Conditions of the Ear and Nose
Subtopic:
Foreign body in the ear and nose
A foreign body is defined as any material or object that is not naturally occurring within a particular part of the human body.
In the context of the ear and nose, foreign bodies are items that are unintentionally introduced or become trapped, leading to potential problems such as:
Discomfort and irritation.
Obstruction of normal function.
Potential medical complications if left untreated.
FOREIGN BODY IN THE EAR
A foreign body in the ear is defined as any object that has entered the ear canal and is not meant to be there.
In most instances, objects lodged in the ear canal are self-inserted, often due to curiosity or accident. Children between 9 months and 8 years old are particularly prone to this issue, as they are naturally inquisitive about their bodies and small objects.
Common objects children insert into their ears include:
Beads
Food items (especially beans or peas)
Paper
Cotton swabs (pieces of cotton)
Rubber erasers
Small toys
Marbles
Small shells
Types of Foreign Bodies in the Ear
Foreign bodies in the ear canal can be broadly classified into two categories:
Inanimate Foreign Bodies: These are non-living objects and can be further divided into:
a. Organic Inanimate Foreign Bodies: These are substances derived from living organisms or containing carbon compounds:
**Earwax (Cerumen)**: Excessive earwax buildup can cause impaction and blockage. * **Food**: Small food particles, like beans or seeds, can become lodged. * **Paper**: Scraps or pieces of paper. * **Cotton Swab Pieces**: Fragments of cotton swabs, often from improper ear cleaning. * **Rubber Erasers**: Small eraser pieces from pencils. * **Small Toys**: Toy components or small play objects. * **Marbles**: Small glass or plastic marbles. * **Small Shells**: Shells from beaches or decorative shells.b. Inorganic Inanimate Foreign Bodies: These are substances not derived from living organisms and lack carbon compounds. They often include metallic or plastic materials:
* **Beads**: Small plastic or glass beads.Animate Foreign Bodies: These are living organisms that enter the ear canal:
Insects: Insects, such as flies, ants, or small beetles, may crawl or fly into the ear, especially during sleep on the floor or outdoors. Live insects like bed bugs, mosquitoes, and cockroaches can also enter the ear canal.
Myiasis (Maggots): Flies may lay eggs in the ears of individuals with chronic suppurative otitis media (CSOM), a chronic ear infection, leading to maggots hatching and infesting the ear canal.
Signs and Symptoms of Foreign Body in the Ear
The signs and symptoms of a foreign body in the ear can vary, but common presentations include:
Pain (Otalgia): Often the most prominent symptom, ranging from mild irritation to severe pain. The ear canal is highly sensitive to pressure and irritation.
Hearing Loss: Partial or complete hearing loss in the affected ear is frequent, particularly if the object obstructs a significant portion of the ear canal, blocking sound transmission.
Ear Discharge (Otorrhea): Discharge from the ear may occur, varying in nature depending on the object and duration of impaction:
Bloody discharge (otorrhagia), especially if the object is sharp or has caused trauma.
Purulent discharge (pus), indicating infection has developed.
Inflammatory fluid, a serous or mucoid discharge due to irritation.
Itching (Pruritus) and Irritation: The ear canal’s sensitivity leads to itching and irritation, often prompting the individual to scratch or rub the ear, potentially worsening the situation.
Sensation of Fullness or Pressure: A feeling of ear fullness or pressure is common, especially if the object is lodged deeply in the ear canal, creating a blockage.
Less Common Symptoms:
Nausea and Vomiting: Irritation of the ear canal can sometimes stimulate the vagus nerve, which has branches in the ear, triggering nausea and, less frequently, vomiting.
Coughing or Throat Clearing: Vagal nerve stimulation can also induce coughing or a sensation of needing to clear the throat.
Tinnitus: Buzzing, ringing, or other noises in the ear (tinnitus) may arise if the foreign body is moving within the ear canal or if it irritates inner ear structures.
Dizziness and Vertigo: In rare cases, a foreign body can cause inflammation or pressure buildup in the middle ear (if it perforates the eardrum or is positioned near it), potentially leading to dizziness and vertigo (a sensation of spinning).
Unsteady Gait: Dizziness and vertigo from middle ear involvement can sometimes result in unsteadiness when walking or loss of balance.
