pleasing: Doctors may administer more injections to satisfy patient expectations and perceived demands, even when not clinically indicated.
Financial Incentives: In some healthcare systems, providers may be financially incentivized to give injections, as they can charge more for injection procedures, potentially leading to overuse.
Addressing Misunderstandings through Communication: Open communication and questions between patients and doctors are vital to:
Clear up misconceptions about injection benefits.
Promote informed decisions about appropriate treatment routes.
Reduce the overuse of unnecessary injections.
Negative Consequences of Injection Misuse and Overuse:
Misusing and overusing injections can have several harmful effects:
Infection Transmission: Unsafe injection practices, particularly during immunization, can transmit serious bloodborne diseases like Hepatitis B, Hepatitis C, and HIV/AIDS, posing significant public health risks.
Vaccine Side Effects: Improper injection technique during vaccination can, in rare cases, cause harmful side effects, highlighting the need for correct administration.
Healthcare Worker Injuries: Healthcare providers administering injections are at risk of needle-stick injuries from unsafe practices, leading to potential infection exposure.
Environmental Harm: Improper disposal of injection waste contaminates the environment (soil, air, water), posing ecological and public health risks.
Ineffective Immunization Programs: Misuse and overuse can undermine immunization program effectiveness, reducing public trust and potentially decreasing vaccine uptake, hindering disease prevention efforts.
Responding to Needle-Stick Injuries: A Step-by-Step Guide
If you experience an accidental needle-stick injury, follow these immediate steps:
Stay Calm: Take a moment to remain calm and assess the situation.
Let it Bleed: Allow the wound to bleed gently; do not suck or rub it.
Wash Thoroughly: Wash the area extensively with soap and running water for at least 20 seconds.
Remember Patient Details: If possible and appropriate, try to remember the patient’s name for accurate reporting.
Report to Occupational Health: Immediately report the incident to your occupational health unit for evaluation and guidance.
Inform Supervisor and Document: Notify your supervisor and document the incident details in writing.
Consider PEP (If Indicated): If the source patient is suspected to be HIV positive, post-exposure prophylaxis (PEP) may be recommended. Initiate PEP as soon as possible after exposure, following local guidelines.
NB: Staff should be thoroughly familiar with local PEP guidelines and protocols for needle-stick injuries.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