Symptom Variation Based on Object Type:
Insects: The movement of a live insect within the ear canal often causes a distinct buzzing or fluttering sensation, along with discomfort and distress.
Earwax Impaction: Earwax blockage typically leads to a gradual onset of ear fullness, pressure, and progressive hearing loss in the affected ear.

Diagnosis and Investigations of Foreign Bodies in the Ear
Diagnosing a foreign body in the ear typically involves a combination of clinical information and physical examination. In some situations, imaging or hearing tests may also be necessary.
Patient History Collection: A detailed history is essential for accurate diagnosis. This involves gathering information from the patient or, in the case of children, their caregiver, concerning:
Nature of the Foreign Body: Identifying what object is suspected of being lodged in the ear canal (e.g., bead, insect, food particle).
Duration of Symptoms: Determining how long the symptoms have been present, including when the object insertion likely occurred.
Attempted Removal History: Inquiring about any prior attempts to remove the object, whether by the individual or others, and the methods used, as these attempts may complicate removal or cause further injury.
Physical Ear Examination: A thorough physical examination is crucial for visualizing and assessing the situation. This typically includes:
External Ear Inspection: Visual inspection of the outer ear (auricle and surrounding skin) for any signs of:
Redness (erythema)
Swelling (edema)
Discharge
Trauma or injury.
Otoscopy: Using an otoscope, a specialized instrument with a light and magnifying lens, to directly visualize:
The ear canal to identify the foreign body, its type, size, and position.
The tympanic membrane (eardrum) to assess for:
Perforation (rupture)
Inflammation
Signs of middle ear involvement.
Symptom Assessment: Evaluating for any accompanying symptoms, such as:
Pain level and character.
Presence and nature of ear discharge (otorrhea).
Subjective hearing loss reported by the patient.
Imaging Studies (Selective Use): In certain cases, imaging may be indicated to provide further information about the foreign body and surrounding structures. The selection of imaging modality depends on clinical suspicion and the nature of the foreign body:
a. Radiography (X-ray): Plain X-rays can be helpful in detecting:
* Radiopaque foreign bodies: Objects that are dense and block X-rays, such as metallic objects (e.g., metal fragments) or button batteries.
* Limitations: X-rays are often less effective for visualizing non-radiopaque objects, such as plastic, wood, or organic materials. They also provide limited detail regarding the object’s precise location within the ear canal.b. Computed Tomography (CT) Scan: CT scans offer more detailed and sensitive imaging compared to X-rays. CT scans are particularly valuable for:
* Complex or Deep-Seated Foreign Bodies: Situations where the foreign body is suspected to be deeply lodged or difficult to visualize with otoscopy alone.
* Detailed Anatomical Information: Providing detailed anatomical images of the ear canal, middle ear, and surrounding bone structures, aiding in pre-procedural planning, especially for complex removals.Audiometry (Hearing Test): If there is concern about potential damage to the ear’s hearing function, particularly if the tympanic membrane is involved, or if hearing loss is reported, audiometry (hearing tests) may be performed. This is done to:
Objectively assess the patient’s hearing acuity in the affected ear.
Determine if there is any conductive or sensorineural hearing loss resulting from the foreign body or attempted removal.
Treatment and Management of Foreign Body in the Ear
Upon a patient’s arrival at the hospital with a suspected foreign body in the ear, the initial approach prioritizes creating a welcoming and comfortable environment before commencing the removal process.
Initial Patient Assessment:
Biodata Collection: Gather essential patient details, including name, age, contact information, and relevant medical history.
Detailed History Elicitation: Obtain a comprehensive account of the incident, focusing on:
The nature of the suspected foreign object.
How long the object has been lodged in the ear.
Any associated symptoms the patient is experiencing.
Ear, Nose, and Throat (ENT) Specialist Consultation:
Prompt Referral: Immediately refer the patient to an ENT specialist for expert evaluation and management.
ENT Examination: The ENT specialist will conduct a thorough examination of the ear, utilizing an otoscope to:
Visually identify the foreign body.
Determine the object’s location within the ear canal.
Assess the characteristics of the foreign body.
Therapeutic Approach Determination:
Individualized Removal Plan: The ENT specialist will decide on the most suitable removal technique, taking into account:
The foreign body’s size and dimensions.
Its shape and configuration.
The material composition of the object.
The precise location of the object within the ear canal.
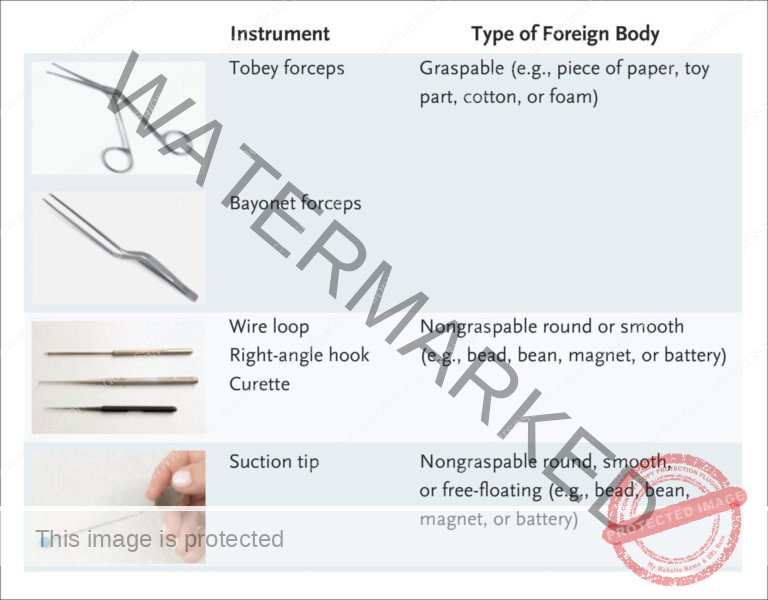
Removal Techniques: A variety of techniques may be employed, depending on the specific case, including:
Gentle suction using specialized equipment.
Fine forceps for grasping and extraction.
Looped instruments designed for foreign body retrieval.
Magnetic tools, specifically for removing metallic foreign bodies.
Ear Canal Irrigation: If the eardrum is confirmed to be intact, warm water irrigation using a small, flexible catheter may be utilized to gently flush out the object.
Sedation Considerations: In the case of young children or individuals who may not tolerate potentially uncomfortable removal procedures, sedation may be considered to ensure cooperation and minimize distress.
Management of Specific Foreign Body Types:
Insects: For live insects in the ear canal:
Insect Immobilization: Typically, insects are first immobilized and killed by instilling lidocaine (anesthetic) or mineral oil into the ear canal.
Gentle Irrigation: Following insect death, gentle irrigation with warm water is often used to flush out the insect.
Button Batteries: Button batteries require immediate and urgent removal due to the significant risk of chemical burns and tissue damage from battery leakage.
Food or Plant Matter: Organic materials like food or plant matter necessitate prompt removal as they can:
Swell and expand upon contact with moisture in the ear canal.
Lead to increased obstruction and patient discomfort.
Live Animate Objects: Living foreign bodies, like insects, can be killed by instilling oily ear drops into the ear canal. This suffocates the insect, which can then be:
Removed using forceps.
Extracted with gentle syringe irrigation.
Inorganic and Small Objects: For inanimate objects such as metallic foreign bodies, glass beads, and small food grains, removal can often be achieved by:
Ear syringing with warm water.
Magnetic Removal: Magnets can sometimes be effective for extracting metallic objects.
Suction: Suction devices can assist in gently pulling out certain foreign bodies.
Forceps Extraction: If the object is readily visible and easily grasped, fine tweezers may be used for gentle removal.
Post-Removal Otoscopic Examination: After removing any foreign body, a thorough re-examination of the ear canal using an otoscope is essential to:
Check for any trauma or injury to the ear canal walls.
Antibiotic Ear Drops (Prophylactic Use): Antibiotic ear drops may be prescribed, typically for a short course, to prevent potential secondary infections, particularly if there was trauma or risk of contamination during removal.
Post-Removal Aftercare:
Antibiotic Ear Drops: If prescribed, administer antibiotic ear drops for the duration recommended by the ENT specialist, usually 5-7 days, to prevent infection.
Follow-Up Appointment: A follow-up appointment within approximately one week is typically advised to:
Ensure proper healing of the ear canal.
Assess for any signs of complications.
Address any persistent symptoms.
If persistent issues like bleeding, ear discharge, or pain are present, further evaluation and management are necessary.
Indications for Urgent Foreign Body Removal: Immediate removal of a foreign body is warranted in situations involving:
Severe Pain: Intense ear pain or escalating discomfort.
Significant Hearing Loss: A noticeable decrease in hearing acuity in the affected ear.
Dizziness: Onset of dizziness or vertigo, suggesting possible middle ear involvement or irritation of the inner ear.
General Management Principles (Key Considerations for Removal)
Avoid Forceps for Deep Insertion: Do not attempt to use forceps to grasp objects deeply lodged in the ear canal, as this may push the object further inward, increasing impaction and risk of eardrum injury.
Forceps for Edge Grasping: If the foreign body presents an edge or projection that can be safely grasped, Hartmann forceps (or similar “crocodile” forceps), designed for ear procedures, may be used for extraction.
Syringing with Lukewarm Water: Ear syringing using lukewarm water is a common technique for non-impacted, mobile foreign bodies, particularly smooth, round objects.
Foreign Body Hook for Syringing Failures: If syringing proves ineffective in removing the foreign body, a specialized foreign body hook can be used by trained personnel to gently manipulate and extract the object.
General Anesthesia in Children: In young or uncooperative children, general anesthesia may be required to ensure safe, atraumatic, and effective removal, especially for deeply embedded or challenging foreign bodies.
Insect Immobilization Before Syringing: For insects, always kill or immobilize the insect first using clean cooking oil or water before attempting to syringe it out with warm water. This prevents the insect from further agitation and potential damage during removal attempts.
Syringing for Smooth, Round Objects: For smooth, round foreign bodies that are not impacted, syringing with lukewarm water is often the initial removal method of choice.
Foreign Body Hook for Syringing Failures (Round Objects): If syringing is unsuccessful for round objects, a foreign body hook can be employed for extraction.
General Anesthesia (Children and Sensitive Adults): General anesthesia may be necessary for foreign body removal in:
Children who are unable to cooperate with removal procedures.
Sensitive adults who may experience significant discomfort or anxiety during removal.
Avoid Forceps on Round Objects: Do not use forceps to attempt to grasp round objects lodged in the ear canal. This approach is likely to simply push the object further into the canal, making removal more difficult and potentially causing injury.
Hartmann Forceps for Edged Objects: For foreign bodies with an edge or graspable point, Hartmann (crocodile) forceps are appropriate for gentle and controlled removal.
Cockroach Removal with Forceps: Cockroaches are best removed with crocodile forceps rather than syringing, as their legs have hooks that can make syringing ineffective and potentially traumatic.
Avoid Syringing Impacted Seeds: Do not syringe with water if the foreign body is a seed. Water can cause seeds to swell, potentially worsening the impaction and making removal more challenging. Immediate referral is advised if seed removal with a hook is not possible.
Suction for Specific Foreign Bodies: Suction devices can be useful for removing certain types of foreign bodies that can be grasped or drawn into the suction tip.
Magnetic Removal of Metallic Objects: Magnets can be utilized in cases where the foreign body is confirmed to be metallic, providing a non-traumatic removal option.
Post-Removal Antibiotic Ear Drops and Pain Relief: After successful removal, antibiotic ear drops are often prescribed to prevent secondary infection. Pain relievers (analgesics) may also be recommended to manage any post-procedure discomfort.
WAX IN THE EAR OR IMPACTED CERUMEN
Impacted cerumen (earwax) refers to an accumulation of earwax in the external ear canal that becomes excessive and causes obstruction of the external acoustic meatus (ear canal opening).
Earwax is a normal, naturally produced substance in the external ear canal. It is composed of:
Epithelial scales (shed skin cells).
Secretions from specialized glands within the skin of the outer ear canal.
Earwax serves a protective function in the ear canal, trapping dust, debris, and microorganisms, and typically self-expels naturally over time. In most individuals, earwax naturally migrates out of the ear canal without intervention. However, in some cases, it accumulates and forms a wax plug, causing blockage and potentially leading to hearing impairment.
Causes of Impacted Cerumen
Factors contributing to impacted earwax include:
Excessive or Thick Wax Production: Some individuals naturally produce more earwax or wax with a thicker consistency, increasing the likelihood of impaction.
Narrow, Tortuous, or Hairy Ear Canal: The anatomy of the ear canal, if narrow, winding (tortuous), or excessively hairy, can hinder natural wax expulsion, leading to buildup.
Ear Pad or Hearing Aid Use: Regular use of ear pads (earplugs, headphones) or hearing aids can impede the natural migration of earwax out of the ear canal, promoting impaction.
Cotton Swab Use: Paradoxically, attempts to clean the ears with cotton swabs often push earwax further into the canal, contributing to impaction rather than removing wax effectively.
Clinical Features of Impacted Cerumen
Common symptoms of impacted earwax include:
Sensation of Blocked Ears: A feeling of ear blockage or fullness in the affected ear.
Tinnitus (Ear Noises): Buzzing, ringing, or other sounds in the ear.
Hearing Loss: Reduced hearing acuity in the affected ear, often described as a muffled or plugged sensation.
Mild Pain (Otalgia): In some cases, mild ear pain or discomfort may be present due to pressure from the wax plug.
Management of Impacted Cerumen
Management aims to soften and remove the impacted wax safely:
Ceruminolytic Ear Drops (Wax Softeners): Initial treatment often involves using ear drops to soften the impacted wax. Common types include:
Olive oil
Vegetable oil
Glycerine
Sodium bicarbonate ear drops
Liquid paraffin ear drops
Application: Instill ear drops three times a day for a few days to soften the wax plug. Often, after softening, the earwax will naturally fall out on its own due to normal ear canal movements.
Ear Syringing (Irrigation): If ear drops alone are insufficient to remove the wax plug, ear syringing may be necessary.
Warm Water Irrigation: Use clean water warmed to body temperature for ear syringing. This is crucial to:
Soften the impacted wax during irrigation.
Minimize stimulation of the inner ear, which could induce dizziness or vertigo.
Syringing Procedure Timing: Perform ear syringing after the wax has been softened by ear drops to facilitate easier and less traumatic removal.
Gentle Drying: After syringing, gently dry the ear canal to remove excess moisture.
Otoscopic Re-Examination: Following syringing, re-examine the ear canal with an otoscope to:
Confirm complete wax removal.
Exclude any damage to the tympanic membrane (eardrum) caused by syringing.
Important Notes on Wax Removal
Avoid Sharp Objects: Advise patients strongly against using any sharp objects (e.g., cotton swabs, hairpins, keys) in the ear canal in an attempt to remove earwax. This practice is highly risky and can lead to:
* Eardrum damage (perforation).
* Ear canal injury or infection.Contraindications for Syringing: Do not perform ear syringing in the following situations:
* History of ear discharge (otorrhea), which may indicate a perforated eardrum or active infection.
* Presence of ear pain (otalgia), which may suggest underlying infection or eardrum perforation.
Complications of Foreign Body in the Ear (and Removal Attempts)
Potential complications associated with foreign bodies in the ear and their removal include:
Ear Canal Infection (Otitis Externa): Infection of the external ear canal is a possible complication, but it usually:
Responds well to topical antibiotic ear drops.
Tympanic Membrane (Eardrum) Damage: Attempts at self-removal or improper removal techniques, especially with sharp objects, can potentially cause:
Eardrum perforation (rupture), leading to hearing loss and potential middle ear infection.
Persistent Symptoms: Ongoing symptoms like pain, bleeding, or ear discharge following foreign body removal may indicate:
Residual irritation or inflammation.
Injury to the ear canal.
Secondary infection.
FOREIGN BODIES IN THE NOSE
Foreign body in the nose refers to any object that has been placed into the nasal cavity and is causing symptoms or obstruction.
Foreign bodies in the nasal passages are relatively common, particularly in:
Children, especially toddlers, due to their exploratory behavior.
Adults with intellectual disabilities or cognitive impairment, who may lack awareness or control over object insertion.
Objects typically enter through the anterior nares (nostrils). However, foreign bodies can also:
Enter from the mouth or stomach during vomiting or forceful coughing.
Be unintentionally left in the nose during nasal surgery or procedures.
Types of Foreign Bodies in the Nose
Common types of foreign objects found in the nasal passages include:
Small Toys: Miniature toys or toy parts, such as:
Lego bricks
Small beads
Miniature action figures.
Children, especially toddlers, may insert these out of curiosity or during play.
Eraser Pieces: Fragments of erasers from pencils or other stationery items, which can break off and become lodged.
Tissue Paper: Pieces of tissue paper or facial tissue, especially if inserted while attempting to stop a nosebleed or accidentally during nose blowing.
Clay or Modeling Compounds: Small pieces of clay, playdough, or modeling materials used in arts and crafts, particularly in children.
Food Items: Small food particles, such as:
Peas
Beans
Nuts
Other small edible items, often inserted by young children while eating or playing.
Small Objects from Outdoors: Items children may pick up while playing outside, such as:
Small stones
Pebbles
Dirt clods or mud.
Paired Disc Magnets: Small, powerful disc magnets, often used for attaching earrings or nose rings, can be hazardous if inserted in the nose. When multiple magnets are inserted, they can:
Attract each other across the nasal septum (the wall separating the nostrils).
Cause pressure necrosis and damage to the nasal tissue over time, potentially leading to septal perforation.
Button Batteries: Small, round button batteries, commonly found in watches, hearing aids, and electronic toys, pose a serious hazard if inserted into the nose. Button batteries can cause:
Liquefaction necrosis: Severe tissue damage due to battery leakage and chemical burns.
Emergency: Button battery insertion into the nose requires immediate and urgent medical attention.
Clinical Manifestations of Nasal Foreign Body
The presentation of a nasal foreign body can vary, but common signs and symptoms include:
Visible Foreign Body: In some cases, the foreign object may be directly visible upon external nasal examination or during anterior rhinoscopy.
Nasal Congestion: Blockage of the nasal passage on the affected side, leading to nasal stuffiness or difficulty breathing through the nostril.
Persistent Sneezing: Irritation from the foreign body can trigger frequent and persistent sneezing.
Breathing Difficulty: If the foreign body obstructs a significant portion of the nasal passage, it can cause difficulty breathing through the nose, potentially leading to mouth breathing.
Irritability: Discomfort and inability to communicate the problem, particularly in infants and young children, may manifest as general irritability and restlessness.
Persistent Crying (Infants): In infants, nasal foreign bodies can cause persistent crying or fussiness due to discomfort and nasal obstruction.
Blood-Tinged Nasal Discharge: Nasal discharge streaked with blood (blood-tinged) can occur due to irritation or trauma to the nasal mucosa from the foreign body.
Rhinorrhea: Runny nose or nasal discharge, which may be clear, mucous-like, or mucopurulent depending on the duration and presence of infection.
Foul-Smelling Nasal Discharge: A particularly concerning sign is a unilateral, foul-smelling nasal discharge, which is highly suggestive of a nasal foreign body, especially if the discharge is also blood-stained. The foul odor is often due to trapped secretions and bacterial overgrowth behind the obstruction.
Diagnosis of Nasal Foreign Body
Diagnosing a nasal foreign body typically involves:
History: A patient history, particularly in children with sudden onset of nasal obstruction and discharge. A history of unilateral, foul-smelling, and bloody nasal discharge in a child should raise strong suspicion of a nasal foreign body.
Anterior Rhinoscopy: Examination of the nasal cavity using an anterior rhinoscopy technique, involving a nasal speculum and a light source. This may:
Directly reveal the foreign body in some cases.
Show the foreign body may be obscured by mucopurulent discharge (pus-containing mucus) and granulations (inflammatory tissue) that have formed around the object over time.
Probing: Gentle probing of the nasal cavity using a blunt probe may help to:
Detect the presence of a foreign body if it is not immediately visible.
Radiological Examination (Selective Cases): Radiological examination (X-ray) of the nose and sinuses may be helpful in certain cases, particularly to:
Identify radiopaque foreign bodies, such as metallic objects or button batteries, which are visible on X-ray.
Management of Nasal Foreign Body
Nasal foreign body removal typically involves the following steps:
Patient Positioning: The patient, especially a child, is usually held in an upright or seated position, often with parental assistance for immobilization.
Nasal Fossae Illumination: The nasal passages (nares) are adequately illuminated using a headlight or external light source to improve visualization.
Curved Hook Extraction: A specialized curved hook instrument (or similar angled instrument) is often used to:
Gently manipulate the foreign body.
Pull the foreign body forward and out of the nasal cavity.
An Eustachian catheter, a thin, curved catheter commonly used in ear procedures, can sometimes be adapted for use as a nasal hook in certain cases.
General Anesthesia (Uncooperative Patients): In cases involving:
Uncooperative patients, especially young children who are unable to remain still.
Deeply seated foreign bodies that are difficult to reach or remove with simple techniques.
General anesthesia may be necessary to ensure safe and atraumatic removal in a controlled setting.
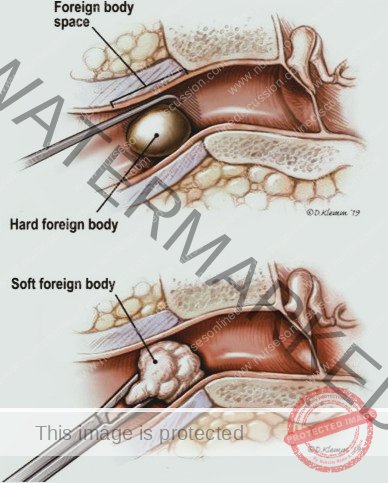
Specific Removal Techniques
Pre-Removal Preparation: Before attempting removal, the following may be helpful:
Decongest Nasal Mucosa: Apply a topical nasal decongestant, such as 0.5% phenylephrine (Neo-Synephrine) nasal spray, to:
Reduce swelling of the nasal lining (mucosa).
Improve visualization and access to the foreign body.
Provide Topical Anesthesia: Apply a topical anesthetic agent, such as lidocaine gel or spray, to:
Numb the area and reduce pain sensation during the removal procedure.
Direct Instrumentation: Utilize instruments for direct visualization and removal:
Direct Visualization and Removal: Use tools that allow direct visualization and grasping of the foreign body, including:
Fine forceps (e.g., alligator forceps, Hartmann forceps).
Small curved hooks or probes.
Cerumen loops (small wire loops).
Suction catheters, for suction-assisted removal of small, loose objects.
Balloon Catheter Method: Employ a balloon catheter technique for certain foreign bodies:
2. Balloon Catheter Technique:
* Pass Catheter Beyond Object: Carefully pass a thin, lubricated balloon-tip catheter gently past the foreign body within the nasal passage.
* Balloon Inflation: Inflate the balloon tip of the catheter distal to (behind) the foreign body.
* Forward Traction: Gently pull the catheter forward, using the inflated balloon to push the foreign body anteriorly and move it out through the nostril for removal.Self-Removal Encouragement: In cooperative patients, particularly older children or adults, encourage self-removal attempts using simple methods:
3. Blowing Nose Technique:
* Instruct Patient to Blow Nose: Instruct the patient to attempt to forcefully blow their nose to expel the foreign body.
* Nostril Occlusion: While blowing, instruct them to block the opposite nostril with a finger to increase pressure in the affected nostril.Positive Pressure Ventilation (Parent’s Kiss Technique): For uncooperative patients, particularly young children, and when direct instrumentation is challenging, positive pressure ventilation techniques can be considered:
4. Positive Pressure Ventilation:
* Caregiver Air Puff (Parent’s Kiss Technique): A caregiver (parent) can deliver a gentle puff of air into the child’s mouth while occluding the unaffected nostril. The sudden burst of air pressure may help dislodge the object and expel it from the affected nostril.
* Bag-Valve-Mask (Ambu Bag) Ventilation: Positive pressure ventilation can also be delivered more formally using a bag-valve-mask (Ambu bag) connected to the mouth and nose.
* Nasal Oxygen Tubing Ventilation: Positive pressure may also be delivered through the nose using oxygen tubing connected to an oxygen source, delivering a controlled puff of air.
Specific Foreign Body Considerations
Button Batteries – Emergency Removal: Button batteries lodged in the nose must be removed immediately due to the high risk of liquefaction necrosis (tissue death) caused by leakage of battery contents and electrical current.
Infection Control Precautions: When removing nasal foreign bodies, adhere to appropriate infection control precautions. Expect that the expelled foreign body will likely be:
* Expelled with force against the caregiver’s cheek or clothing.
* Covered in nasal mucus.
* Potentially contaminated with blood.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

